 One of the worst aspects of my rosacea, I feel, is the burning pain it gives me. My face most of the time feels tight, stinging, hot and like it has a sunburn. Even when my skin looks pink or leans towards pale, I still usually have that same burning tight uncomfortable feeling. And when a flush breaks through - which happens still often, for instance when I enter a warm room, or when I don't cool my face with a fan for a significant time, or from stress, or catching sunlight - , this burning pain gets worse and washes over the face. Some compare it with an acid sort of burning pain. It is hard, dealing with the burning hot pain daily.. I take one day at a time and try to stay cool and keep my face from flushing. So this burning pain, this nerve pain almost; what is it and what can be done about it? Recently (2011) scientists suggested a new subgroup of rosacea: neurogenic rosacea. A key characteristic of neurogenic Rosacea is the burning sensation and chronic facial pain it gives, both while the face is flushed or inflamed, but also in the absence of flushing and redness. It is something that is mostly seen with people who have subtype 1 rosacea, with redness of the face and flushing, and less so with subtype 2 patients with skin outbreaks and pimples (p&p's for rosacea). Constant flushing especially, but also inflammation of the skin and blood vessels, can cause the neurogenic onset, as it puts pressure on the small nerve endings in the face. And these nerve endings get hypersensitive and possibly even damaged from this. Inflammation of the trigeminal nerve, which is located in the facial skin, and helps create our facial sensations of pain, can also be affected and play a role in burning pain of the skin. Chronic inflammation can both affect existing nerves and nerve roots, and can make nerves hypersensitive. And long term nerve pain can not only make the area of skin that is painful bigger with time, but it can also create a nerve 'memory' for this pain, making it very hard to stop. The constant stimulation of the nerves in the facial skin from the pressure of dilated blood vessels and sometimes also from the edema -swelling- that rosacea flushing can give, sometimes leads to a condition called dysesthesia: an abnormal unpleasant sensation felt when the skin is touched, caused by damage to peripheral nerves. If the nerves are irritated, hyper-sensitive or damaged, it also can alter the way certain sensations, such as light, touch, and temperature, are felt. But there are also other ways in which the nerves in our face get sensitized more, for instance because organic chemicals like norepinephrine are released by an overactive central nervous system.
One of the worst aspects of my rosacea, I feel, is the burning pain it gives me. My face most of the time feels tight, stinging, hot and like it has a sunburn. Even when my skin looks pink or leans towards pale, I still usually have that same burning tight uncomfortable feeling. And when a flush breaks through - which happens still often, for instance when I enter a warm room, or when I don't cool my face with a fan for a significant time, or from stress, or catching sunlight - , this burning pain gets worse and washes over the face. Some compare it with an acid sort of burning pain. It is hard, dealing with the burning hot pain daily.. I take one day at a time and try to stay cool and keep my face from flushing. So this burning pain, this nerve pain almost; what is it and what can be done about it? Recently (2011) scientists suggested a new subgroup of rosacea: neurogenic rosacea. A key characteristic of neurogenic Rosacea is the burning sensation and chronic facial pain it gives, both while the face is flushed or inflamed, but also in the absence of flushing and redness. It is something that is mostly seen with people who have subtype 1 rosacea, with redness of the face and flushing, and less so with subtype 2 patients with skin outbreaks and pimples (p&p's for rosacea). Constant flushing especially, but also inflammation of the skin and blood vessels, can cause the neurogenic onset, as it puts pressure on the small nerve endings in the face. And these nerve endings get hypersensitive and possibly even damaged from this. Inflammation of the trigeminal nerve, which is located in the facial skin, and helps create our facial sensations of pain, can also be affected and play a role in burning pain of the skin. Chronic inflammation can both affect existing nerves and nerve roots, and can make nerves hypersensitive. And long term nerve pain can not only make the area of skin that is painful bigger with time, but it can also create a nerve 'memory' for this pain, making it very hard to stop. The constant stimulation of the nerves in the facial skin from the pressure of dilated blood vessels and sometimes also from the edema -swelling- that rosacea flushing can give, sometimes leads to a condition called dysesthesia: an abnormal unpleasant sensation felt when the skin is touched, caused by damage to peripheral nerves. If the nerves are irritated, hyper-sensitive or damaged, it also can alter the way certain sensations, such as light, touch, and temperature, are felt. But there are also other ways in which the nerves in our face get sensitized more, for instance because organic chemicals like norepinephrine are released by an overactive central nervous system.
Actually damaged nerves (think of damage after injury for instance), can sometimes also affect the way the skin looks: it can cause a change in color or texture, or making the skin more pale, red, purple or spotty, or looking thin and shiny. In my case; I used to flush and go red in the face without having the additional burning feeling. This was in the early days of my rosacea, around age 19-21. But now it only takes a little redness and blood vessel dilation to make the nerves of my face angry and for my face to feel on fire and with uncomfortable pain. Chronic sinus infections, the holes on both sides of the nose right under the most sensitive rosacea areas of the cheeks, can also fire up rosacea skin and nerve pain in the area. Think also of chronic nasal allergy symptoms here, which can inflame the sinus area. If you want to read how pain signals are exactly passing through our body to our brain, and how it all exactly works, scroll down; below I explain it in more detail. There is discussion by the way about whether or not rosacea inflammation comes first, and stimulates inflammation from the nerves, or if it could be the other way round, and if the systematic nervous system can inflame the nerves of the face - in a way in which auto-immune activity can create inflammation in all sorts of areas of the body when things go wrong - and that as a result of that, rosacea skin becomes painful and blood vessels start to dilate (in this interesting research paper, trigeminal nerves were found to be very effective at generation neurogenic inflammation). Chicken, or egg? Which came first and which was a secondary result? At this point we don't know for sure and it can be case dependent also, but uncontrolled rosacea has proven in trials to be causing trigeminal nerve pain. It is also possible that the nerves themselves become inflamed, in this entire inflammatory/ blood vessel dilating cycle. If the trigeminal nerves in the face become hypersensitive or inflamed (for instance as a result of poorly controlled rosacea inflammation of the skin), they can not only give off pain signs in the skin of the face, but also generate inflammation. That can negatively affect rosacea, but also increase the incidence of migraines and headaches for instance. Inflammation can even increase the risk of depression (which is recently linked to inflammation) and anxiety, and is also thought to be behind the increased risk of rosacea patients to develop dementia/ Alzheimer's disease...

In this small scale study, 14 patients with rosacea were tested. The majority of them were Caucasian females. They had what is called classic rosacea symptoms (burning and stinging, erythema, flushing, facial edema, telangiectasia, pruritus and papules) as well as neurological symptoms.
Researchers called these patients sufferers of a special rosacea subgroup: neurogenic rosacea. They suffer from redness of the skin and facial flushing, and some have visible blood vessels on the skin's surface, and they also suffer from stinging, burning and nerve pain of the skin, often even when their face isn't directly flushed or inflamed. They also have a higher risk of suffering from headaches and depressions, or OCD, tremors or complex regional pain syndrome. They emphasize that this subgroup of rosacea patients often has a hard time finding any treatment that really works. Because traditional rosacea treatments often do not work. Many of these trial patients had already tried more standard rosacea treatment options: topical metronidazole, topical steroids, and oral antibiotics with no or limited success. The researchers found that these patients had in fact more benefit from neurological treatment options, including gabapentin (5 of 11), duloxetine (4 of 6), pregabalin (1 of 4), tricyclic antidepressants (2 of 3) and memantine (2 of 2). Some of these patients also saw improvement from topical neurological treatments: Topically formulated neuroleptic agents including doxepin, glycopyrrolate, amitriptyline, capsaicin and ketamine, were effective in some cases (3 of 7). Hydroxychloroquine (3 of 5) and vasoactive agents including beta-blockers and alpha-1-adrenergic receptors (2 of 5) were also helpful in some patients. Photo below is taken from the research article it has the caption: "Facial erythema is seen in most patients at baseline and uniformly during flares. Inflammatory papules and pustules and rhinophymatous change are unusual in this subset of patients."

In this small scale study, 14 patients with rosacea were tested. The majority of them were Caucasian females. They had what is called classic rosacea symptoms (burning and stinging, erythema, flushing, facial edema, telangiectasia, pruritus and papules) as well as neurological symptoms.
"Within this group, 43% had neurologic symptoms and 50% had neuropsychiatric symptoms; these included complex regional pain syndrome, essential tremor, depression, and obsessive-compulsive disorder."
Researchers called these patients sufferers of a special rosacea subgroup: neurogenic rosacea. They suffer from redness of the skin and facial flushing, and some have visible blood vessels on the skin's surface, and they also suffer from stinging, burning and nerve pain of the skin, often even when their face isn't directly flushed or inflamed. They also have a higher risk of suffering from headaches and depressions, or OCD, tremors or complex regional pain syndrome. They emphasize that this subgroup of rosacea patients often has a hard time finding any treatment that really works. Because traditional rosacea treatments often do not work. Many of these trial patients had already tried more standard rosacea treatment options: topical metronidazole, topical steroids, and oral antibiotics with no or limited success. The researchers found that these patients had in fact more benefit from neurological treatment options, including gabapentin (5 of 11), duloxetine (4 of 6), pregabalin (1 of 4), tricyclic antidepressants (2 of 3) and memantine (2 of 2). Some of these patients also saw improvement from topical neurological treatments: Topically formulated neuroleptic agents including doxepin, glycopyrrolate, amitriptyline, capsaicin and ketamine, were effective in some cases (3 of 7). Hydroxychloroquine (3 of 5) and vasoactive agents including beta-blockers and alpha-1-adrenergic receptors (2 of 5) were also helpful in some patients. Photo below is taken from the research article it has the caption: "Facial erythema is seen in most patients at baseline and uniformly during flares. Inflammatory papules and pustules and rhinophymatous change are unusual in this subset of patients."
"Finally, patients with dysesthesia out of proportion to flushing or inflammation can be difficult to treat and require a unique approach first used to treat disorders such as complex regional pain syndrome and neuropathic itch. [..] Because of the associated heightened sensitivity to heat and sunlight, laser- and light-based interventions should be used with caution."
 Also check out this blog post I made about erythromelalgia; if explains the blurry line between rosacea flushing and burning, and Erythromelalgia (EM) flushing and burning, as well as the frustrating difficulty of treating its symptoms. A lot of meds and treatments mentioned in this blog post for the treatment of neuropathic pain, are also tried and sometimes tested as EM treatments. The more I read and try to write here about other flushing disorders, especially about erythromelalgia (EM), the more I start to think that this extreme face flushing and burning might not be strictly 'rosacea'. I feel there is a grey zone, where bad neurogenic/vascular rosacea falls into, as well as EM, as well as perhaps bad flushing from neuropathic pain disorders. The more I hear and read, the more it seems that it is extreme to flush this bad. And the few people I know who have it too, all seem to balance on the edge of different possible diagnosis. For instance, one of the derms I see thinks I have a mast cell disorder, hence the violent flushing. I also know a bad flusher who's doctor says she must have erythromelalgia. I joined an EM facebook group and there are many more people there with extreme face flushing and burning! More than in your average rosacea group. However they tend to also have burning hands and feet. My hands do burn but that has been diagnosed as Raynaud's syndrome in hospital. But the division lines are blurry and I might just as well have EM instead of straight forward rosacea. But... at the end of the day, they are labels and EM doctors also struggle to treat the facial burning and flushing, so we end up either way with a flushing problem that is hard to treat; both for dermatologists as well as for neurologists as well as for a rheumatologist, or a vascular specialist...
Also check out this blog post I made about erythromelalgia; if explains the blurry line between rosacea flushing and burning, and Erythromelalgia (EM) flushing and burning, as well as the frustrating difficulty of treating its symptoms. A lot of meds and treatments mentioned in this blog post for the treatment of neuropathic pain, are also tried and sometimes tested as EM treatments. The more I read and try to write here about other flushing disorders, especially about erythromelalgia (EM), the more I start to think that this extreme face flushing and burning might not be strictly 'rosacea'. I feel there is a grey zone, where bad neurogenic/vascular rosacea falls into, as well as EM, as well as perhaps bad flushing from neuropathic pain disorders. The more I hear and read, the more it seems that it is extreme to flush this bad. And the few people I know who have it too, all seem to balance on the edge of different possible diagnosis. For instance, one of the derms I see thinks I have a mast cell disorder, hence the violent flushing. I also know a bad flusher who's doctor says she must have erythromelalgia. I joined an EM facebook group and there are many more people there with extreme face flushing and burning! More than in your average rosacea group. However they tend to also have burning hands and feet. My hands do burn but that has been diagnosed as Raynaud's syndrome in hospital. But the division lines are blurry and I might just as well have EM instead of straight forward rosacea. But... at the end of the day, they are labels and EM doctors also struggle to treat the facial burning and flushing, so we end up either way with a flushing problem that is hard to treat; both for dermatologists as well as for neurologists as well as for a rheumatologist, or a vascular specialist... So, Scientists stress the problem of traditional rosacea treatment modalities not working well for neurogenic rosacea
So, Scientists stress the problem of traditional rosacea treatment modalities not working well for neurogenic rosaceaSo rounds of tetracycline antibiotics will most of the time do nothing for these burning and stinging symptoms. Instead, doctors should look in a different direction if they want to treat this condition, and try to calm the neurological pain instead. Scientists suggest neuroleptic agents, tricyclic antidepressants, and pain-modifying antidepressants. But another very important step in calming this burning pain of the skin down, is to control facial flushing first. Because it is the flushing and inflammation/redness that fires this problem on most of all. I have written an extensive blog post about the prescription medication that is available for the treatment of facial flushing, and after trying practically anything and everything to control my flushing (ranging from a host of rosacea and neurological medications, prescription creams, to acupuncture, homeopathy, herbal therapy, traditional Chinese medicine, diets, tea's.. I even got a healing crystal from my mother!). Some anti flushing medication that has a decent track record for rosacea subtype 1 are clonidine, propranolol (or another type of beta blockers, for instance carvedilol), certain antidepressants, antimalarial anti-inflammatory medication and also antihistamines. Antidepressants and clonidine are also tested and found effective for menopausal hot flashes, which are not exactly the same as rosacea flushing, but which go through some similar pathways and often are also effective to reduce flushing of the face. So getting your flushing under control is an important first step. There are many ways to try to achieve this; IPL or laser have also helped people with facial flushing and redness, there are natural anti-inflammatory supplements that sometimes help, and avoiding triggers and keeping your skin cool can also make a lot of difference. But medication like Plaquenil (hydroxychloroquine) or Mepacrine can also really help some people with rosacea redness (and burning and flushing sometimes too). They can reduce skin inflammation dramatically for some. Read more about my own trials with both meds in this blog post. Low dose Roaccutane is another treatment for rosacea, which can really alter the skin inflammation for the better, but it comes with potential side effects.
 If these adjustments aren't helping enough
If these adjustments aren't helping enougha proactive dermatologist or a neurologist, can look into specific medication that lowers the nerve pain we can feel in our faces and skin. There are a couple of first line meds that can be tried:
-Neurontin (gabapentin)
-Lyrica (pregabalin)
-Carbamazepine
-Tricyclic antidepressants (nortriptyline for instance, and amitriptyline)
-Pain-modifying antidepressants (e.g. duloxetine)
Then there are also other treatment options, which should be reserved for when the above do not work, the researchers stated: "N-methyl-D-aspartic acid receptor antagonists (eg memantine), systemic antibiotics, and other topically formulated medications (eg, ketamine, glycopyrrolate, capsaicin) may be helpful in certain cases. Because of the associated heightened sensitivity to heat and sunlight, laser- and light-based interventions should be used with caution." And the natural supplement PEA (Palmitoylethanolamide) is also tested and proven to be effective for neuropathic pain. More on that one at the bottom of this blog post.
 Usually when a dermatologist diagnoses you with rosacea, he or she will do this based on both the clinical symptoms you present (how your skin looks and feels, what your triggers are etc), as well as (ideally) ruling out other conditions that can give a red or flushed face. In this blog post I describe some other conditions that can cause facial flushing and redness. Ideally, a derm. rules out at the very least Lupus and Carcinoid Flushing. Both can be tested with blood tests (unlike rosacea). Depending on your triggers, a doctor can also test on allergies, mast cell disorders and hormone or thyroid disorders. I also had full immunology blood work done, which resulted in some indications for systemic autoimmune related inflammation issues in my body, but which were not conclusive of big issues. The same for my tests for lupus; I had them three times now over a ten year time span, and my ANA levels (one of the things they test you on; antinuclear antibodies) have been doubling since, now at 1:80, which indicated some autoimmune issues, but the level is not high enough to diagnose me with something like lupus. So, there is a good chance that your test results are either negative, or vaguely elevated. It is mostly important to have these tests, to not miss a blatant positive diagnosis of an autoimmune disease like lupus, or one of the other mentioned health conditions. But there are also neurological tests that can be done, in the search of a solid diagnosis, for instance MRI/CT testing, X-rays or lumbar punctures, to look for serious infections of central Nervous System conditions. In reality, VERY few rosacea patients get one or two of these tests, let alone all of them. You have to be blessed with a wonderful proactive dermatologist or general practitioner, or be very loud about what you want from the medical community. And then there is always the issue of costs. Even in this part of the world, with wonderful (but expensive) health insurance, doctors are hesitant to spend too much money and time on diagnostic testing of illnesses that they do not already suspect you might suffer from.
Usually when a dermatologist diagnoses you with rosacea, he or she will do this based on both the clinical symptoms you present (how your skin looks and feels, what your triggers are etc), as well as (ideally) ruling out other conditions that can give a red or flushed face. In this blog post I describe some other conditions that can cause facial flushing and redness. Ideally, a derm. rules out at the very least Lupus and Carcinoid Flushing. Both can be tested with blood tests (unlike rosacea). Depending on your triggers, a doctor can also test on allergies, mast cell disorders and hormone or thyroid disorders. I also had full immunology blood work done, which resulted in some indications for systemic autoimmune related inflammation issues in my body, but which were not conclusive of big issues. The same for my tests for lupus; I had them three times now over a ten year time span, and my ANA levels (one of the things they test you on; antinuclear antibodies) have been doubling since, now at 1:80, which indicated some autoimmune issues, but the level is not high enough to diagnose me with something like lupus. So, there is a good chance that your test results are either negative, or vaguely elevated. It is mostly important to have these tests, to not miss a blatant positive diagnosis of an autoimmune disease like lupus, or one of the other mentioned health conditions. But there are also neurological tests that can be done, in the search of a solid diagnosis, for instance MRI/CT testing, X-rays or lumbar punctures, to look for serious infections of central Nervous System conditions. In reality, VERY few rosacea patients get one or two of these tests, let alone all of them. You have to be blessed with a wonderful proactive dermatologist or general practitioner, or be very loud about what you want from the medical community. And then there is always the issue of costs. Even in this part of the world, with wonderful (but expensive) health insurance, doctors are hesitant to spend too much money and time on diagnostic testing of illnesses that they do not already suspect you might suffer from. Neurontin and Lyrica are brand names, their generic names are gabapentin and pregabalin and are fine as well to use instead (and cheaper). Both medications are 'neuromodulators' (changing nerve activity - like botox by the way; a messenger released from a neuron that affects the transmission of the signals between neurons). They quiet pain signals from your nerve cells and change the way in which your body senses nerve pain. Both are nerve calming meds, tackling pain signals in your brain and nervous system. They stabilize the electrical activity in your brain, and affect the way your nerves send messages to your brain. More specifically, Neurontin and Lyrica, but also carbamazepine for instance, cut down transmissions of ectopic nerve impulses and independent nerve firing, caused by damaged nerves. They also alter sympathetic feedback loops and microneruomas at damaged nerve sites. These type of medication also block sodium channels (which helps lower nerve pain), enable GABA reuptake inhibition, Non-NMDA glutamate receptor blocking, GABA synthesis, and GABA sub-receptor stimulation. Note that both meds take a while to build up in your system and start working. Multiple weeks or sometimes a month+ for users.
Neurontin and Lyrica are brand names, their generic names are gabapentin and pregabalin and are fine as well to use instead (and cheaper). Both medications are 'neuromodulators' (changing nerve activity - like botox by the way; a messenger released from a neuron that affects the transmission of the signals between neurons). They quiet pain signals from your nerve cells and change the way in which your body senses nerve pain. Both are nerve calming meds, tackling pain signals in your brain and nervous system. They stabilize the electrical activity in your brain, and affect the way your nerves send messages to your brain. More specifically, Neurontin and Lyrica, but also carbamazepine for instance, cut down transmissions of ectopic nerve impulses and independent nerve firing, caused by damaged nerves. They also alter sympathetic feedback loops and microneruomas at damaged nerve sites. These type of medication also block sodium channels (which helps lower nerve pain), enable GABA reuptake inhibition, Non-NMDA glutamate receptor blocking, GABA synthesis, and GABA sub-receptor stimulation. Note that both meds take a while to build up in your system and start working. Multiple weeks or sometimes a month+ for users.
Neurontin (gabapentin) is a widely used medication to treat neuropathic pain, but also hot flashes and restless legs syndrome. It is one of the very first medications which doctors/neurologists often prescribe for the treatment of neuropathic (nerve) pain. Think for instance of nerve pain caused by diabetic neuropathy, postherpetic neuralgia, or central neuropathic pain. But rosacea can also cause the nerves in the skin of the face to become hyper reactive and painful, especially when a person flushes a lot and has red skin with a lot of inflammation of the blood vessels. In research, Neurontin (gabapentin) was found to reduce hot flushes in test persons. However, a common* side effect of gabapentin/Neurontin is high blood pressure, flushing or dilation of blood vessels..(*Common; may affect up to 1 in 10 people - See information leaflet of this medication). This does not mean you will get it if you try gabapentin/Neurontin. But it means there is a risk for these side-effects to occur (sometimes also temporarily, only at the start of treatment).
Lyrica (pregabalin) is also a medication used to treat neuropathic (nerve) pain, fibromyalgia, and generalized anxiety disorder. It was developed after Neurontin. Where Neurontin was originally also designated as a treatment for epilepsy, Lyrica on the other hand is specifically approved for use in diabetic neuropathic pain, and in 2007 was also approved for use in fibromyalgia. Unfortunately 'flushing' and 'hot flashes' are mentioned as a possible side effect for Lyrica. It is estimated to be a less common side effect for Lyrica/pregabalin than it is for gabapentin/Neurontin however, and is listed as "Uncommon (0.1% to 1%)". Which does not mean you need to flush from it, but it is possible... And strangely enough, in research Lyrica (pregabalin) was found to reduce hot flushes in test persons. Here is another positive test result. Acclaimed forum poster Laser_cat also suggested interestingly another reason why Lyrica (and Neurontin by default) can make the face hotter: "I think any membrane stabilizer has the potential to increase heat in the face (adrenergic nerves might be stabilized too, which would otherwise be releasing norepinephrine to constrict the blood vessels)." In this medical article, it is reported that neurogenic rosacea symptoms including swelling and redness responding to lyrica. However, Lyrica is a strong anti-nerve pain medication and there are many people with rosacea burning who have taken or are taken it with success.. Like with Neurontin, it works by decreasing the number of pain signals that are sent out by damaged nerves in the body. It offers similar efficiency at treating nerve pain with Neurontin, and also the same as the antidepressant amitriptyline, which will be discussed below. All three meds showed clinical effect in trials, but most professionals keep Lyrica as a last resort; for when Neurontin and amitriptyline do not (sufficiently) work. But it can depend entirely on each individual pain patient which of the three medications works better for them. As stated above, with both Neurontin and Lyrica it may take several weeks before you notice the nerve pain reducing effects. Dosis should be discussed with your doctor. One doses that is mentioned more often to be effective for neurogenic pain is 150 mg pregabalin, twice daily.
 Carbamazepine (Tegretol) is a neuromodulator too, and I used that drug for a period of time as well. I stopped it when I got more flushed and red and hot on it. Carbamazepine is more effective for a specific type of nerve pain; trigeminal neuralgia. Tiagabine, Gabapentin and Lyrica are more effective with a broader range of neuropathic pain disorders. They also tend to have a lower side effect profile. They can help to eliminate burning, abnormal, piercing and electrical types of pain. My pharmacist said about Carbamazepine that it shouldn't induce vasodilatation, flushing or hot flash as a side-effect, but that it acts an an anticholinergic, working on the central nerve system and that it can therefore cause drowsiness, as well as increased blood flow to the face. Other anticholinergic side effects that can work against us flushers, is that they decrease sweating (dry skin = often more red skin), and can increase body temperature. They can also cause red skin in some cases. You can also read about my own experience with carbamazepine in this blog post. I only used it short term and felt it made my skin more red, so stopped again... Not a good trial period, by all means, so my verdict should not count at this point I feel. I wrote about it on December 2006, after finding that Neurontin made me flush too much:
Carbamazepine (Tegretol) is a neuromodulator too, and I used that drug for a period of time as well. I stopped it when I got more flushed and red and hot on it. Carbamazepine is more effective for a specific type of nerve pain; trigeminal neuralgia. Tiagabine, Gabapentin and Lyrica are more effective with a broader range of neuropathic pain disorders. They also tend to have a lower side effect profile. They can help to eliminate burning, abnormal, piercing and electrical types of pain. My pharmacist said about Carbamazepine that it shouldn't induce vasodilatation, flushing or hot flash as a side-effect, but that it acts an an anticholinergic, working on the central nerve system and that it can therefore cause drowsiness, as well as increased blood flow to the face. Other anticholinergic side effects that can work against us flushers, is that they decrease sweating (dry skin = often more red skin), and can increase body temperature. They can also cause red skin in some cases. You can also read about my own experience with carbamazepine in this blog post. I only used it short term and felt it made my skin more red, so stopped again... Not a good trial period, by all means, so my verdict should not count at this point I feel. I wrote about it on December 2006, after finding that Neurontin made me flush too much:
 Side effects of these medications are generally mild, but may include nausea, dizziness or drowsiness. Both antidepressants and anti-seizure medications like Neurontin and Lyrica can also in rare cases worsen depression or cause suicidal thoughts; usually at the start of treatment and temporarily. Doctors often let you build these types of medication up slowly to reduce side effect risks. If they make you drowsy, take them before bedtime. Both Neurontin/gabapentin and Lyrica/pregabalin have been tested for efficiency for both rosacea and hot flashes. In this research, scientists concluded:
Side effects of these medications are generally mild, but may include nausea, dizziness or drowsiness. Both antidepressants and anti-seizure medications like Neurontin and Lyrica can also in rare cases worsen depression or cause suicidal thoughts; usually at the start of treatment and temporarily. Doctors often let you build these types of medication up slowly to reduce side effect risks. If they make you drowsy, take them before bedtime. Both Neurontin/gabapentin and Lyrica/pregabalin have been tested for efficiency for both rosacea and hot flashes. In this research, scientists concluded:
And in this pubmed research, 420 women with hot flashes (which are comparable in essence in some ways to face flushing, also in shared treatment efficiency) were treated with gabapentin. Those treated with the highest dose of 900 mg a day of gabapentin showed a significant reduction in hot flashes. Those treated with a placebo or a lower dose of 300 mg/day gabapentin showed no such improvement. However a subsequent study showed that gabapentin at a lower dose of 300 mg/day did show moderate improvement of hot flashes in their test persons. In this pubmed research pregabalin (Lyrica) was found effective as a treatment for hot flashes. Please scroll down in this article to read reviews and posts from rosaceans about their experience with gabapentin (Neurontin) and pregabalin (Lyrica)!
Lyrica (pregabalin) is also a medication used to treat neuropathic (nerve) pain, fibromyalgia, and generalized anxiety disorder. It was developed after Neurontin. Where Neurontin was originally also designated as a treatment for epilepsy, Lyrica on the other hand is specifically approved for use in diabetic neuropathic pain, and in 2007 was also approved for use in fibromyalgia. Unfortunately 'flushing' and 'hot flashes' are mentioned as a possible side effect for Lyrica. It is estimated to be a less common side effect for Lyrica/pregabalin than it is for gabapentin/Neurontin however, and is listed as "Uncommon (0.1% to 1%)". Which does not mean you need to flush from it, but it is possible... And strangely enough, in research Lyrica (pregabalin) was found to reduce hot flushes in test persons. Here is another positive test result. Acclaimed forum poster Laser_cat also suggested interestingly another reason why Lyrica (and Neurontin by default) can make the face hotter: "I think any membrane stabilizer has the potential to increase heat in the face (adrenergic nerves might be stabilized too, which would otherwise be releasing norepinephrine to constrict the blood vessels)." In this medical article, it is reported that neurogenic rosacea symptoms including swelling and redness responding to lyrica. However, Lyrica is a strong anti-nerve pain medication and there are many people with rosacea burning who have taken or are taken it with success.. Like with Neurontin, it works by decreasing the number of pain signals that are sent out by damaged nerves in the body. It offers similar efficiency at treating nerve pain with Neurontin, and also the same as the antidepressant amitriptyline, which will be discussed below. All three meds showed clinical effect in trials, but most professionals keep Lyrica as a last resort; for when Neurontin and amitriptyline do not (sufficiently) work. But it can depend entirely on each individual pain patient which of the three medications works better for them. As stated above, with both Neurontin and Lyrica it may take several weeks before you notice the nerve pain reducing effects. Dosis should be discussed with your doctor. One doses that is mentioned more often to be effective for neurogenic pain is 150 mg pregabalin, twice daily.
 Carbamazepine (Tegretol) is a neuromodulator too, and I used that drug for a period of time as well. I stopped it when I got more flushed and red and hot on it. Carbamazepine is more effective for a specific type of nerve pain; trigeminal neuralgia. Tiagabine, Gabapentin and Lyrica are more effective with a broader range of neuropathic pain disorders. They also tend to have a lower side effect profile. They can help to eliminate burning, abnormal, piercing and electrical types of pain. My pharmacist said about Carbamazepine that it shouldn't induce vasodilatation, flushing or hot flash as a side-effect, but that it acts an an anticholinergic, working on the central nerve system and that it can therefore cause drowsiness, as well as increased blood flow to the face. Other anticholinergic side effects that can work against us flushers, is that they decrease sweating (dry skin = often more red skin), and can increase body temperature. They can also cause red skin in some cases. You can also read about my own experience with carbamazepine in this blog post. I only used it short term and felt it made my skin more red, so stopped again... Not a good trial period, by all means, so my verdict should not count at this point I feel. I wrote about it on December 2006, after finding that Neurontin made me flush too much:
Carbamazepine (Tegretol) is a neuromodulator too, and I used that drug for a period of time as well. I stopped it when I got more flushed and red and hot on it. Carbamazepine is more effective for a specific type of nerve pain; trigeminal neuralgia. Tiagabine, Gabapentin and Lyrica are more effective with a broader range of neuropathic pain disorders. They also tend to have a lower side effect profile. They can help to eliminate burning, abnormal, piercing and electrical types of pain. My pharmacist said about Carbamazepine that it shouldn't induce vasodilatation, flushing or hot flash as a side-effect, but that it acts an an anticholinergic, working on the central nerve system and that it can therefore cause drowsiness, as well as increased blood flow to the face. Other anticholinergic side effects that can work against us flushers, is that they decrease sweating (dry skin = often more red skin), and can increase body temperature. They can also cause red skin in some cases. You can also read about my own experience with carbamazepine in this blog post. I only used it short term and felt it made my skin more red, so stopped again... Not a good trial period, by all means, so my verdict should not count at this point I feel. I wrote about it on December 2006, after finding that Neurontin made me flush too much:
"So I'll start trying another painkiller by Monday; Tegretol (carbamazepine). Carbamazepine doesn't have vasodilatation, flushing, hot flashes or anything mentioned as side-effect. Flushing is mentioned with all the tricyclics, and my pharmacist explained that these drugs can widen the little blood vessels in the face; modern SSRI antidepressant (which give facial flushing as well often), anticonvulsants like Carbamazepine, phenytoin, gabapentin (or Lyrica) and lamotrigine and eventually certain antiarrhythmics, such as lidocaine and mexiletine. Also there are opioids, but they can cause facial flushing AS WELL (SIGHT................). So for anyone else I would bet on either gabapentin, which is registered as helpful for menopausal hot flashes as well (does something with the calcium channels and regulates body temperature, which is promising for us), or the carbamazepine, which I will try myself by next week, so I'll update on that one as well. Then there is Trileptal (oxcarbazepine), which is a derivative from carbamazepine (Tegretol), like Lyrica from neurontin, but Trileptal has a high incidence of facial acne and depression, and I rather give the Tegretol a fair chance first. Besides: Tegretol has a proven track for the treatment of neuropathic pain and Trileptal has still studies running for this." [...] "On Sunday I took 75 mg of carbamazepine. My skin was pink by then. At night I had a bad flushing attack however. Maybe I ate too many white beans! When I woke up my right cheek was burning and pretty red. And my left cheek was red and swollen too. I don't know now if the carbamazepine is helping, or making me more flushed than normal."
 Side effects of these medications are generally mild, but may include nausea, dizziness or drowsiness. Both antidepressants and anti-seizure medications like Neurontin and Lyrica can also in rare cases worsen depression or cause suicidal thoughts; usually at the start of treatment and temporarily. Doctors often let you build these types of medication up slowly to reduce side effect risks. If they make you drowsy, take them before bedtime. Both Neurontin/gabapentin and Lyrica/pregabalin have been tested for efficiency for both rosacea and hot flashes. In this research, scientists concluded:
Side effects of these medications are generally mild, but may include nausea, dizziness or drowsiness. Both antidepressants and anti-seizure medications like Neurontin and Lyrica can also in rare cases worsen depression or cause suicidal thoughts; usually at the start of treatment and temporarily. Doctors often let you build these types of medication up slowly to reduce side effect risks. If they make you drowsy, take them before bedtime. Both Neurontin/gabapentin and Lyrica/pregabalin have been tested for efficiency for both rosacea and hot flashes. In this research, scientists concluded:
"The patient could not tolerate gabapentin, but within 2 months of starting pregabalin, her symptoms improved dramatically, with a reduction in facial burning sensation, redness and swelling. She is currently being maintained on pregabalin 300 mg in the morning and 225 mg at night."
And in this pubmed research, 420 women with hot flashes (which are comparable in essence in some ways to face flushing, also in shared treatment efficiency) were treated with gabapentin. Those treated with the highest dose of 900 mg a day of gabapentin showed a significant reduction in hot flashes. Those treated with a placebo or a lower dose of 300 mg/day gabapentin showed no such improvement. However a subsequent study showed that gabapentin at a lower dose of 300 mg/day did show moderate improvement of hot flashes in their test persons. In this pubmed research pregabalin (Lyrica) was found effective as a treatment for hot flashes. Please scroll down in this article to read reviews and posts from rosaceans about their experience with gabapentin (Neurontin) and pregabalin (Lyrica)!
Neurontin especially seemed to help my rosacea for a couple of weeks, until I started to get more flushed from it. Mind you, I have really unstable reactive blood vessels and flush from practically half the things life has to offer lol, but when I discussed it with my doctor at the time, he said that in rare cases, neurontin can give vasodilation (blood vessel dilation) as a side effect. Both seemed to make my face feel more hot as well.. I have read a lot of positive rosacea user reviews for both Neurontin and Lyrica however. I used both meds back in 2006, after I fell asleep on a (frozen) gelpack on holiday in Ireland. I had been flushed and my face was burning when I stayed over with friends there, and half sleep-drunk fetched a gelpack which I had stored in their freezer. Mine at home never made the gel packs rock solid hard frozen, but this one did. I intended to just cool my face for a few minutes and then put the packs away again, but instead I fell back to sleep, while resting one cheek on the cold pack.. It was wrapped in a t-shirt, but the cold came through nevertheless and I ended up with frostbite on one cheek and very piercing nerve pain, which lasted half a year! The neurologist pain specialist I saw at the time for this, had predicted this time frame from the get go. He explained that nerves take a long time to recover and resettle. That I had to expect 6 months, but at the same time that if things hadn't recovered by then, there was a slim chance that they ever would normalize! It was a nervous time, and I tried several types and brand of nerve pain medication in my quest to stop the nerve pain without blowing up my rosacea flushing. My neurologist put me on neurontin first and Lyrica later. My experience with neurontin was that it did numb the nerve pain, and that initially I felt also less flushed and red on it, but this changed after a week or so, maybe two weeks, when I started to notice that I had more background redness all over my face, and that I would flush more often and longer than normal too. Went back and discussed it, and one of neurontins side-effects turned out to be vasodilatation. This is rare and I reckon it can only be a problem for people who have really reactive blood vessels. But I stopped using it after about 4 weeks for this reason. You can read more about this in this blog post.*Below, at the end of this post, I will copy my blog entries from 2006, where I detail my trial with neurontin.
 More about Lyrica
More about LyricaIn 2015, a scientific publication called "Neurogenic rosacea: an uncommon and poorly recognized entity". It read (and I put some clarifications of terminology between brackets now and then): "We present a case of neurogenic rosacea, a distinct variant of rosacea that has only recently been described, and which we feel is probably under-recognized. A 61-year-old woman presented with flushing, facial redness and burning. She had been diagnosed with rosacea in her early 20s, and it was thought that this presentation was simply an exacerbation. The patient was otherwise fit and well, and was treated with a prolonged course of lymecycline 408 mg daily and topical applications including metronidazole gel and azelaic acid. The patient became increasingly distressed as the erythema (red skin), oedema (swelling) and burning sensation gradually developed over her cheeks, and reported suicidal tendencies. She was taking mirtazapine and saw a community psychiatric nurse for weekly for psychological therapies. Investigations for lupus, porphyria, carcinoid and pheochromocytoma were negative. The patient had carried out internet searches for possible cures, and was ready to consider sympathectomy (a cutting of the sympathetic nerve, for instance done in ETS surgery). She underwent a course of intense pulsed light (IPL) treatment for the facial redness, which was partially effective. We also tried the patient on clonidine and beta-blockers for the flushing without any benefit. Given the additional severe facial burning sensation and oedema, and failure to respond to standard treatments, the condition was diagnosed as neurogenic rosacea. The patient could not tolerate gabapentin (Neurontin), but within 2 months of starting pregabalin (Lyrica), her symptoms improved dramatically, with a reduction in facial burning sensation, redness and swelling. She is currently being maintained on pregabalin 300 mg in the morning and 225 mg at night.
Amitriptyline is a tricyclic antidepressant and is often used to treat chronic neuropathic (nerve) pain, especially pain due to nerve damage but also for fibromyalgia pain. It is recommended as a first line treatment for nerve pain (it is considered most effective in combination with acceptable side effect profiles) and in a dose that is lower than the dose at which it is normally prescribed to treat depression. But in the medical article "Neurogenic Rosacea: A Distinct Clinical Subtype Requiring a Modified Approach to Treatment", amitriptyline is mentioned as a treatment option for neurogenic rosacea with only limited success. It has been used in a 15% cream formulation in the mentioned research, as well as when taken orally. Amitriptyline and nortriptyline act as anticholinergics, working on the central nerve system and can cause drowsiness, as well as increased blood flow to the face. Other anticholinergic side effects that can work against us flushers, is that they decrease sweating (dry skin = often more red skin), and can increase body temperature. They can also cause red skin in some cases. Dose should be discussed with your doctor. One doses that is mentioned more often to be effective for neurogenic pain is 80 mg amitriptyline, once daily (taken at night). I tried amitriptyline in the dreaded year 2005, when I had severe flushing after a botched IPL treatment. I was flushing a lot so it was very hard to pinpoint whether or not this drug helped me, but I felt it made me more flushed at the time. And it did not help me with my nerve pain. But, I was flushed so much that no pain med would probably have really helped, short of a horse drug like opium or something. I wrote about it at the time on the Rosacea Forum.
 I wrote on 14th August 2005: "Hi all, I’m having a bad time lately (again) with very uncontrollable and painful flushing. The doc. prescribed me an anti-depressant named Amitriptyline, that is used for nerve pains in small doses. Side-effects can be hypertension and it can effect medicines like clonidine and moxonidine. I wonder if anybody is familiar with this drug and has good or bad experiences with it? I can tell all I want about rosacea but usually docs don’t really listen to me and give the med anyway. A while ago I had an colon examination for example and they gave me morphine, of all drugs. Even though I almost refused to take it (flushing!!). Intravenous and it gave me the most horrible flushing ever. Like to avoid this if possible next times… Thanks, Nat"
I wrote on 14th August 2005: "Hi all, I’m having a bad time lately (again) with very uncontrollable and painful flushing. The doc. prescribed me an anti-depressant named Amitriptyline, that is used for nerve pains in small doses. Side-effects can be hypertension and it can effect medicines like clonidine and moxonidine. I wonder if anybody is familiar with this drug and has good or bad experiences with it? I can tell all I want about rosacea but usually docs don’t really listen to me and give the med anyway. A while ago I had an colon examination for example and they gave me morphine, of all drugs. Even though I almost refused to take it (flushing!!). Intravenous and it gave me the most horrible flushing ever. Like to avoid this if possible next times… Thanks, Nat"Keisha06 replied on 14th August 2005: "Hi Nat, my doctor prescribed this when my Rosacea first came out (really bad flushing) but he prescribed it to help me sleep because I kept waking up at about 2:00 a.m. and couldn't go back to sleep (was just flushing, and flushing and flushing). As I understand it is an older style antidepressant and quite a bit can be taken (he started me off at 5 mg but said I could take up to 70 mg - I think I ended up taking about 60 mg a night for a week to break the sleep cycle problem, then tapered down and off it. If anything it helped my Rosacea as I was getting more sleep, it certainly didn't adversely affect it. One effect I did notice is it tends to make you sleep longer and you can be a little tired in the morning (but I was taking it at night)."
I replied on 15th August 2005: "Thanks Diana, so no extra flushing and night sweats etc? Might give it a try myself! Nat"
Mermaid replied on 15th August 2005: "Hello Nat, I truly hope that you are feeling better and looking forward to your IPL treatments at the end of the year. I think it will make things so much easier and it really frustrates me that you have to go through all of this pain. I am assuming that you will be taking the Amitriptyline in an oral form. The reason I ask is that Dr Nase mentioned a little while ago that 2% Amitriptyline in an emollient cream base for sensitive skin (not PLO base), in which clinical studies showed that it could relieve neural burning and pain sensations. Dr Nase also mentioned 6% Gabapentin in an emollient cream base for sensitive skin (not PLO base) and 2% Clonidine in an emollient cream base for sensitive skin (not PLO base). I was wondering if Dr Nase could comment on this when he has the time or some other informed member. Good luck Nat."
Mollie_T replied on 29th March 2006: "My family doctor prescribed amitriptyline 50mg as a sleep aid, and I began using Metrogel 1% yesterday. I haven't noticed any change in my flushing yet- but I'm not a really big flusher anyway."
And in this PDF file, the same is mentioned:
 Duloxetine (Cymbalta); pain-modifying antidepressants
Duloxetine (Cymbalta); pain-modifying antidepressantsIn 2008 Duloxetine became the second drug approved by the FDA to treat fibromyalgia. It is used to treat treat depression and generalized anxiety disorder, but duloxetine is also used to treat diabetic neuropathy. It belongs to a class of medications called selective serotonin and norepinephrine reuptake inhibitors (SNRIs). Some user reviews form The Rosacea Forum:
Y-gwair wrote on April 10th 2012: "I tried Duloxetine a week ago with disastrous results. Within 48 hours I developed terrible flushing in my face, and also in my tongue and palate, as if I'd eaten a mouthful of chili, and had to stop. Over the next 48 hours, I had terrible withdrawal symptoms, my hands, feet and tongue went into Raynaud's like vasospasm as the circulation cut off completely, so painful I couldn't walk and my tongue went numb and lost all sense of taste. My hands have become so painful it's virtually impossible to use my laptop because of the freezing metal casing. [..] For some, Serotonin can be a powerful vasodilator and such drugs can potentially cause disturbance to the sympathetic nervous system with disastrous results."
G24 wrote on June 16th 2005: "Hello all, What's the best med/otc product for neural burning in the face? Thanks, G24"
Cactus responded on June 17th 2005: "Hi, I would have to recommend Cymbalta. It is not an otc product, however. It is actually an antidepressant but is supposed to help with neural burning. I can vouch for that - I have been on it a short time and already noticed the burning is more a sensation of warmth instead of the intense burning I used to have. However, I don't look any less red, just feel less on fire. [..] I believe it is also used for diabetics with neuropathic pain."
Jmb212121 wrote on December 1st 2007: "Cymbalta will help burning - I just started this topic to let you all know that Cymbalta will help with burning sensations. It has also really helped with my mood also and help me get off the rosacea mind set so to speak."
Laser_cat wrote on September 11th, 2018: "I have tried effexor and cymbalta each - for me the norepinephrine reuptake inhibition for both facilitates some vasoconstriction. If I wasn't on an SNRI I would be flushing/burning 24/7 and wouldn't be able to sit down. The effexor is more like an SSRI at doses under 150 mg so I wouldn't give up if it doesn't work for you in the beginning at lower doses. The vasoconstriction might be a little more noticeable with the effexor than the cymbalta but not much (maybe why effexor is more known to have high bp as a side effect ..). My experience is that cymbalta helps more with nerve pain. There is a paper out there that says that cymbalta at 60 mg can block sodium channels (like amitriptyline or lidocaine) and maybe this is why (sodium channels might be instrumental in pain transmission .. people with sodium channel loss-of-function mutations have an inability to sense pain .. people with gain-of-function sodium channel mutations have lower thresholds in sensing heat + pain both .. ). My doc said that she will give 120 mg+ on cymbalta for nerve pain though. I am on 80 mg cymbalta and do well. [..] I am also on mirtazapine 22.5 mg -- and I think by being an alpha 2 adrenoceptor blocker, it might help with some subtle vasoconstriction (I notice if I miss a day) but imo not as much as the SNRI's."
In tests the SSRI-type antidepressants turned out to be less effective at treating painful diabetic neuropathy than antidepressants which affect both serotonin and norepinephrine in the brain. These drugs are great for the treatment of depression, but are not very effective for neuropathic pain.
Please scroll down in this post to read why exactly antidepressants like Cymbalta (and other types) can reduce nerve pain.
 Other meds that can help with nerve pain are:
Other meds that can help with nerve pain are: -Other anticonvulsant medications; phenytoin, carbamazepine, valproic acid and clonazepam
-The epilepsy drug Trileptal (oxcarbazepine)
-Antiarrhythmics like mexiletine. In this article is detailed how mexiletine quiets the sensory nerves and neurogenic pain (which in turn can quiet down pain-triggered flushing)."An increase in the dose to 200 mg 3 times a day was attempted resulting in a dramatic improvement in pain and redness of his ears."
-SSRI antidepressants like Fluoxetine (Prozac), Paroxetine (Paxil) and Venlafaxine (Effexor)
-Systemic local anesthetics including lidocaine, tocainide
-Muscle relaxants like Baclofen or diazepam
-Memantine
-Ranolazine
-Daily aspirin (if aspirin / salicylates don't make you flushed)
-Topical capsaicin cream (Zostrix, 0.025% and 0.075%) or Baclofen
Topical 0.5% amitriptyline has also been used to treat neuropathic pain. Be weary of potential blood vessel dilation from that one.
-Ketamine
-The supplement Alpha Lipoic Acid: "Studies also found that alpha-lipoic acid supplements can help with neuropathy -- nerve damage -- caused by diabetes or cancer treatment. They seem to reduce symptoms like pain, tingling, and prickling in the feet and legs."
-Magnesium supplements can help but magnesium can also dilate blood vessels and heighten nitric oxide in the system, which is also a blood vessel dilator and potential rosacea worsener. But of magnesium doesn't flare your rosacea and does help your nerve pain, then consider also a prescription low dose (long-acting) calcium channel blocker, which can work even better. (Again; warning as they are blood vessel dilators too).
-CBD oil (Cannabidiol): Read this info on the possible help of CBD oil for nerve pain.
-Butterbur, feverfew, ginger -- "natural" migraine remedies
-Botox (see this blog post on botox for rosacea)
-Intravenous Immunoglobulin (IVIG) for Resistant Neuropathic Pain
-Infusions (lidocaine, ketamine, etc) can interrupt the 24/7 neuropathic pain cycle. They can be followed with mexiletine (oral lidocaine analog) for longer analgesic effects.
-Nerve blocks (see dedicated paragraph further down in this blog post. Nerve blocks are not permanent, but can be very helpful in conditions like CRPS/hot flashes/depression/etc particularly if the pain is sympathetically mediated
-Acupuncture
-Tapentadol; A new medication for nerve pain. Tapentadol is a new opioid for neuropathic pain that is as strong as oxycodone, but has less of its side-effects, especially less nausea and vomiting. It also blocks the reuptake of noradrenaline in the brain.
 A general practitioner or a dermatologist can prescribe nerve pain medication, as well as anti flushing medication. However, if none of them are effective, it can be worthwhile asking a referral to a specialist pain management doctor or neurologist. In my home town hospital there is a pain clinic especially for nerve pain treatment and under one of their doctors, I was able to try out medications like neurontin, lyrica and carbamazepine. It are these pain specialists who can ultimately go the next step in some cases, and offer the options of nerve blocks (stellate ganglion, trigeminal), botox, lidocaine infusions, ketamine infusions and IVIGs. It can be difficult however to first get a referral (rosacea is still seen by many as a primarily 'cosmetic' issue, and many doctors do not realize how much burning pain it can give us), and then it can be difficult also to convince a pain specialist to go as far as nerve blocks. But just know that these options are available. Ideally your dermatologist should work together with a pain specialist, when you deal with nerve pain on top of your rosacea inflammation and/or flushing. Sometimes combining two antidepressants (an SSRI with Cymbalta for instance) for nerve pain gives a better result than taking just one. Blood vessel constricting medication (clonidine, beta-blockers like propranolol) can sometimes be added to nerve pain blocking medication, to stabilize the blood vessels, and reduce flushing-triggered nerve pain. Anti-inflammatory medication (plaquenil for instance, or for those who benefit from antibiotics, low dose or regular dose tetracycline antibiotics can also help) can also be added to help reduce inflammation-mediated nerve pain. Please note that opioids, anti-inflammatories, and anticonvulsants have limited effects and tolerability in the treatment of neuropathic pain..(i.e., limited efficacy, safety and tolerability issues). Regarding the use of antidepressants to treat neuropathic pain, there have been numerous studies demonstrating the pain reducing effects of antidepressants. Data is strong regarding the pain-inhibiting effects of tricyclic antidepressants (TCA) and newer agents enhancing norepinephrine and serotonin neurotransmission. In contrast, review of studies with selective serotonin reuptake inhibitors (SSRIs) show poorer or inconsistent evidence of efficacy for migraine or tension headaches, diabetic neuropathy, and fibromyalgia. Several studies of SSRI treatment for mixed-chronic pain on the other hand are universally positive.
A general practitioner or a dermatologist can prescribe nerve pain medication, as well as anti flushing medication. However, if none of them are effective, it can be worthwhile asking a referral to a specialist pain management doctor or neurologist. In my home town hospital there is a pain clinic especially for nerve pain treatment and under one of their doctors, I was able to try out medications like neurontin, lyrica and carbamazepine. It are these pain specialists who can ultimately go the next step in some cases, and offer the options of nerve blocks (stellate ganglion, trigeminal), botox, lidocaine infusions, ketamine infusions and IVIGs. It can be difficult however to first get a referral (rosacea is still seen by many as a primarily 'cosmetic' issue, and many doctors do not realize how much burning pain it can give us), and then it can be difficult also to convince a pain specialist to go as far as nerve blocks. But just know that these options are available. Ideally your dermatologist should work together with a pain specialist, when you deal with nerve pain on top of your rosacea inflammation and/or flushing. Sometimes combining two antidepressants (an SSRI with Cymbalta for instance) for nerve pain gives a better result than taking just one. Blood vessel constricting medication (clonidine, beta-blockers like propranolol) can sometimes be added to nerve pain blocking medication, to stabilize the blood vessels, and reduce flushing-triggered nerve pain. Anti-inflammatory medication (plaquenil for instance, or for those who benefit from antibiotics, low dose or regular dose tetracycline antibiotics can also help) can also be added to help reduce inflammation-mediated nerve pain. Please note that opioids, anti-inflammatories, and anticonvulsants have limited effects and tolerability in the treatment of neuropathic pain..(i.e., limited efficacy, safety and tolerability issues). Regarding the use of antidepressants to treat neuropathic pain, there have been numerous studies demonstrating the pain reducing effects of antidepressants. Data is strong regarding the pain-inhibiting effects of tricyclic antidepressants (TCA) and newer agents enhancing norepinephrine and serotonin neurotransmission. In contrast, review of studies with selective serotonin reuptake inhibitors (SSRIs) show poorer or inconsistent evidence of efficacy for migraine or tension headaches, diabetic neuropathy, and fibromyalgia. Several studies of SSRI treatment for mixed-chronic pain on the other hand are universally positive.So, all in all, tetracyclic antidepressants like amitriptyline can be very effective in the treatment of nerve pain. But.... if you are a severe flusher, with hyper-reactive blood vessels, there is a chance that medication like this one can make your face more hot, more red and more dry.. Trial and error, you might be fine with it. The same goes for Neurontin and Lyrica and carbamazepine; they can all help control or diminish nerve pian that is associated with rosacea, but they also all have possible side effects with can set your face off. You simply need to try these meds. And remember, that most of them can require a good few weeks at the least of taking before they can start to work. When you suspect one or the other makes your rosacea worse, you can stop taking them (taper off ideally), then wait till your face has stabilized, and then start again. Do not change anything else in your daily routine, and see whether or not your rosacea flares up again or not. (If so, good chance that the medication is not ideal for you). It is stuff like this that drives me desperate some days: there are pain treating meds, but so often they cause the blood vessels to dilate (vasodilatation), something which is of no further consequence for people with 'just' pain symptoms, but which can make the drug close to useless for us bad rosacea flushers, who need to not only think of ways to treat pain, but also keep the root cause of it, the flushing and redness, down at the same time...
In this research, scientists tested whether or not a stellate ganglion block was effective in reducing menopausal hot flashes. There were some positive research results found for its efficiency. Read also more about ganglion nerve blocks for neuropathic pain here. Nerve blocks are currently also examined as a treatment for a condition called Harlequin Syndrome, which patients also deal with face flushing and burning (read more about this condition in this blog post I made). For Harlequin syndrome, the procedure that is used is called contralateral sympathectomy. In contralateral sympathectomy, the nerve bundles that are responsible for causing flushing in the face are interrupted. Therefore, this procedure causes both sides of the face to no longer flush or sweat. This treatment is only recommended if a person is very uncomfortable with the flushing and sweating associated with the syndrome. Recently, a novel approach to the management of Harlequin syndrome was introduced, using repeated stellate ganglion blocks, which are considered a less invasive alternative treatment
 ETS (Endoscopic thoracic sympathectomy) is a much more radical treatment option. It is the most invasive of all the sympathetic nerve block treatments (other nerve related treatments are trigeminal nerve block, sphenopalatine ganglion (SPG) blocks and superficial cervical plexus blocks). During ETS surgery, surgeons attempt to interrupt the transmission of nerve signals from the spinal column to the sweat glands and to thus prevent these nerve signals from "turning on" the sweat glands. They can 'clamp' the nerves with a special device, or completely cut them. (The clamp can in theory be removed again when demanded, but often has by then created a lot of damage to the nerves, making recovery impossible). Patients are put under general anesthesia for an ETS procedure. A miniature camera is inserted into the chest under the armpit. A lung is temporarily collapsed so the surgeons can cut or otherwise destroy the nerve paths associated with the overactive sweat glands. This procedure is permanent; there have been no successful reversal procedures reported. After the surgeon completes this procedure on one side of the body, he/she performs the same procedure on the other side.
ETS (Endoscopic thoracic sympathectomy) is a much more radical treatment option. It is the most invasive of all the sympathetic nerve block treatments (other nerve related treatments are trigeminal nerve block, sphenopalatine ganglion (SPG) blocks and superficial cervical plexus blocks). During ETS surgery, surgeons attempt to interrupt the transmission of nerve signals from the spinal column to the sweat glands and to thus prevent these nerve signals from "turning on" the sweat glands. They can 'clamp' the nerves with a special device, or completely cut them. (The clamp can in theory be removed again when demanded, but often has by then created a lot of damage to the nerves, making recovery impossible). Patients are put under general anesthesia for an ETS procedure. A miniature camera is inserted into the chest under the armpit. A lung is temporarily collapsed so the surgeons can cut or otherwise destroy the nerve paths associated with the overactive sweat glands. This procedure is permanent; there have been no successful reversal procedures reported. After the surgeon completes this procedure on one side of the body, he/she performs the same procedure on the other side.
ETS is most often used to treat severely sweaty palms, sometimes the combination of sweaty palms and sweaty underarms, and rarely facial blushing and sweating, but it is major surgery (even though it's called 'minimally invasive') with significant risks (people have died from this procure, or ended up with irreversible side-effects they couldn't live with), and limited success. ETS gives no success certainty, and a host of debilitating possible side effects. It is considered a last resort because it frequently causes serious, irreversible compensatory sweating (excessive or debilitating sweating on large areas of the body, including the back, chest, abdomen, legs, face, and/or buttocks which can be equally or even more extreme than the original hand sweating problem most people came with) as well as other serious side effects such as extreme hypotension, arrhythmia, and heat intolerance. The face often cannot sweat anymore, which causes dry skin and an increase of skin temperature, which can make rosacea worse. In a study involving 121 patients at the Medical City Hospital of Dallas, Texas, compensatory sweating occurred in more than 80% of the patients undergoing ETS. Similarly, in a Danish study conducted at the Aarhus University Hospital, 90% of the patients undergoing ETS for underarm sweating, reported compensatory sweating, half of whom were forced to change their clothes during the day because of it.
Stellate ganglion blocks are also performed in the treatment of another health condition called erythromelalgia, which has some overlap with neurogenic rosacea, and which treatment options can be interesting for us. Erythromelalgia is a rare skin disorder, characterized by redness, increased temperature and burning pain of the skin of the hands, feet and only sometimes the face (it rarely also affects the neck, ears, nose and scrotum). These attacks happen on irregular intervals. Its symptoms may be triggered by some of the same symptoms we rosacea patients have: warmth or moderate exercise, change of temperature, stress. Its attacks can be prevented or relieved by cooling. Very much like neurogenic, subtype 1 rosacea thus. It is only very rarely that this condition only manifests itself on the face (and not also on the hands and feet), but there are cases known, such as this one. (Read more about erythromelalgia versus rosacea in this blog post I made). One of the treatment options for erythromelalgia is a ganglion nerve block. It involves getting injections with an anesthetic, for instance lidocaine, in the neck, at the spot of specific (sympathetic) nerve bundles. Ganglion blocks are researched and found effective in research for some people with nerve pain in the facial region, for instance Complex Regional Pain Syndrome, or postherpetic or trigeminal neuralgia. They have symptoms of nerve pain in the face. A nerve block can also improve severe headaches. The injections block pain signals from the central nervous system and the peripheral nervous system. This treatment only offers temporary (possible) pain relief, but even after one injection, some EM patients reported two whole days of complete pain relief in the facial region (this involved someone who normally had constant burning hot facial pain). The anesthetic wears off after several hours and sometimes the pain relief is only that short lived, but it is also often the case that the pain relief lingers on for days or weeks. Usually people need a series of injections to continue the pain relief. Sometimes it takes only two injections; sometimes it takes more than 10. The relief tends to last longer with each treatment. One of the immediate (short lived) side effects and signs that the treatment worked, is increased temperature and blood flow to the face. Aiii.... not something I would be looking forward to :) Interestingly however, this treatment option is also used to treat hot flashes! As well as excessive sweating. One of the possible side effects is therefore dry skin. You can read more about this treatment option here. And when you scroll down to the bottom of this post, you can read more on Stellate Ganglion Block for the treatment of hot flashes.
In this research, scientists tested whether or not a stellate ganglion block was effective in reducing menopausal hot flashes. There were some positive research results found for its efficiency. Read also more about ganglion nerve blocks for neuropathic pain here. Nerve blocks are currently also examined as a treatment for a condition called Harlequin Syndrome, which patients also deal with face flushing and burning (read more about this condition in this blog post I made). For Harlequin syndrome, the procedure that is used is called contralateral sympathectomy. In contralateral sympathectomy, the nerve bundles that are responsible for causing flushing in the face are interrupted. Therefore, this procedure causes both sides of the face to no longer flush or sweat. This treatment is only recommended if a person is very uncomfortable with the flushing and sweating associated with the syndrome. Recently, a novel approach to the management of Harlequin syndrome was introduced, using repeated stellate ganglion blocks, which are considered a less invasive alternative treatment
 ETS (Endoscopic thoracic sympathectomy) is a much more radical treatment option. It is the most invasive of all the sympathetic nerve block treatments (other nerve related treatments are trigeminal nerve block, sphenopalatine ganglion (SPG) blocks and superficial cervical plexus blocks). During ETS surgery, surgeons attempt to interrupt the transmission of nerve signals from the spinal column to the sweat glands and to thus prevent these nerve signals from "turning on" the sweat glands. They can 'clamp' the nerves with a special device, or completely cut them. (The clamp can in theory be removed again when demanded, but often has by then created a lot of damage to the nerves, making recovery impossible). Patients are put under general anesthesia for an ETS procedure. A miniature camera is inserted into the chest under the armpit. A lung is temporarily collapsed so the surgeons can cut or otherwise destroy the nerve paths associated with the overactive sweat glands. This procedure is permanent; there have been no successful reversal procedures reported. After the surgeon completes this procedure on one side of the body, he/she performs the same procedure on the other side.
ETS (Endoscopic thoracic sympathectomy) is a much more radical treatment option. It is the most invasive of all the sympathetic nerve block treatments (other nerve related treatments are trigeminal nerve block, sphenopalatine ganglion (SPG) blocks and superficial cervical plexus blocks). During ETS surgery, surgeons attempt to interrupt the transmission of nerve signals from the spinal column to the sweat glands and to thus prevent these nerve signals from "turning on" the sweat glands. They can 'clamp' the nerves with a special device, or completely cut them. (The clamp can in theory be removed again when demanded, but often has by then created a lot of damage to the nerves, making recovery impossible). Patients are put under general anesthesia for an ETS procedure. A miniature camera is inserted into the chest under the armpit. A lung is temporarily collapsed so the surgeons can cut or otherwise destroy the nerve paths associated with the overactive sweat glands. This procedure is permanent; there have been no successful reversal procedures reported. After the surgeon completes this procedure on one side of the body, he/she performs the same procedure on the other side. In fact, most physicians do not recommend ETS surgery because of the serious negative side effects of the procedure. To make matters worse, there are testimonials from rosacea patients who had ETS, and found it did not improve their flushing and burning problems (but did give them the side-effects), despite ETS aiming to reduce facial blushing by cutting contact with the sympathetic nerves that control the supply of extra blood to the skin. ETS is mostly performed to stop people from having excessive sweating on the hands and underarms. It also has been performed to stop facial blushing. But facial flushing is something different from blushing (blushing is a short lived pinkness of the cheeks; flushing is a more severe and long lasting redness and burning of the skin, where the blood vessels in the face dilate). ETS is said to work best for sudden surges of blushing. It is not useful for people with a reddish complexion. ETS is not recommended as a rosacea treatment. Anyone considering it nevertheless is advised to first and foremost make sure that there is not an underlying skin condition causing the flushing and burning problems (rosacea is mentioned as such an underlying skin condition in information leaflets! In other words; when you have rosacea and inflammation of the skin and vessels, ETS is not the right treatment for you). When your flushing is occurring as part of the menopause, ETS is also not suitable for you. Another side-effect risk is that if the procedure works for one side and not the other, you could end up with half your face blushing. In this post in David Pascoe's Rosacea Support Group, a person with rosacea blushing however praises ETS for helping him with facial blushing.
In fact, most physicians do not recommend ETS surgery because of the serious negative side effects of the procedure. To make matters worse, there are testimonials from rosacea patients who had ETS, and found it did not improve their flushing and burning problems (but did give them the side-effects), despite ETS aiming to reduce facial blushing by cutting contact with the sympathetic nerves that control the supply of extra blood to the skin. ETS is mostly performed to stop people from having excessive sweating on the hands and underarms. It also has been performed to stop facial blushing. But facial flushing is something different from blushing (blushing is a short lived pinkness of the cheeks; flushing is a more severe and long lasting redness and burning of the skin, where the blood vessels in the face dilate). ETS is said to work best for sudden surges of blushing. It is not useful for people with a reddish complexion. ETS is not recommended as a rosacea treatment. Anyone considering it nevertheless is advised to first and foremost make sure that there is not an underlying skin condition causing the flushing and burning problems (rosacea is mentioned as such an underlying skin condition in information leaflets! In other words; when you have rosacea and inflammation of the skin and vessels, ETS is not the right treatment for you). When your flushing is occurring as part of the menopause, ETS is also not suitable for you. Another side-effect risk is that if the procedure works for one side and not the other, you could end up with half your face blushing. In this post in David Pascoe's Rosacea Support Group, a person with rosacea blushing however praises ETS for helping him with facial blushing. Blzucker wrote on August 1, 1999:
Blzucker wrote on August 1, 1999:
"I’m 25 years old and have experienced significant facial blushing since I can remember (elementary school). My brother has had the same problems as me growing up. We’ve both got red hair and very light complexions which obviously don’t make dealing with Rosacea any easier. As many of you have also done, I’ve tried about 200 different cleansers and moisturizers. They all produce different results… some better than others. None of them are good enough. I have zero tolerance for this condition. The reason that I titled this message "I don’t blush anymore" is because I’ve had Endoscopic Transthoracic Surgery (ETS). You can find out a ton of information on this procedure all over the Web. It started as a cure for sweaty palms and it was discovered that the surgical procedure also stopped facial sweating (actually stops all sweating above the nipple), and greatly decreases facial blushing. My palms might have sweat much more than the average person’s, but facial blushing was 2 million times more embarrassing than a clammy handshake as far as I was concerned. I did a TREMENDOUS amount of research on this surgery. It’s extremely risky from the standpoint of possible side effects — mainly compensatory sweating in other parts of your body (the upper half of your body loses much of its connection with your sympathetic nervous system and the lower portion of your body — below your nipples — takes on the job often causing a great deal of sympathetic activity (sweating) on your chest, lower back, butt, legs, feet, etc. Another side-effect is that your palms are extremely dry. I’m detailing this (and could get even more detailed if I didn’t want to put some of your to sleep with the length of this message) because this procedure is not a good option unless you’re COMPLETELY aware of the risks and do some thorough investigation. The Dr’s Web sites are not good sources for unbiased information. They’re making big bucks off this relatively new procedure and won’t tell you about the small group of patients who have ended up with disastrous results. I was lucky… the procedure has worked very well. I would have rated by facial blushing/ sweating/ general redness to be about 8.5 on a scale of 1-10. Not an hour would go by without my obsessing over the problem. Few days would go by without somebody calling attention to my problem. Triggers were the normal rosacea variety… spicy food, alcohol, hot rooms, coming in from the cold, etc… if you’ve read this far you’re aware of the stuff I’m talking about. Although I was diagnosed with Rosacea in 1993, I was so disappointed with the treatment options (or lack thereof) that I continued to look elsewhere for help. Finding a good soap gave me way better results than MetroGel, and taking oral medications was not going to be acceptable to me. This ETS surgery, which I saw as a way of curing all of my blushing/ flushing/ redness, seemed to be worth the considerable risk that goes along with it (again – don’t let any doctor tell you otherwise)."
Post-Surgery… "I don’t have that rush of blood to my face when somebody says something embarrassing. That’s about it. Alcohol still gets my cheeks and neck flushed most all the time. Going from a really cold area into the heat (best example is coming into a ski lodge after a day of swimming) will guarantee a red face (plus I don’t sweat or have any really effective way of cooling my face off after it’s gotten red). I will say that in general, my face isn’t as red as what it was like before surgery. However, it’s MUCH dryer. My scalp is also very dry. Only a moisturizing shampoo and conditioner prevent me from flaking all over the place.[..] My feet sweat like crazy – way more than before the surgery. However, Botox injections (search the Web for that too) have reduced that problem to a comfortable level (but cost about $2000 annually). Prior to ETS surgery, if I was guaranteed the result I ended up with, I would do it. I’m better off having had the surgery. However, there are some incredibly tragic stories related to ETS gone bad, and I have not been able to recommend the procedure to my brother (who has rosacea-induced flushing/blushing/redness symptoms as bad or worse than me) because I would take my own life if I ruined his by convincing him to try this risky procedure. After having had the surgery, I’m more convinced than ever that I have Rosacea. Spicy foods are still a killer. Alcohol still causes my skin to turn red. A day at the beach still has the aftermath you’re all experiencing. Going from a cold room into the heat still causes me to flush."
 This devastating account is from a woman, who is experiencing a high degree of compensatory sweating and shows emphatically the downside of this procedure
This devastating account is from a woman, who is experiencing a high degree of compensatory sweating and shows emphatically the downside of this procedure"I am a 38-year-old woman who feels totally out of place. I started off sweating on my hands and feet and I had the ETS surgery. Immediately after the surgery, while I was still in the hospital bed, I awakened to a sweaty butt, back, and legs. The doctor said it was compensatory sweating and it would go away. I continued to sweat and eventually I requested the clamps used to block the nerves be removed. The doctor stated the nerve should regenerate itself and the compensatory sweating would stop and my hands and feet would probably continue to sweat. It has been more than 4 years and in that time I have totally removed myself from everyone. I have had to switch job positions two times. I can't speak or stand up in front of a crowd. My clothes get soaked. People often say I have a stain on my butt. My back, chest, and stomach constantly sweat. My ex boyfriend called me "sweaty butt" and always made comments about the bed being wet. I wear a lot of black and have spent hundreds of dollars on Under Armor gear and underarm pads. Nothing works. This condition causes me great depression. I cannot wear shorts, tank tops, or light-colored shirts. My jeans get wet in the butt and around the waist. I don't date. Every time I do, the young men always ask me 'What is wrong?' and 'Why are your clothes wet? It's disgusting.' I cry and cover up a lot. I need help."
.jpg) Here you can read another painful patient testimonial of someone who had excessive compensatory sweating after ETS surgery
Here you can read another painful patient testimonial of someone who had excessive compensatory sweating after ETS surgery
"As each day passed, it only got worse. By the end of summer, I had to wear two to three undershirts to contain the bulk of the sweat. Then, out of nowhere, the sweating appeared on my left shoulder blade. Of course, my doctor kept blaming it on the heat. But by then, I was going through four to five undershirts a day. So here I am, stuck with torso sweating that is much worse than the sweat from my head and a random area on my left shoulder blade. Try explaining that to people. The side effects of ETS didn’t end with sweating, either. I experienced a noticeable lack of energy and felt like my thought process was flawed. It took three times longer to make a simple impulse purchase decision than it used to. My natural feelings of assertiveness seemed to diminish because ETS impairs your fight-or-flight capabilities. The surgery also made my face super dry or oily, and acne appeared for the first time ever. Eventually, the effects trickled down to my hands, which also dried up badly. My metabolism was cut in half. My scalp dried out. Then I started to dramatically lose my hair. Search YouTube for “ETS Side Effects,” and you’ll get some real-life experiences. Be cautious of clicking on the ads, which are most likely pro-ETS." And here you can read another striking patient account of excessive compensatory sweating in the Guardian newspaper. I will try to make an independent blog post in the near future about ETS.
.jpg) In this Pubmed article the efficiency of ETS surgery for facial blushing was researched and confirmed:
In this Pubmed article the efficiency of ETS surgery for facial blushing was researched and confirmed:"Objective: No study has yet compared the efficacy of endoscopic thoracic sympathectomy (ETS) for treating facial blushing with other treatment or no treatment. We conducted a prospective, observational, open-label, clinical study to compare ETS for blushing with generalized social anxiety disorder versus sertraline treatment and no treatment.
Method: Three-hundred and thirty consecutive patients seeking treatment for their blushing were assessed by psychiatric interview and patient-rated scales. The Brief Social Phobia Scale was the primary outcome measure. Patients meeting Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition criteria for generalized social anxiety disorder, scoring 20 points or more in the Brief Social Phobia Scale and 19 points or more in the Social Phobia Inventory were considered eligible and followed up for a mean of 11 months (range 1–64) after ETS or initiation of sertraline.
Results: At baseline, 97 percent of the ETS-treated group, 87 percent of the sertraline-treated group, and 78 percent of the nontreated group rated their blushing as being “severe” or “extreme.” At follow up, 16 percent of ETS-treated patients, 32 percent of sertraline-treated patients, and 57 percent of untreated patients reported this degree of blushing. At endpoint, Brief Social Phobia Scale total scores exhibited a greater decline with either treatment than with no treatment. Nonetheless, in comparison to no treatment, only the results obtained with ETS achieved statistical difference (p=0.003). Compensatory sweating occurred in 99 percent of patients who underwent endoscopic thoracic sympathectomy. High degrees of satisfaction with treatment were reported by 89 percent of patients undergoing ETS and by 59 percent of patients taking medication.
Conclusion: ETS was associated to a greater reduction of blushing and Brief Social Phobia Scale scores, and higher degrees of satisfaction with treatment, in comparison to sertraline and no treatment."
And in this scientific article (read excerpt here), ETS was considered an effective treatment for neurogenic rosacea. Scientists warn for the potentially serious side-effects of ETS though.
 What exact chemicals in the body are involved with nerve pain?
What exact chemicals in the body are involved with nerve pain? Neuropathic pain is in essence a defense mechanism of the body, warning us for injury or damage. Pain is a complex interaction of physical, mental and environmental factors. Pain has many gradations and is also subjective, and can be experienced different depending on the person. Nerve pain is the result of damaged or reduced functioning nerves. They give off a constant message to the brain, that something is wrong on that specific spot. This creates an over-stimulation of the nerve, which makes it hypersensitive. Patients can experience non painful stimuli as painful (think of the sensation of fabric touching the skin, or the sensation of cold or warm air touching the skin). Patients can also feel a constant dull pain without clear cause for it. It is hard to treat nerve pain and it can linger for a long time, often chronically. nerve pain is also described as constantly present burning, itching, stabbing electrical, painful coldness or a numb feeling. The location of the pain does not have to correspond with the place where the nerve damage is exactly. I have a constant dull pain in my cheeks. It is a mildly burning and tight feeling, even when I am not flushed or cooling my face with a fan. When I have a big flush, the pain increases tenfold. It is very hard to deal with this daily.. Pressure on the nerves in the face can cause nerve pain; think of swelling of rosacea skin, redness from inflammation, pressure from dilated blood vessels and the effects of inflammation.
Special receptors and nerves guide pain stimuli to the brain. It is only once these signals reach the brain, that we 'feel' the pain. Our body does not have specific 'pain receivers'; instead, the nerve endings of two types of nerves, the fast A delta fibers and the slow C-fibers are responsible for the sensation of pain in our body. These nerve endings are sensitive to pressure, temperature and to a large amount of chemicals in our body (neurotransmitters) that are released at the site where pain is sensed.Neurotransmitters are like the messengers of the nerve system. Aside from the neurotransmitters noradrenaline, serotonin and dopamine, our body also produces prostaglandine, bradykinin and substance P. When someone sticks a needle in your skin, for instance, you first feel a mild stabbing pain on the site; this is the fast acting A delta (nerve) fiber that was triggered instantly (and it triggers the body and the central nervous system directly; we pull our hand back immediately, our blood pressure and breathing intensify right away, even before our brain has made us feel the pain). Then follows a burning pain (warning us for tissue damage), which is triggered by the slower acting C-fibers (warning us for more long standing discomfort being on the way). So, there are two routes which these pain signals can take, when they travel to the brain: a fast pain one (red on the picture above) or a slow pain one (yellow). The fast pain route ends in the thalamus (B), which redirects the signal further to other parts of the brain. The slow pain route leads the the brain stem (A), and sometimes also to the thalamus (B). The brain then sends the signal back, after which the body responds.These pain receiving nerve endings aren't evenly divided over our body. Our skin, hands and gums have relatively many of them, while our belly and brain have less of them. The fast A fibers and the slow C fibers transport the pain signals to the spinal cord. The painful spot then releases neurotransmitters and the fast A fibers transport the pain signal to the brain. (They transport them through the nerve system at the opposite side of the body! So when you feel pain in your left hand, the pain signals are transported on the right side of your body to the brain). They arrive in the thalamus center in the brain, which exchanges information with the relevant part of the brain. Only when the pain signal is strong enough and can reach the cortex in the brain, will we become aware of the pain. The central nervous system then modulates the pain signal; strengthens or weakens the pain signal, depending on the amount and types of neurotransmitters that are released on the site of the injury. Pain signals from the slow C-fibers pass different parts of the spinal cord before reaching the thalamus in the brain. The brain can set a system in motion (by producing specific neurotransmitters; endorphins, but also serotonin and noradrenaline) that can either stem or strengthen the pain sensations. So in the end, the amount of pain we feel depends on the amount and type of neurotransmitters that are released by our body and that reach our pain receptors.
 When you have chronic pain, our neurotransmitter system can experience changes. The type of neurotransmitter chemicals can change. The amount and type of receptors can change. For instance, as a result of chronic neuropathic pain, a very specific receptor in the spinal cord is activated (N-Methyl-D-Aspartate - NMDA). New pain-related research can hopefully come up with medication to influence this receptor. And within the (central) nervous system, new connections can appear between nerve bundles and nerves; this can lead for instance to new short circuits between nerves that signal pain and nerves that signal touch, making touching of the skin suddenly painful. We also build up a 'pain memory' with chronic pain. Think of phantom pain. The precise mechanisms of pain perception and transmission in the central nervous system have not been fully discovered. However, extensive research indicates that dopamin, serotonin,
When you have chronic pain, our neurotransmitter system can experience changes. The type of neurotransmitter chemicals can change. The amount and type of receptors can change. For instance, as a result of chronic neuropathic pain, a very specific receptor in the spinal cord is activated (N-Methyl-D-Aspartate - NMDA). New pain-related research can hopefully come up with medication to influence this receptor. And within the (central) nervous system, new connections can appear between nerve bundles and nerves; this can lead for instance to new short circuits between nerves that signal pain and nerves that signal touch, making touching of the skin suddenly painful. We also build up a 'pain memory' with chronic pain. Think of phantom pain. The precise mechanisms of pain perception and transmission in the central nervous system have not been fully discovered. However, extensive research indicates that dopamin, serotonin, monoamine neurotransmitters and norepinephrine all play a role in the perception of nerve pain (in particular an imbalance of serotonin and norepinephrine). Experiments with animal models of pain indicate that noradrenergic interventions, and to a lesser extent serotonergic interventions, reduce pain-related behavior. In humans, antidepressants have been shown to reduce pain and functional impairment in central and neuropathic pain conditions. These effects are particularly well-studied in trials with serotonin-norepinephrine reuptake inhibitors (SNRIs).
Researchers at The Johns Hopkins University and the University of Maryland discovered that the brain uses serotonin to let pain signals in chronic pain linger on for longer. Chronic pain seems to cause serotonin to be released by the brain into the spinal cord. There, it acts on the trigeminal nerve at large, triggering nerve sensitivity throughout nerve branches, even causing some non-pain-sensing nerve cells to start responding to pain. It causes the nerves to fire more frequently, sending additional pain signals to the brain. This also appears to have a role in the phenomenon that causes uninjured areas of the body to be more sensitive to pain when an area nearby has been hurt. In their new research, the scientists focused on a system of pain-sensing nerves within the faces of mice, known collectively as the trigeminal nerve. The trigeminal nerve is a large bundle of tens of thousands of nerve cells. Each cell is a long “wire” with a hub at its center; the hubs are grouped together into a larger hub. On one side of this hub, three smaller bundles of wires — V1, V2 and V3 — branch off. Each bundle contains individual pain-sensing wires that split off to cover a specific territory of the face. Signals are sent through the wires to the hubs of the cells and then travel to the spinal cord through a separate set of bundles. From the spinal cord, the signals are relayed to the brain, which interprets them as pain. When the researchers pinched the V2 branch of the trigeminal nerve for a prolonged period of time, they found that the V2 and V3 territories were extra sensitive to additional pain. This spreading of pain to uninjured areas is typical of those experiencing chronic pain, but it can also be experienced during acute injuries, as when a thumb is hit with a hammer and the whole hand throbs with pain. Nerves that don’t normally respond to pain can modify themselves during prolonged injury, adding to the pain signals being sent to the brain. Then the team, led by Feng Wei, M.D., Ph.D., blocked the production of serotonin, which is released from the brain stem into the spinal cord, and found that nerve hyperactivity nearly disappeared.
 So, serotonin, dopamine and noradrenaline all play a role in controlling nerve pain
So, serotonin, dopamine and noradrenaline all play a role in controlling nerve painOne way of focusing on those three neurotransmitters, is to see why it is that some antidepressants are successfully treating nerve pain. Many researchers believe that the benefits of antidepressants stem from how they affect certain brain circuits and the chemicals (called neurotransmitters) that pass along signals from one nerve cell to another in the brain. These chemicals also include serotonin, dopamine, and norepinephrine. In various ways, different antidepressants seem to affect how these neurotransmitters behave. Some of the most commonly prescribed antidepressants are called reuptake inhibitors (SSRI's for instance). Reuptake refers to the process in which neurotransmitters are naturally reabsorbed back into nerve cells in the brain after they are released to send messages between nerve cells. A reuptake inhibitor prevents this from happening. Instead of getting reabsorbed, the neurotransmitter stays, temporarily, in the gap between the nerves (synapse). And when you keep levels of the neurotransmitters higher, this can improve communication between the nerve cells. And that can strengthen circuits in the brain which regulate mood. But these antidepressants even often help patients with nerve pain who are not depressed. And while these antidepressants can take 2 to 5 weeks of use before they start to show antidepressant effects, their nerve pain effects start within days to a week of use. Studies revealed that noradrenaline is extremely important for the reducing of neuropathic pain. When you take an SSRI antidepressant, the antidepressants bind to noradrenaline and serotonin (5-HT) transporters. Reuptake of these neurotransmitters is inhibited, so that means your body will have increased levels of noradrenaline and serotonin 5-HT available. When your body (spinal cord) has more noradrenaline available (by preventing them from being reabsorbed by the body right away), it has proven to reduce neuropathic pain (through α2-adrenergic receptors). Serotonin and dopamine are also thought to reinforce the noradrenergic effects in reducing neuropathic pain. Tricyclic antidepressants (TCA's) are statistically most effective at this. Dual-type TCAs (e.g., amitriptyline, imipramine, clomipramine), which inhibit reuptake of both noradrenaline and 5-HT (serotonin) are also effective. Noradrenaline reuptake inhibitors (nortriptyline, desipramine) are scoring a bit lower on the efficiency comparison ladder. SSRI type of antidepressants score relatively welland SNRI-antidepressants a little bit lower. All in all, an antidepressant that inhibits reuptake of both noradrenaline and 5-HT (serotonin) has stronger pain numbing effects than a drug that selectively inhibits reuptake of only one of these neurotransmitters, and noradrenaline plays a greater role than 5-HT (serotonin) when it comes to numbing nerve pain.
Dopamine
Dopaminergic neurotransmission plays a central role in changing pain perception and in pain control within certain parts of the brain. Low levels of dopamine often result in higher pain levels in people with Parkinson’s disease for instance. And abnormal dopaminergic neurotransmission has also been demonstrated in painful conditions such as fibromyalgia, burning mouth syndrome and painful diabetic neuropathy. Dopamine seems to play a key role in maintaining chronic pain. Researchers traced the pain signalling pathway between the brain and spinal cord in an animal model and found that removing dopamine-containing cells reduced chronic pain. These dopamine cells turn out to have no effect on acute pain, but do seem to have a significant effect on chronic pain. However, medication which prevents the reuptake of dopamine, can also help control nerve pain oddly enough.. Read: 'dopamine increases in the central nervous system are likely to play a role in the inhibitory effect of antidepressants on neuropathic pain' -
"Bupropion, a dopamine noradrenaline reuptake inhibitor, increases noradrenaline
and dopamine levels in the spinal cord and suppresses hyperalgesia in a rat neuropathic pain model through α2-adrenergic receptors and D2-like receptors. No other antidepressants are reported to strongly inhibit dopamine transporters. Nevertheless, we demonstrated that intraperitoneal administration of amitriptyline (TCA), duloxetine and milnacipran (SNRI) and fluoxetine (SSRI) at a dose of 10 mg/kg, all increased dopamine in the spinal cord and inhibited hyperalgesia in a rat model of neuropathic pain through D2-like receptors. There are few dopamine transporters in the frontal cortex and reuptake of dopamine is mediated by noradrenaline transporters. It is unclear why antidepressants increase dopamine levels in the spinal cord. Dopaminergic neurons in the ventral tegmental area (A10) release dopamine in the nucleus accumbens and enhance analgesic activity through D2-like receptors. A previous study demonstrated that duloxetine (25 mg/kg orally) increases dopamine in the nucleus accumbens, but amitriptyline and maprotiline (both 50 mg/kg orally) do not have this effect [80]. Dopamine enhances the antinociceptive effects in the striatum. Although it is unclear whether antidepressants increase dopamine in these brain areas, dopamine increases in the central nervous system are likely to play a role in the inhibitory effect of antidepressants on neuropathic pain."
and dopamine levels in the spinal cord and suppresses hyperalgesia in a rat neuropathic pain model through α2-adrenergic receptors and D2-like receptors. No other antidepressants are reported to strongly inhibit dopamine transporters. Nevertheless, we demonstrated that intraperitoneal administration of amitriptyline (TCA), duloxetine and milnacipran (SNRI) and fluoxetine (SSRI) at a dose of 10 mg/kg, all increased dopamine in the spinal cord and inhibited hyperalgesia in a rat model of neuropathic pain through D2-like receptors. There are few dopamine transporters in the frontal cortex and reuptake of dopamine is mediated by noradrenaline transporters. It is unclear why antidepressants increase dopamine levels in the spinal cord. Dopaminergic neurons in the ventral tegmental area (A10) release dopamine in the nucleus accumbens and enhance analgesic activity through D2-like receptors. A previous study demonstrated that duloxetine (25 mg/kg orally) increases dopamine in the nucleus accumbens, but amitriptyline and maprotiline (both 50 mg/kg orally) do not have this effect [80]. Dopamine enhances the antinociceptive effects in the striatum. Although it is unclear whether antidepressants increase dopamine in these brain areas, dopamine increases in the central nervous system are likely to play a role in the inhibitory effect of antidepressants on neuropathic pain."
 But that is not all. Antidepressants also act as sodium channel blockers. Sodium channel blockers inhibit ectopic discharges occurring when there is nerve damage, thereby inhibiting neuropathic pain. Second, some antidepressants act as NMDA receptor antagonists [87,88]. NMDA receptors, which are expressed in the neurons of the dorsal horn of the spinal cord, induce wind-up and central sensitization result in contribute to the onset and maintenance of neuropathic pain. Tricyclic antidepressants (TCAs) for instance, act as α1-adrenergic receptors, calcium channel blockers, potassium channel activators, modulate the adenosine system and increase GABA-B receptor function. They activate opioid receptors, inhibit the production of nitric oxide, prostaglandin E2 and have a variety of other actions that may inhibit neuropathic pain in a complex manner. For more in debt explorations of the exact method of acting, read this medical article. Summarized, the main mechanism of antidepressants that control and reduce neuropathic pain is first, to increase noradrenaline in the spinal cord. Second, to act on a specific group of nerve cells that contain noradrenaline in the brain (the locus coeruleus), thereby directly inhibiting pain. Dopamine and serotonin also increase in the central nervous system and may increase the pain reducing effects of noradrenaline. When you look for an antidepressant medication to help you with nerve pain, try the ones which help your body create the most noradrenaline first. Tricyclic antidepressants have a particular good track score and work in several ways to reduce nerve pain. The downside is that they can make the face a bit more red and warm, in some cases, as they have anticholinergic effects.
But that is not all. Antidepressants also act as sodium channel blockers. Sodium channel blockers inhibit ectopic discharges occurring when there is nerve damage, thereby inhibiting neuropathic pain. Second, some antidepressants act as NMDA receptor antagonists [87,88]. NMDA receptors, which are expressed in the neurons of the dorsal horn of the spinal cord, induce wind-up and central sensitization result in contribute to the onset and maintenance of neuropathic pain. Tricyclic antidepressants (TCAs) for instance, act as α1-adrenergic receptors, calcium channel blockers, potassium channel activators, modulate the adenosine system and increase GABA-B receptor function. They activate opioid receptors, inhibit the production of nitric oxide, prostaglandin E2 and have a variety of other actions that may inhibit neuropathic pain in a complex manner. For more in debt explorations of the exact method of acting, read this medical article. Summarized, the main mechanism of antidepressants that control and reduce neuropathic pain is first, to increase noradrenaline in the spinal cord. Second, to act on a specific group of nerve cells that contain noradrenaline in the brain (the locus coeruleus), thereby directly inhibiting pain. Dopamine and serotonin also increase in the central nervous system and may increase the pain reducing effects of noradrenaline. When you look for an antidepressant medication to help you with nerve pain, try the ones which help your body create the most noradrenaline first. Tricyclic antidepressants have a particular good track score and work in several ways to reduce nerve pain. The downside is that they can make the face a bit more red and warm, in some cases, as they have anticholinergic effects. In this string of forum posts, rosacea patients with nerve pain discuss their experiences with gabapentin (Neurontin) and pregabalin (Lyrica), as well as other nerve pain meds
In this string of forum posts, rosacea patients with nerve pain discuss their experiences with gabapentin (Neurontin) and pregabalin (Lyrica), as well as other nerve pain medsAs shown Neurontin and Lyrica especially can be very helpful for flushers and burners! The possibility of side-effects does not mean everyone gets them, far from it in fact.
ZK_78 wrote on April 17th 2017: "Pain control – Amitriptyline / Gabapentin - I am currently taking high doses of oral Amitriptyline with little success for the pain from Type 1 Rosacea nerve pain. In the past I have taken Gabapentin also with little improvement. Has anybody found an effective way of controlling the pain from Type 1 Rosacea?"
Laser_cat replied on April 17th 2017: "Hi, In this thread someone mentioned anti-migraine drugs like Maxalt, and narcotics like Roxicodone. I am in a similar boat, having tried cymbalta, effexor, topical ketamine/amitriptyline with no improvement. Am just ramping up on gabapentin, but don't notice much. I saw Dr. Tim Berger at UCSF who said it is trial and error and he cannot predict who responds to which medication. He suggests for me to try next: lyrica, doxepin, mexiletine, baclofen. A few more meds (like memantine, topical capsaicin, anti-malarials) are included here. I hope you eventually have improvement. [..]
Update from my end - the gabapentin seemed to help (maybe) for 1-2 days and then was definitely making things worse (flushing and burning both). I have read similar experiences with gabapentin from other forum users. Arg! I am actually trying out botox injections very soon from my rheum. From anecdotal reports here, they seem to hold some promise (more so it seems, than gabapentin). I want to see how much mileage I can get from botox before I try other oral meds with more systemic side effects. Hope you are well."
Laser_cat replied on May 1st, 2017: "I had a few botox injections initially to make sure I didn't have a bad reaction, and to gauge how much I'll be paralyzed. Since I did ok, my rheum was comfortable increasing the dose and surface area covered. I had 2 more procedures - the first being most of my cheeks (had some improvement, which only lasted for ~ 4 days), and the second being a bit more cheek, outside of nose, chin (I just had that done, crossing my fingers). I will be getting more injections in ~1 month. My rheum doesn't have much experience with doing botox for flushing purposes, so I actually recently asked him to consult with an out-of-state dermatologist (whose name I kindly got from someone on this forum) who had some success. In any case, botox seems much "safer" than lasers/ipl (which did not help me). I've never read about anyone having increased flushing/burning from botox, but could be wrong. I've been on clonidine for many months now. It was more help with my flushing in the beginning (and helped me more so than propranolol, I believe), but never enough to get me out of a debilitating state. If you haven't yet tried clonidine, I would still recommend it though (I'm assuming your flushing and burning go hand in hand, which I realize may not be the case ... )"
Redtere wrote on May 1st, 2017: "I took 20mg of Amitriptyline for a month back in 2003. It actually helped the flushing and flareups but didn't stop the pain and tingling. What dose are you on and has it helped your flushing at all."
ZK_78 wrote on May 3rd, 2017: "Hi, I currently take 35mg of Amitriptyline each night. This is the highest does I can tolerate, otherwise I experience tiredness and drowsiness the following day. It has marginally helped with the pain but unfortunately not with the flushing. [..] I am currently taking 3 * 100 mcg of Clonidine per day (breakfast, lunch and evening meals). I find it effective for the flushing with little in terms of side effects. If I could only address the pain then I would be in a really good position. Regards."
Laser_cat wrote on May 8th, 2017: "Hi there, I have tried Lyrica for the past 4 days and it has helped with the pain quite a bit, I'd say over 50%. Still early though, but I'm excited. My rheum says in many ways lyrica is a much better drug than gabapentin. Hope you are well. [..] Lyrica/ pregabalin to me is superior to gabapentin. It is a bit sedating though (like all these drugs, it seems!) but I'm hoping my body will adjust to that. It is extremely helpful for the pain. My body isn't really responding to the botox, sadly I am having a full-face procedure at the end of the month, and then will re-evaluate ... I will update after my next procedure. No downsides though, at least. Best, Lizzy"
 Laser_cat wrote on September 13th 2018: "I was on 225 mg ER effexor that was helpful, but I think the norepinephrine was giving me heart racing episodes (like anxiety beyond my control) which contributed to flushing. My understanding is the norepinephrine helps give some blood vessel constriction but the downside is it might rev you up a bit / increase blood pressure. It was very helpful apart from those heart racing episodes, though! For this reason I tried to see if another antidepressant would work better for me. I switched to zoloft (an SSRI) for a bit but realized I do much better on an SNRI (mentally and flushing both). So I switched to cymbalta and am doing well on that (in addition to mirtazapine 22.5 which I think amplifies the norepinephrine a bit on the blood vessels .... but the SNRI's I feel are stronger?) I'm on 80 mg cymbalta in the morning,and do well. The cymbalta gives me some heart racing too, but not as bad as effexor and just slapped on atenolol to take care of that. [..] I've been on an SNRI for years prior to my onset, so i think my body was used to a single antidepressant enough to handle cymbalta + mirt. together. But, maybe it would be too much norepinephrine/serotonin if you are not used to it, you might feel too hot, etc. Antidepressants are so individual (some people take SSRI's for Raynaud's ... some people it makes them flush more .. .some less .. etc) so titrate up slowly. I have tried an SNRI, mirtazapine each together and individually and find the most benefit with both, then effexor or cymbalta alone, then mirtazapine to barely make a dent (all with respect to flushing .. but actually both mood and flushing). [..] I know increasing serotonin (as well as dopamine, norepinephrine) in the brain can all help with burning pain/sensation via descending inhibition pathways (if you have that issue). I notice that SSRI's and SNRI's all increase sweating for me (trunk / armpits) which in turn might help the flushing."
Laser_cat wrote on September 13th 2018: "I was on 225 mg ER effexor that was helpful, but I think the norepinephrine was giving me heart racing episodes (like anxiety beyond my control) which contributed to flushing. My understanding is the norepinephrine helps give some blood vessel constriction but the downside is it might rev you up a bit / increase blood pressure. It was very helpful apart from those heart racing episodes, though! For this reason I tried to see if another antidepressant would work better for me. I switched to zoloft (an SSRI) for a bit but realized I do much better on an SNRI (mentally and flushing both). So I switched to cymbalta and am doing well on that (in addition to mirtazapine 22.5 which I think amplifies the norepinephrine a bit on the blood vessels .... but the SNRI's I feel are stronger?) I'm on 80 mg cymbalta in the morning,and do well. The cymbalta gives me some heart racing too, but not as bad as effexor and just slapped on atenolol to take care of that. [..] I've been on an SNRI for years prior to my onset, so i think my body was used to a single antidepressant enough to handle cymbalta + mirt. together. But, maybe it would be too much norepinephrine/serotonin if you are not used to it, you might feel too hot, etc. Antidepressants are so individual (some people take SSRI's for Raynaud's ... some people it makes them flush more .. .some less .. etc) so titrate up slowly. I have tried an SNRI, mirtazapine each together and individually and find the most benefit with both, then effexor or cymbalta alone, then mirtazapine to barely make a dent (all with respect to flushing .. but actually both mood and flushing). [..] I know increasing serotonin (as well as dopamine, norepinephrine) in the brain can all help with burning pain/sensation via descending inhibition pathways (if you have that issue). I notice that SSRI's and SNRI's all increase sweating for me (trunk / armpits) which in turn might help the flushing.""Lyrica medication. My flushing has continued and actually is getting worse."
 Mswilson21 wrote on the 28th September 2006: "Ok, so I am supposed to check in with my doctor tomorrow regarding my Lyrica medication. My flushing has continued and actually is getting worse. Not sure if I will continue with this drug but I will consult with my doc first. If I do, then I will definitely have to go in for an IPL treatment soon. I just wish I knew if the flushing will persist or if my body will get used to it. Bellamermaid said that she noticed increased flushing for the first 4 weeks she was on it. With that being said I might decide to stick with it because she said that it has helped her so much.
Mswilson21 wrote on the 28th September 2006: "Ok, so I am supposed to check in with my doctor tomorrow regarding my Lyrica medication. My flushing has continued and actually is getting worse. Not sure if I will continue with this drug but I will consult with my doc first. If I do, then I will definitely have to go in for an IPL treatment soon. I just wish I knew if the flushing will persist or if my body will get used to it. Bellamermaid said that she noticed increased flushing for the first 4 weeks she was on it. With that being said I might decide to stick with it because she said that it has helped her so much.Mswilson21 updated on October 3rd 2006: "So, after consulting with my doc, I decided to stop taking Lyrica. The flushing not only persisted, but was getting worse. He said that Neurontin doesn't have the side effects and might be worth a try but I may hold off for a little bit. I'll post my experience if I decide to go that route."
Twickle Purple replied on October 3rd 2006: "I hope the Neurontin does the job for you mwilson21. I use it and have only mild fuzziness while i am acclimating to it. I increase the dose very slowly to avoid this and I take it at night. However, I have learned to keep my dosage relatively low now because at higher doses I was fuzzy fulltime."
I replied on October 4th 2006: "Hi, I've been taking neurontin for about 3 or 4 weeks now and eventually it worked wonders, making me more pale and helping a lot with my neuropathic and burning pain. But after a couple of weeks I'm getting the feeling that it actually starts to make me a bit more red and even flushed sometimes. Very difficult to tell though and lately my right cheek is playing up again and has another sunburn-like reaction, so I take diclofenac (NSAID) with it to hopefully calm this redness and burning/ flushing on the right side down a bit... I noticed that "vasodilatation" and "hypertension" are mentioned as "frequent" side effects for neurontin. That is not flushing (which is noted for Lyrica), but still not good for us. So I'll start trying another painkiller by monday; Tegretol (carbamazepine).
https://www.mentalhealth.com/drug/p30-t01.html
http://www.helpforpain.com/articles/understand-neuropathic-pain/understanding.htm
Carbamazepine doesn't have vasodilatation, flushing, hot flash or anything mentioned as side-effect, but because it acts an an anticholinergic, it works on the central nerve system and can cause drowsiness etc and thereby increased blood flow in the face. Like all medication that works on the CNS. https://en.wikipedia.org/wiki/Anticholinergic If you check the given links out, you'll see that neuropathic pain management comes down to either tricyclic antidepressants like amitriptyline (which I tried a few years ago and made me definitely flush a lot more. Flushing is mentioned with all the tricyclics, and my pharmacist explained that this drugs can widen the little blood vessels in the face), modern SSRI antidepressant (which give facial flushing as well often), anticonvulsants like Carbamazepine, phenytoin, gabapentin (or Lyrica) and lamotrigine and eventually certain antiarrhythmics, such as lidocaine and mexiletine. Also there are opioids, but they can cause facial flushing AS WELL (SIGHT................). So I would bet on either gabapentin, which is registered as helpful for menopausal hot flashes as well (does something with the calcium channels and regulates body temperature, which is promising for us), or the carbamazepine, which I will try myself by next week, so I'll update on that one as well. They there is Trileptal (oxcarbazepine), which is a derivative from carbamazepine (Tegretol), like Lyrica from neurontin, but Trileptal has a high incidence of facial acne and depression, and I rather give the Tegretol a fair chance first. Besides: Tegretol has a proven track for the treatment of neuropathic pain and Trileptal has still studies running for this. Hope you can try the gabapentin mwilson21, it certainly helps for the burning with me. Nat"
Lakan replied on October 23rd 2006: "I would just like to add one thing. Someone said that one of Lyricas side-effects is flushing (that's true) and that Neurontin does not have that side-effect. I'm eating Lyrica, I do not experience more flushing but I just wanted to check the side-effects of Neurontin and on the common side-effects list it says "flushing, dilation of blood vessels" while on Lyricas side-effects flushing is listed on the less common side-effects list. Just wanted to post this if someone is choosing between the two drugs, worth knowing."
Froggirl replied on October 23rd 2006: "Just wanted to say for anyone tossing up which of these to try, that my doctor, pharmacist and dermatologist all agree that Neurontin is less likely than Lyrica to cause flushing. I have looked into this in detail as I have bad nerve pain in my face and had a terrible reaction to tricyclic antidepressants. 2.5mg was enough to cause a month of extreme flushing, not just my face but my knees, arms, legs, chest and ears. SSRI's also gave me bad flushing. Of course for any one who flushes at the drop of a hat like me Neurontin, like any med, could possibly cause flushing, however i have been told that it is less likely too than Lyrica."
Mswilson21 wrote on November 13th 2006: "I just started taking neurontin on Friday, 100 mg once at night. From what I have read and what my doctor has told me, neurontin is very well tolerated by most patients unlike Lyrica which is much stronger. Lyrica has a flushing side effect that neurontin does not. I am going to build my way up as I go and will keep everyone informed on how things go."
Lakan updated on January 22nd 2007: "Just wanted to say that Lyrica is a great medication, really. I have eaten it now for about 5 months and I'm done with it in about 1 month and I got to say that I am really pleased with this medication this far. I no longer got any big problems with burning, actually I experience burning very rarely and quite mild those times I get it. Before Lyrica I got burning with almost every flush and sometimes for no apparent reason. It is so much better now. Hope it will stay better after I've finished it too. Just wanted to write this, can be good for people to see posts like this if they try to decide whether or not to try a medication. I'm on 75 mg twice/day."
Kanmi wrote on January 28th 2007: "I started taking Lyrica about a week ago I think. It was already helping dramatically with my flushing and pain."
Lakan updated on October 30th 2008: "Pregabalin (Lyrica) helps me very, very much with the pain and with no side effects at all. Doesn't do anything for my flushing though but I love this medication. Never tried Gabapentin. Pregabalin is the "stronger" one, fairly new. Gabapentin has been around for a while and you usually need a higher dose of Gabapentin than with Pregabalin. I also think there's more side effects associated with Gabapentin but I'm not totally sure. What I know though is that I only need 150mg/day (Pregabalin) and that eliminates at least 90% of my pain without any side effects."
WrinkledClue replied on October 30th 2008: "Please be careful with Gabapentin; I took it for two days (I think it was 300 mg) and my face flared unbelievably badly from it. My rosacea doctor says we rosaceans are frequently sensitive to meds that non rosaceans are not.-WC [..] Gabapentin made me flush horrifically. It was appalling. Really dreadful. I urge caution!"
 Vicki wrote on April 12th 2011: "I take Neurontin (gabapentin is generic, Neurontin is brand) for back pain and fibromyalgia. It doesn't do much for my rosacea pain. However, everyone is different as you know so it might help you. It is non addictive as far as I know but it can make people feel woozy, sluggish etc. Because of this neurologists usually recommend you take it at night. If you have problems falling asleep it can help with that. Best of luck, vicki"
Vicki wrote on April 12th 2011: "I take Neurontin (gabapentin is generic, Neurontin is brand) for back pain and fibromyalgia. It doesn't do much for my rosacea pain. However, everyone is different as you know so it might help you. It is non addictive as far as I know but it can make people feel woozy, sluggish etc. Because of this neurologists usually recommend you take it at night. If you have problems falling asleep it can help with that. Best of luck, vicki"And Vicki updated on April 12th 2011: "WC and Nat, you are making me wonder if gabapentin (neurontin) started all this for me in the first place. Have been taking it for a few years (began late 2008 for back pain) and my rosacea started in summer 2010. Normal skin before that, just really fair-skinned."
"I can tell you my experience with neurontin"
Fauxmccoy wrote on May 1st 2014: "I can tell you my experience with neurontin. It is a very old and relatively very safe drug. It was prescribed to me by my pain doc and I took it for 6 months and later for 3 months. I have severe nerve damage from having a nerve cell tumor removed from my chest cavity. The tumor was attached to my heart, lung and spine and a lot of healthy nerve tissue had to be removed as well to remove the entire tumor. It left me with neuropathy. I still have severe pain at the surgical sites. places that are completely numb also with a left arm and leg that do not always comply exactly with what they are being told to do. I do know that most people who try neurontin do experience relief -- i was not one of them. In fact, I had to discontinue the med due to side effects/allergy which is fairly rare. This drug might be very helpful to you, I would encourage you to try. If you do experience any severe side effects, then you can discontinue. I found no ill effects from sudden stoppage on my doc's advice. It really does help a lot of people and you have little to lose. [..] I am surrounded by folks with very good experiences with it. My pain doc cannot speak highly enough about it and it is not because of sales reps. This is a very old drug and no one's 'pushing' it any more, it has simply built a reputation for being effective. My mom was for many years, the director of nurses at the rehab hospital where my pain doc works. In her many years on the job, she formed a very positive opinion on how patients experienced relief with neurontin. Long before I was with my current pain doc (living in a different city), my mom actually pressed me for info such as 'why isn't your doc putting you on neurontin, it is absolutely the first line for what you are dealing with ... blah blah blah (you know how moms are). Also, I attend a regular swim class at the rehab hospital with my fellow fibromyalgia sufferers. Many of them have experienced relief with neurontin. as I said, I am literally surrounded by folks who have nothing but great things to say about it. My negative personal experience is very rare."
Ben1992 wrote on July 26th 2013: "Any pain medications for painful burning/stinging flushes? -Hey there guys. Haven't posted on the forum in a little while. I live in the UK and naturally my rosacea is much better in the summer months so I tend to live my life a lot more instead of keeping coming to this forum for help with my flushing and painful sensations that arise from the flushes. Last year I visited Dr Chu. He prescribed me remeron, clonidine, and after a little while also mepacrine. This was in the winter these meds were prescribed. They had somewhat of an effect but nowhere near enough of an effect to completely stop the painful burning sensations in my cheeks. Also the mepacrine made me bright yellow after a little while and I do not think this was a good trade off for only a LITTLE bit of improvement of my flushing and associated pain. I am currently anxiously awaiting the winter months yet again, as I do not want to be in pain for another 6 months over the colder months constantly trying to calm my cheeks down. Would I would like to know is the following. Is there a painkiller that can effectively stop the painful burning sensations? I do not care if my cheeks are visibly flushed, it is just the intense pain that I want gone. Please help! In this day and age with medical technology so advanced there must be at least a pain medication that could stop painful burning sensations in my cheeks. I am also going to ask Dr Chu this same question, but I would like to get some thoughts and advices off of here first. Thanks guys, Ben."
Wendykay replied on August 13th 2013: "Hello, I have tried several pain medications but non of them work. I am currently taking low dose Cymbalta for depression in the hopes that it will also help with the burning. It has not! When I asked my derm whether the continuous pain causes damage, she said no. I was worried about this because I would hate to think that my skin is continuously being damaged by all of the burning. If I find something that works I will most certainly share it with you. I hope you will do the same. Many thanks, wendykay"
JayBee201 replied on September 5th 2013: "I have the same thing.. stinging and burning and sooooooo painful! I must be the only one whose rosacea gets worse in the summer! The heat and humidity are the worst on my face! If I go in the sun or a hot car .. that's it, I'm RED for days! I used to love going to the beach, now I'm a hermit"
Hg24 replied on September 16th 2013: "I had success with Zoloft, an SSRI antidepressant. Others here have also used SSRIs for flushing and burning. It calms the nervous system, including the nerve endings in your skin. It took about 6-8 weeks to feel relief. After the next year, the doc and I increased the dose some more. It's been very helpful in calming my skin and calming my anxiety caused by my skin. Also, make sure your skin is well hydrated. A good, simple moisturizer one the skin during as much of the day as possible. I've been having great success with an eczema cream - Neosporin Eczema Essential Moisturizing Cream - NOT the one with the steroid. It's a basic cream for restoring the skin barrier. Active key ingredient is colloidal oatmeal. I put a fairly generous layer on at night. I often have it on throughout the day when I'm home. It has really helped with strengthening my skin. Also, skin that is dry is more prone to reactivity, flushing and burning. So keeping your skin well moisturized really should help. Drink lots of water, too. Hope this helps!"
Paperbag wrote on January 9th 2015: "Neurontin causing flushing - Hi, I've just recently started taking Neurontin for nerve pain. I've been waking up with severe flushes on some days, but not others. I don't take the Neurontin every day. I am not sure, but I think I'm on to something. I take the Neurontin at night, because it helps me sleep. I think I wake up with flushing only when I take neurontin the night before. Has anyone else had bad flushing when taking Neurontin? I want to make sure I'm not crazy. Thanks board for any advice. I have not flushed in months. Please if anyone has any experience with Neurontin and flushing, please reply. I really need advice. Thank you"
Birdie replied on January 9th 2015: "Yes. I had a compound cream for nerve pain that included neurontin. After many months I realized the flushing, hot face in the morning may be related. I stopped the compound cream and the flushes subsided. No, yer not crazy! Birdie"
 Paperbag replied on January 9th 2015: "Thanks Birdie. I won't take the Neurontin tonight, and pray I wake up without flushing. I really hope that was the cause. I'm so glad I found some posts here about Neurontin causing vasodilation. I did then look at the prescribing information for Neurontin, and it does says vasodilation happens in 1% of people. I couldn't deal with my rosacea coming back full force after 2 purpuric v-beams and 1 non-purpuric v-beam. I just had a purpuric v-beam in October."
Paperbag replied on January 9th 2015: "Thanks Birdie. I won't take the Neurontin tonight, and pray I wake up without flushing. I really hope that was the cause. I'm so glad I found some posts here about Neurontin causing vasodilation. I did then look at the prescribing information for Neurontin, and it does says vasodilation happens in 1% of people. I couldn't deal with my rosacea coming back full force after 2 purpuric v-beams and 1 non-purpuric v-beam. I just had a purpuric v-beam in October."
"Going to try Oracea and Gabapentin"
Panacea wrote on July 11th 2008: "Going to try Oracea and Gabapentin - I was diagnosed in Feb 2008. Had a very quick onset brought on by a reaction to a moisturizer. Oddly, I've never had any flushing issues before the onset. Currently, my symptoms are moderate burning/stinging and mild flushing. My nose is the worst followed by cheeks and chin. Sometime I get it on my neck also. More recent is the p&p. They are worse around my mouth and chin, but smaller ones are starting to develop on my cheeks and nose. My doc also agreed to an Rx for Gabapentin (Neurontin). When I took it for the first time last night, I had stomach upset and very bizarre dreams, but it was tolerable. It does build up in the system over time, so we'll see how bad the side effects get compared to the pain relief. I will post updates over the next few weeks. Melissa" [Scarlet Nat: Melissa also started Oracea - low dose doxycycline - at the same time]Lakan replied on July 16th 2008: "Good luck with your treatment. If the gabapentin doesn't help or if you get a of of side effects then Lyrica (pregabalin) may be better. It's like a "newer and better" version of Neurontin. I think the chemical structure of those drugs are quite similar. You usually get good results on very low doses and I don't feel any side-effects at all from the Lyrica. Just wanted to tell you so you know that there's alternatives to the Neurontin but I hope you will be doing good on it now that you're on it."
Panacea replied on July 19th 2008: "Red face getting some relief - Well, it's been one week. I do feel better. The burning has calmed down some, and there is less redness. The p&p is about the same [..] I may discontinue the Oracea since I don't want to be doing too many things at once, and won't know what is helping/not helping. I'm am grateful for a little relief, but really hope I can find a natural alternative. We'll see. I'll update again soon. Melissa"
Willbill90 wrote on June 6th 2015: "Lyrica for burning - Has anyone here had any success with reducing the burning sensation using Lyrica?"
Samar2000 replied on June 6th 2015: "Tried it, but didn't help at all for me. Now I'm using remeron which helps."
J-Mill wrote on April 24th 2008: "If burning pain is really bad I can tell you that some people have success with using certain prescriptions meds like: amitriptyline - an anti-depressant at high doses but prescribed in low doses for pain, is apparently especially good respecting skin pain, it used in shingles treatment and has been prescribed for Rosaceans with burning/stinging. Gabapentin (neurontin) - Anti-seizure med that is used to treat nerve pain including facial pain/stinging, also used for shingles. Has been used off label for neuropathic pain associated with Rosacea. Pregabalin (Lyrica) - See Gabapentin, slightly different drug, more effective at lower doses."
J-Mill wrote on April 24th 2008: "If burning pain is really bad I can tell you that some people have success with using certain prescriptions meds like: amitriptyline - an anti-depressant at high doses but prescribed in low doses for pain, is apparently especially good respecting skin pain, it used in shingles treatment and has been prescribed for Rosaceans with burning/stinging. Gabapentin (neurontin) - Anti-seizure med that is used to treat nerve pain including facial pain/stinging, also used for shingles. Has been used off label for neuropathic pain associated with Rosacea. Pregabalin (Lyrica) - See Gabapentin, slightly different drug, more effective at lower doses."
"One of the most horrible things I experience are these bizarre burning and stinging sensations"
Bailey0397 wrote on July 15th 2009: "stinging sensations please some advice - One of the most horrible things I experience are these bizarre burning and stinging sensations. I don't have to be in a flush to feel them. In some areas they can feel like someone is sticking a needle in my face. Also the areas right next to my nose have very enlarged pores are oily and sting. Is this seb derm even though no flakes? Is this just a symptom of swollen blood vessels, an allergy,or nerves in my face acting crazy? Has anyone felt this and found some answers or ways to relieve it because it is really disabling and so hard to live every day with this pain for 2 years!!! I am at the end of my rope. I know people have flares and periods of relief, I have this every day. Sometimes I believe it is actually driving me crazy. The docs just say sensitive skin, this is not just sensitive skin it is completely abnormal. I don't know what my next step should be and I really could use some advice. Thanks for any suggestions. Bailey"
Melissa W replied on July 15th 2009: "Hi Bailey, I am sorry you are suffering with this as the burning sensation can be very painful and debilitating. What treatments have you tried? There are some meds that can help with these sensations like Remeron and clonidine. There are also laser treatments (yag 1064 and VBeam) that may help with the burning sensation. Lastly, red light therapy may be helpful as well. Unfortunately it will come down to trial and error to find what may provide you with relief. I hope you find something that helps soon and hang in there! Best wishes,
Melissa"
RedFaced replied on July 15th 2009: "I suffer from the neuro type pain as well and it is terribly debilitating. Take the advice above and find a good Dr. that has experience with treating complex regional pain syndromes. I take Lyrica (Pregabalin) and it has helped with the neuro/burning pain, has not gotten rid of it but taken the edge off. I also take Oxycodone which helps too, but this is an opiate and best avoided if possible but it helps the most out of the heavier painkillers. I have tried several painkillers including Morphine but some, like Morphine, have a histamine release and made me flushy. Oxycodone does not make my flush if I keep it under 10mg per day. I am also doing Acupuncture (only 2 weeks in) and have felt some pain relief and benefit (face is not as tight feeling for a few days following the treatment). Clonidine will not help with pain I don't think, it didn't at least for me, unless your pain is solely based on flushing in which case it could help in that respect. Diet is also huge and you can eliminate a lot of inflammation with diet changes, although you need to be strict. Search "Anti-inflammatory diet" and "Anti-yeast/candida diet". These are generally healthier diets that consist of lots of fresh veggies, organic fish, chicken, rice and oils such as extra virgin olive oil and unsalted clarified butter. Hope this helps."
Googoo replied on July 15th 2009: "Hi Bailey, Low dose accutane (10mg every other day) was the only drug that stopped the debilitating burning sensations that accompanied my rosacea. I also experienced stinging and stabbing sensations. I also had a problem with sensations of extreme tightness. Sometimes it felt like I was wearing a mask. My lips would also burn just like my face. I experienced these symptoms without any signs of redness, or flushing. While my face looked normal, it definitely did not FEEL normal. Accutane completely altered the inflammatory process of my disease. I'm extremely thankful that I have a derm who is knowledgeable about low dose Accutane as a treatment option for recalcitrant rosacea. This drug has given me part of my life back. I hope you find a treatment option that will work for you. Good Luck!! Kim"
Bailey0397 updated on July 15th 2009: "Redfaced, thank you so much! This is the first time that anyone has suggested some kind of pain medicine and it is a great help to me to get this information. I should definitely try to find a pain specialist or neurologist to help with this. Just to get some relief would be amazing. One question about the acupuncture do they put the small needles in your face or some other part of your body? Do you have a lot of broken vessels and thread veins like I do? Thanks so much for the suggestions and I am so happy to hear acupuncture is helping you! I'm with you I know how bad the pain can be. Thanks again, Bailey"
 Squirrelgirl6 replied on July 17th 2009: "You've described my face exactly Bailey! - Dear Bailey, just logged on to read more of the forum and saw your post re. burning agony pain continually on your face even when not flushing. That is me!!!!!!!!! You are soooo not alone because I have that exact very same feeling ALL the time and I feel like I'm going to go mad. I have a face full of red broken capillaries all over..my nose, cheeks and chin. Blotchy red marks and it looks awful and I can't even tolerate a tiny amount of cover up or even moisturizer. I use mineral water on my eyes only and that's it. I used to be 'product Queen' so for me this is devastating. I cannot remember what it's like to not have stinging skin!!! Something anyone with 'normal' skin takes for granted. I look at people around me etc and would give anything to be them...to experience a normal face that doesn't burn. Like you, I had the most amazing year in 2007. My best yet. I was incredibly happy, great skin, could wear makeup, dye my hair its beautiful blonde colour and had no issues what so ever with my skin/allergies etc. The last 2 years have been HELL ON EARTH!!!!! How did this all happen???!!!! I think that my burning skin will never go because no docs have been able to diagnose properly/treat/ help...... I cry every day as I cannot stand the pain anymore. I have very itchy skin around my nose crease, my forehead gets very itchy n' burns like Hell. I have to pin my fringe back as the hair brushing on my skin makes it worse. I was on some antifungals for 2 weeks and during that time I did notice my forehead wasn't as itchy and things settled a bit. I thought that the tablets didn't do anything but now my skin is horrendously sore again....so looking back I did get a brief time of relief. However, IF it was the anti-fungals that helped, obviously you can't stay on them for the rest of your life!!!!!!!! So, what do you do? It's a total and utter living nightmare that you can't seem to wake up from isn't it?! I have huge sympathy for you as I am right there with ya on the burning face 24/7. It is nice to know you're not alone and that someone somewhere else in the world is going thru' exactly the same thing. I feel like a freak!!! No one I know has this. I am so jealous of my friends who can wear makeup and get dressed up to go out, looking so pretty. I used to do this to. Now I don't see anyone except my brothers and VERY close friends who don't judge and love me for me. I'm so scared for my future. I'm only 35 and want to live my life but feel like I just want to be a hermit now. I send biggest hugs. Sorry I can't offer much help except that I am going through it too. We have to be strong together and take comfort in that. and NEVER NEVER NEVER give up."
Squirrelgirl6 replied on July 17th 2009: "You've described my face exactly Bailey! - Dear Bailey, just logged on to read more of the forum and saw your post re. burning agony pain continually on your face even when not flushing. That is me!!!!!!!!! You are soooo not alone because I have that exact very same feeling ALL the time and I feel like I'm going to go mad. I have a face full of red broken capillaries all over..my nose, cheeks and chin. Blotchy red marks and it looks awful and I can't even tolerate a tiny amount of cover up or even moisturizer. I use mineral water on my eyes only and that's it. I used to be 'product Queen' so for me this is devastating. I cannot remember what it's like to not have stinging skin!!! Something anyone with 'normal' skin takes for granted. I look at people around me etc and would give anything to be them...to experience a normal face that doesn't burn. Like you, I had the most amazing year in 2007. My best yet. I was incredibly happy, great skin, could wear makeup, dye my hair its beautiful blonde colour and had no issues what so ever with my skin/allergies etc. The last 2 years have been HELL ON EARTH!!!!! How did this all happen???!!!! I think that my burning skin will never go because no docs have been able to diagnose properly/treat/ help...... I cry every day as I cannot stand the pain anymore. I have very itchy skin around my nose crease, my forehead gets very itchy n' burns like Hell. I have to pin my fringe back as the hair brushing on my skin makes it worse. I was on some antifungals for 2 weeks and during that time I did notice my forehead wasn't as itchy and things settled a bit. I thought that the tablets didn't do anything but now my skin is horrendously sore again....so looking back I did get a brief time of relief. However, IF it was the anti-fungals that helped, obviously you can't stay on them for the rest of your life!!!!!!!! So, what do you do? It's a total and utter living nightmare that you can't seem to wake up from isn't it?! I have huge sympathy for you as I am right there with ya on the burning face 24/7. It is nice to know you're not alone and that someone somewhere else in the world is going thru' exactly the same thing. I feel like a freak!!! No one I know has this. I am so jealous of my friends who can wear makeup and get dressed up to go out, looking so pretty. I used to do this to. Now I don't see anyone except my brothers and VERY close friends who don't judge and love me for me. I'm so scared for my future. I'm only 35 and want to live my life but feel like I just want to be a hermit now. I send biggest hugs. Sorry I can't offer much help except that I am going through it too. We have to be strong together and take comfort in that. and NEVER NEVER NEVER give up."
RedFaced replied on July 17th 2009: "Thought I would just add that there is a name to what we are suffering from it is called "Subtype 5: Neuropathic Rosacea". This subtype can be combined with other subtypes or you can experience this subtype on its own (ie. neuropathic pain upon exposure to triggers with NO flushing or P&P's). [..] I struggled to find a derm that has even heard of this subtype but finally did. I have found some minor relief with the use of LYRICA as well as couple other painkillers. I am also doing Acupuncture for the pain and so far have felt some improvement for a couple days following. I can't stress how difficult this condition is to treat. As the article suggests, you really need to find an experienced derm who has at least heard of this subtype as well as a pain specialist (neurologist) who also has experience in treating complex regional pain syndromes of the face. I also suffer from flushing and swelling of the face and am trying a new medication from my derm that is sometimes used to treat certain types of Lupus. So fingers crossed. My advice is be persistent. You may need to go through trial and error both with Dr.'s and medications (as I did) to find a Dr. and combination that can at the very least take the edge off which it has for me - although I still have pain on a daily basis and still suffer from debilitating attacks upon exposure to certain triggers. Look into an anti-inflammatory diet as lactic acid can have a large influence on the nerves and lactic acid is high in areas of underlying inflammation/swelling such as the face. Stay strong and try to stay positive."
Bailey0397 updated on July 18th 2009: "Just found this: Alpha Lipoic acid. This antioxidant has long been used in Europe to treat symptoms of diabetic nerve disease. In a recent study at the Emory University School of Medicine, Atlanta, researchers reported that 300 mg of alpha-lipoic acid improved endothelial function by almost 50 percent, and the antioxidant also enhanced the benefits of a drug used to treat heart disease."
 Matos replied on October 19th 2009: "Hi! I am the new one in these forum. I come from Europe, but my English is so so. Ok, I have the same stinging complexion because I had one treatment in 2008 with Elos IPL and its been horrible. Before I didn't have any problem with rosacea. I have few capillaries and that is it. This Elos IPL is been very irritating for my skin, and is worsened my condition because I have more red veins and much more sensitive skin like before+stinging+sun sensitivity. Elos is big NO NO for rosacea.. Now how I am finding a good solution for my rosacea and capillaries. I don't have problem with P&P or acne only visible capillaries and stinging, burning sensation. I have 5x treatments with VERSA PULSE ND-yag LASER for visible capillaries on my forehead and nose."
Matos replied on October 19th 2009: "Hi! I am the new one in these forum. I come from Europe, but my English is so so. Ok, I have the same stinging complexion because I had one treatment in 2008 with Elos IPL and its been horrible. Before I didn't have any problem with rosacea. I have few capillaries and that is it. This Elos IPL is been very irritating for my skin, and is worsened my condition because I have more red veins and much more sensitive skin like before+stinging+sun sensitivity. Elos is big NO NO for rosacea.. Now how I am finding a good solution for my rosacea and capillaries. I don't have problem with P&P or acne only visible capillaries and stinging, burning sensation. I have 5x treatments with VERSA PULSE ND-yag LASER for visible capillaries on my forehead and nose."
Piscesblue13 replied on October 7th 2015: "I realize this is an old post but I have found it very helpful. Like many on here, I have been experiencing the stinging and burning for almost 5 months now. At first it was only a couple days a week and I thought I just washed my face too hard or something like that... I used proactive (wash and toner) for 13 years and was using retina micro for 3 years with NO problems and total success. But all of a sudden this past May 2015, things started to change and I noticed my skin became much more sensitive and much more oily. I have always had oily skin but suddenly it became like a faucet, combined with the burning and stinging, I didn't know what the heck was happening!! I gradually had to stop the proactiv and retin-a because I could not tolerate it at all. I know I have rosacea and was diagnosed many years ago but have never had any real issues with it. I also have finacea which I used to use as a spot treatment (along with my proactiv and retina micro) but I can barely use that. It's annoying because since my skin is so oily and I'm not really able to wash it, I am now breaking out in some tiny bumps as well as some pustules. I am now at my wits end and have been experiencing the pain everyday for the last 2 months. I have an appointment with a dermatologist and neurologist next week but i am scared at what they might say or recommend. I am currently taking Neurontin which helps dull the pain a bit but it definitely does not remove it. If anyone still reads this post I wood love to hear some feedback from others. This is truly the most debilitating thing--just doing small things like eating, showering, walking, cause me great pain.... :::sigh:::"
Piscesblue13 wrote again on December 12th 2015: "Treatment options for constant burning and stinging? - I am writing because over the last several months I have developed constant burning and stinging on my face. I was diagnosed with rosacea (which I knew I had but haven't had any issues with it for over 15 years) but doctors seem stumped as to what to do with me in terms of the pain. I am currently taking neurontin which helps but doesn't take away the pain. I read on some other posts about people's experiences with low dose accutane helping the burning and stinging--is there anyone out there who has had success with this treatment and could respond? I would love to hear any and all suggestions as I am really starting to lose my mind. This is such a debilitating condition."
Hg24 replied on December 12th 2015: "Hi, I had burning and stinging. Zoloft helped me greatly. Burning was gone. Also, keeping your skin very well hydrated is important. Use a gentle moisturizer and drink lots of water. [..] It can reduce the flushing. Several members on the forum take antidepressants for their flushing and burning."
TinyDancer replied on December 13th 2015: "This is something I definitely want to keep in mind for further along if I don't recover or if my condition worsens. It's challenging to figure out the right ones. My neurologist prescribed Amitriptyline for my nerve pain. But, it can actually worsen flushing. Someone recommended lyrica. But, I am in a group for people with trigeminal neuralgia and while it helped some, it caused serious harm to others. So, I will continue gathering information from people's experiences and then bring the info to my neurologist. I will look into Zoloft. Thank you! I do remember you mentioning this before. It's helpful info."
AEB replied on November 15th 2016: "I sympathize greatly as I've been struggling with intense burning for about two years now (my face is inflamed but also flushes badly daily). I've tried many things--it seems like different things work for different people, and my derms say sometimes a combo of meds is needed. Things I've tried that haven't helped much are neurontin, lyrica, amitriptyline. Some help: fluoxetine, clonazepam, orap, clonidine, dapsone, doxy, 3 V-beams (still doing those). I'm currently on a crazy cocktail of meds, still looking for something with many drs (pain specialists, psychoderm, terms) that can really keep the burning down--I've frankly found it completely debilitating and keeps me home bound trying to avoid flushing pain. I'll let you know if I find something that works even better, and feels free to PM me as well if you'd like more details on things I've tried. Good luck! You're not alone!"
Hg24 replied on November 30th 2016: "Have you guys been reading the thread about the ketamine and amitriptyline ointment? Not sure if it will work for rosacea - people are still experimenting - but read the thread. If the ointment helps the burning pain of erythromelalgia, maybe it will help rosacea stinging/burning? Here's the thread link. In the meantime, I had some help from Zoloft. Anything you can do to calm inflammation is also helpful. Try zinc supplements; also zinc cream (diaper rash) or calamine lotion with zinc. The cream can be drying, so moisturize. Also, I cleanse my skin as little as possible. Instead I just rinse with cold water. [..] Lysine and MSM supps have helped some here. You can search the forum. I know how horrible the burning/stinging can be. You basically are trying to quiet the nerve endings, which are way overstimulated from flushing and inflammation. Check out the thread on the ketamine/amitriptyline ointment. It's a new discussion, but it might help you. Best of luck!"
Antwantsclear replied on December 30th 2016: "Stinging and burning reduced quite a lot for me just by not putting tap water on the rosacea affected areas (I wash them with mineral water instead). That is something you can do yourself without any help from the doctor. I found baths were better then you don't need to put your head under the water and can wash your face with mineral water instead. You don't want a very hot steamy bath either or the steam will rise up and affect your rosacea. I use a colloidal silver spray bottle which is quite helpful on the rosacea affected areas as well. [..] The anti-flushing medication will help to manage the rosacea overall which should help with the stinging and burning as well - clonidine or moxonidine, hydroxychloroquine, mepacrine, remeron, propranolol. I think hydroxychloroquine can be especially helpful to burning as it's an anti-parasitic drug, so helps to kill demodex mites (which cause the burning and irritation) as well as having other mechanisms to help manage the rosacea."
 Laser_cat wrote on November 4th 2018: "My derm who co-authored that paper linked by Nat, and has seen ~15 patients with neurogenic rosacea (he says it is obvious to him what is neuro vs vascular/ who would benefit from laser) says a lot of his patients are made worse by laser, if not triggered by laser. He doesn't know why. Maybe the settings were increased to something the patient couldn't handle. He strongly thinks that the redness seen in neuro patients - is the tip of the iceberg and its due to dysfunctional neuronal regulation and hyperexcitable sensory nerves. He has urged me to focus on treatments not that control the blood vessels, but that help calm the overactive nerves. After 2-3 years of obsessively reading + thinking about my symptoms, he has convinced me. I was later diagnosed via leg biopsy with small fiber neuropathy (non length dependent) -- the nerves degenerate for whatever reason, and become hyperexcitable as your body tries to grow them back (something like that). Usually small fiber neuropathy is associated with feet or hands (diabetes eg), but my derm thinks that this is what is going on with his neuro rosacea patients. Biopsies are only standardized in the leg (not face) so this cannot be confirmed (except sometimes if it is in the face or other areas, it will show up in the leg as well), but it would prove a sensory nerve dysfunction association and make sense. I would a rheum do a full workup, and ask for an SFN punch biopsy in a leg (derm or neuro can do this) + neurodiagnostic testing. Having a pos. SFN biopsy has totally changed the way I am having convos with my doctors for the better -- no one mentions anti-acne topicals etc and I have objective evidence of a pain condition. Sometimes the cause of SFN can be treated and symptoms cured (~50% of cases) eg b12 deficiency, hepatitis, lyme, sjogrens (lip biopsy is best for sjogren's .. sjogren's is the most common cause of non length dependent SFN). And new evidence says that in a significant minority of idiopathic SFN cases, they are "apparently autoimmune" without any autoimmune markers that we know how to detect, and will respond to aggressive immunotherapies like IVIG, steroids, plaquenil (something like inflammation is continually angering the nerves, triggering pain + dilation). [..] Imo, all the meds in that paper are worth trying. I get relief from cymbalta 80 mg in the morning, mirtazapine 22.5 mg at night (for sleep), zonegran (a sodium channel blocker and t type channel blocker ... stabilizes sensory nerves). Currently ramping up on the zonegran, trying IVIG (super anti inflammatory infusion), and low dose naltrexone in case i have autoimmune origin. If I fail IVIG, I probably will trial (oral or iv) steroids (my derm says a couple of his neuro patients do respond to, though it's tricky because they can cause flushing as a side effect). I see a pain doc and we are working to get lidocaine infusions every other day approved by my insurance to "reset" the nerves (lidocaine is the best thing i have found that makes me more heat tolerant ... acts on nerves, but blocks pain and flushing both). If that doesn't work, then maybe ketamine iv's. I think a pain doc can be great, but might not be worthwhile if you have not yet tried the first line treatments like amitriptyline, cymbalta, gabapentin, lyrica. Basically I just want to say, there is hope and many things your mom can try -- I wish someone had told me that when i thought treatments were limited to soolantra and gabapentin. Bless you for trying to help your mom. I feel for you both. Good luck and keep us updated. PS - i really think neuro rosacea is another word for facial erythromelalgia. All the stuff out there on erythromelalgia applies."
Laser_cat wrote on November 4th 2018: "My derm who co-authored that paper linked by Nat, and has seen ~15 patients with neurogenic rosacea (he says it is obvious to him what is neuro vs vascular/ who would benefit from laser) says a lot of his patients are made worse by laser, if not triggered by laser. He doesn't know why. Maybe the settings were increased to something the patient couldn't handle. He strongly thinks that the redness seen in neuro patients - is the tip of the iceberg and its due to dysfunctional neuronal regulation and hyperexcitable sensory nerves. He has urged me to focus on treatments not that control the blood vessels, but that help calm the overactive nerves. After 2-3 years of obsessively reading + thinking about my symptoms, he has convinced me. I was later diagnosed via leg biopsy with small fiber neuropathy (non length dependent) -- the nerves degenerate for whatever reason, and become hyperexcitable as your body tries to grow them back (something like that). Usually small fiber neuropathy is associated with feet or hands (diabetes eg), but my derm thinks that this is what is going on with his neuro rosacea patients. Biopsies are only standardized in the leg (not face) so this cannot be confirmed (except sometimes if it is in the face or other areas, it will show up in the leg as well), but it would prove a sensory nerve dysfunction association and make sense. I would a rheum do a full workup, and ask for an SFN punch biopsy in a leg (derm or neuro can do this) + neurodiagnostic testing. Having a pos. SFN biopsy has totally changed the way I am having convos with my doctors for the better -- no one mentions anti-acne topicals etc and I have objective evidence of a pain condition. Sometimes the cause of SFN can be treated and symptoms cured (~50% of cases) eg b12 deficiency, hepatitis, lyme, sjogrens (lip biopsy is best for sjogren's .. sjogren's is the most common cause of non length dependent SFN). And new evidence says that in a significant minority of idiopathic SFN cases, they are "apparently autoimmune" without any autoimmune markers that we know how to detect, and will respond to aggressive immunotherapies like IVIG, steroids, plaquenil (something like inflammation is continually angering the nerves, triggering pain + dilation). [..] Imo, all the meds in that paper are worth trying. I get relief from cymbalta 80 mg in the morning, mirtazapine 22.5 mg at night (for sleep), zonegran (a sodium channel blocker and t type channel blocker ... stabilizes sensory nerves). Currently ramping up on the zonegran, trying IVIG (super anti inflammatory infusion), and low dose naltrexone in case i have autoimmune origin. If I fail IVIG, I probably will trial (oral or iv) steroids (my derm says a couple of his neuro patients do respond to, though it's tricky because they can cause flushing as a side effect). I see a pain doc and we are working to get lidocaine infusions every other day approved by my insurance to "reset" the nerves (lidocaine is the best thing i have found that makes me more heat tolerant ... acts on nerves, but blocks pain and flushing both). If that doesn't work, then maybe ketamine iv's. I think a pain doc can be great, but might not be worthwhile if you have not yet tried the first line treatments like amitriptyline, cymbalta, gabapentin, lyrica. Basically I just want to say, there is hope and many things your mom can try -- I wish someone had told me that when i thought treatments were limited to soolantra and gabapentin. Bless you for trying to help your mom. I feel for you both. Good luck and keep us updated. PS - i really think neuro rosacea is another word for facial erythromelalgia. All the stuff out there on erythromelalgia applies."
"Neurogenic rosacea turned out to be Lyme disease"
Kittydoc wrote on August 15th 2017: "Neurogenic rosacea turned out to be Lyme disease - Hi all, I posted for the first time a few months back about my neurogenic rosacea and wanted to come back with an update. A brief history - I developed extreme facial burning and redness over the course of one day out of what seemed to be nowhere. Thus began my nightmare. Although the redness has almost completely resolved (other than a faint blush over the bridge of my nose and my upper cheeks) the burning has continued. As I reported previously, to the casual observer I probably appear normal. The burning was constant at first, but now has become more random. It flares for a few days and then calms down, only to flare a week later (or less). Sunlight and computer screens are my two big triggers. If I'm not in a large hat and wearing 50 spf or more when I leave the house my skin reminds my of my error later on in the day. I was instantly diagnosed with Rosacea, and later diagnosed with neurogenic Rosacea. I tried several treatments from 2 different derms (metrogel, solantra, etc) but they didn't help at all. One derm recommended I try an SSRI or an anti-seizure med since this form of the disease is sometimes responsive to those. Tried one dose of Lexapro and ended up having a massive panic attack. I haven't been the same since that panic attack. For whatever reason this episode led to a generalized anxiety disorder. I was put on xanax and told I should try another SSRI (ummm, no way). I next started experiencing horrible insomnia and getting weird muscle twitches and spasms. All in all, I ended up seeing 2 GP's, 2 derms, 2 naturopaths, a chiropractor, and an acupuncturist before getting to the root problem. After doing my own research I came up with Lyme. I asked one of the naturopaths to test me and I came up positive. I started treatment today. I'm coming back to this board because I'm hoping to reach anyone out there that has the neurogenic form of the disease, especially people that have just started having similar symptoms, or for those that experience any symptoms beyond the skin in association with their Rosacea. I spent the better part of year thinking I had Rosacea when I didn't. My treatment for Lyme has been delayed since everyone kept chalking it up to stress and Rosacea. I know that it's definitely more of an out there diagnosis for Rosaceans, but I wanted to put it out there in case my story helps anyone. [..] I had the Igenex IGg/IGm and and IFA performed. They don't look directly for spirochetes, but tend to use antibody/PCR/IFA. Lyme disease, especially when it's been longer than the acute phase of 6-8 weeks can sometimes be a bit difficult to diagnose - so much so that some doctors feel comfortable diagnosing Lyme disease based entirely on clinical signs. Most doctors (unless they are what the lyme community calls lyme literate doctors) won't treat you without a positive blood test. Fortunately - or unfortunately depending upon how you look at it - my IGg and IFA was positive. My doctor is convinced the phantom burning in my face, along with the sensitivity I've experienced is due to a neuropathy caused by Lyme attacking my nervous system. My symptoms seem to be neural and digestive so far - although the digestive is likely due to inappropriate neural stimulation too. My treatment consists of two antibiotics, doxycycline and Augmentin. I am also on a variety of supplements to to support my gut health, detox from the lyme die off, and prevent yeast overload from the chronic antibiotics. This will go on for months at a minimum. If I don't respond well to the orals he mentioned placing a port for IV antibiotics. There are also more unconventional treatments out there such as Vit C IV infusions and UV treatment. I'm just starting to get myself educated about this disease, so I don't know all the ins and outs yet. I've just joined a support forum like this one for Lyme. It's a real drag going from one chronic crappy disease which is poorly understood to another chronic crappy disease which is poorly understood, but at least I have an accurate diagnosis now. Kittydoc"
Babadah replied on August 15th 2017: "Ok thanks. And do you remember being bitten by a tick?"
Kittydoc replied on August 16th 2017: "Yes, I remember. I didn't think it was a deer tick at the time. I also didn't get a classic rash or feel sick after the bite. I now know that 50% of people don't remember getting bit when they come up Lyme positive. Now that I know better I wish I would have checked it out. Live and learn I guess. Kittydoc"
Fiugs replied on July 2nd 2018: "Hi.. I think my rosacea might fall into the neuropathic/neurogenic category.. although that’s my take on it, as all the docs and derms I've seen are pretty rosacea ignorant (but that’s another story). It was suggested to me by a friend in the US that I test for Lyme disease because a friend of hers had it and it presented as rosacea symptoms... so, for sure, there are others out there who seem to be in the same situation as you. As for myself, I haven’t been tested for Lyme... but my rosacea is improving on an almost daily basis since I started trialing low dose naltrexone 3 months ago. LDN is known to work for chronic stage Lyme disease as well as a host of other conditions. I don't know if I contracted Lyme disease, I haven’t been tested... but I live in the country and would be surprised not to have been bitten at some point.. I also traveled to rural NY state (which seems to be the Lyme-tick capital of the world!) twice a year for several years before my rosacea kicked in.. so it’s a thought.... No need for me to test for Lyme now I would think, as the LDN seems to be helping with all my symptoms at once. My terrible, almost constant face pain, burning and tingling stopped within 24 hours of my first LDN dose." Read more on rosacea turning out to be Lyme disease in this forum post.
"Facial burning w/ little to no redness?"
Meg101 wrote on May 25th 2018: "Facial burning w/ little to no redness? - Can this happen? I have it mainly on my cheeks and chin area, and I honestly don't know what to do. It feels so uncomfortable Please help"
 Laser_cat replied on May 25th 2018: "Is this a consequence maybe of repeated flushing and sensitized nerves? Eg, perhaps originally you could flush without much burning, but now it only takes *a little* redness / blood vessel jumpiness to make the nerves angry? Do you ever have tingly / stabbing / pins and needles sensations (I think the more specific you can be to a derm, the more helpful they can hopefully be). The nerve pain is tough to treat. But there are lots of things to try. I think that in addition to treating the flushing, it's a good idea to have something that also helps with the nerves directly because these things can quickly get a life of their own + harder + harder to treat with time. The more I read about chronic pain / neuropathic pain / related pain conditions the more questions I have lol but this seems to be the clear message. Unfortunately lots of options have side effects that are less than optimal but everyone's different in that regard. I do think though that once you get a handle on it, then maybe you can slowly pare back, and maybe your body will "forget" about those pain circuits. I'm really sensitive to anything that affects cognitive function -- One thing that helped me a lot was alpha lipoic acid. Unfortunately this had other side effects for me (hair loss + insomnia) but seems like most ppl don't. Took a few weeks for me to notice a difference. Many "natural" anti-pain or anti-inflammatories are dilating so be careful.
Laser_cat replied on May 25th 2018: "Is this a consequence maybe of repeated flushing and sensitized nerves? Eg, perhaps originally you could flush without much burning, but now it only takes *a little* redness / blood vessel jumpiness to make the nerves angry? Do you ever have tingly / stabbing / pins and needles sensations (I think the more specific you can be to a derm, the more helpful they can hopefully be). The nerve pain is tough to treat. But there are lots of things to try. I think that in addition to treating the flushing, it's a good idea to have something that also helps with the nerves directly because these things can quickly get a life of their own + harder + harder to treat with time. The more I read about chronic pain / neuropathic pain / related pain conditions the more questions I have lol but this seems to be the clear message. Unfortunately lots of options have side effects that are less than optimal but everyone's different in that regard. I do think though that once you get a handle on it, then maybe you can slowly pare back, and maybe your body will "forget" about those pain circuits. I'm really sensitive to anything that affects cognitive function -- One thing that helped me a lot was alpha lipoic acid. Unfortunately this had other side effects for me (hair loss + insomnia) but seems like most ppl don't. Took a few weeks for me to notice a difference. Many "natural" anti-pain or anti-inflammatories are dilating so be careful.
-SSRI (or cymbalta) paired with a different kind of antidepressant (has helped me a lot)
-gabapentin / lyrica / baclofen / memantine / oxtellar / ranexa / mexiletine / amitriptyline / etc -- out of all these I'd say lyrica, ranexa, mexiletine have the fewest side effects
-clonazepam / xanax as needed -- very helpful for me
-daily aspirin might be helpful -- give it a month or so before giving up
-magnesium -- it can be dilating + relaxes muscles, but if your nerve pain comes from nerves not getting appropriate nutrients / oxygen, this can be helpful. If this is helpful (or not hurtful), than a prescription low dose (long-acting) calcium channel blocker might be even better.
-butterbur, feverfew, ginger -- "natural" migraine remedies, in case the pathophysiology is similar.
-topical analgesics -- 0.5% amitriptyline eg (careful cuz i think all topical analgesics are dilators .. but worth a try. little to no systemic side effects)
off-the-menu things --
-infusions (lidocaine, ketamine, etc) can interrupt a 24/7 pain cycle. Can be followed with mexiletine (oral lidocaine analog) for longer analgesic effects
-botox
-nerve blocks (these are not permanent, can be very helpful in conditions like CRPS/hot flashes/depression/etc particularly if the pain is sympathetically mediated)
miscellaneous --
-visual imagery techniques - visualize your pain neural circuits shrinking (do this while you have pain). your body image (in your mind) can be surprisingly in sync with your actual body. Pain is not wholly driven by sensory input if that makes sense
-Acupuncture
-red light therapy -- stop immediately if burning intensifies
-meditation
I hope you get relief soon for yourself. My main point is that there are a lot of different things to try and you aren't alone. I'd be very surprised if you couldn't find anything to at least give you partial relief but it takes time."
Meg101 replied on May 25th 2018: "Thank you so much for your response! I very much appreciate it. Btw do you consider your rosacea to be neurogenic or neuropathic? Are these terms interchangeable? However, upon first course of action do you think I could benefit from propranolol and mirtazapine at nigth? Adding on to the fact that I am dealing with a lot of anxiety anyway:/ Also what does "pain is sympathetically mediated" mean?"
Laser_cat replied on May 25th 2018: "Yea mirtazapine + propranolol first sounds like a good plan (and maybe you only need the one!) Stagger start dates so you know which one is working / giving what side effects I'd probably give mirtazapine 3-4 months until you call it a failure + propranolol 6 weeks (just based on what my derm says and what I've read). I and others I know have noticed mirtazapine benefit 3-4 months down the road even though it is supposed to kick in much faster than SSRI's. I am reallllllly not a dr nor an expert in any of this ;) However I do think that derms aren't too knowledgeable in pain stuff + so I have been trying recently to read up and consult with dr google (har har). The paper on neurogenic rosacea as a separate subtype (the one by Scharschmidt et al) I think purposefully skims the surface and omits any pathophysiology. Boundaries between pain types/definitions seem to overlap but I think neuropathic pain falls under the umbrella of neurogenic pain. Neuropathic pain is when there's damage to peripheral/central nervous system (even when there's no painful stimulus). Sympathetically maintained pain is part of neuropathic pain. I think what happens is that sensing nerves (feeding into the CNS) get sensitized more and more due to stuff (eg norepinephrine) released by sympathetic efferents (coming from the CNS). Things can be both sympathetically mediated and also have sympathetically independent mechanisms. When you block the sympathetic efferents, it can resolve sympathetically maintained pain (which can come back if you locally inject norepinephrine or something like that). I was reading the other day how fibro can be majorly sympathetically maintained, perhaps due to the hyper sympathetic nervous system in these ppl. I also was diagnosed with high blood pressure around my neurogenic rosacea onset so I think for me personally I might have an over active sympathetic nervous system (high bp is odd given my weight/age). (Sympathetic nervous system = "fight or flight"). A lot and most of this stuff is over my head lol. I believe what I have is neuropathic / neurogenic. The gabapentin / amitriptyline eg is mainly for neuropathic pain, I think. I also had a stellate ganglion nerve block recently which gave me a lot of pain relief (after the initial inevitable flushing from the sudden lack of norepinephrine (providing basal vasoconstriction)) -- tbd how long that will last. But I think this means that at least a good portion of my burning is sympathetically mediated. Sometimes they give a series to retrain the nerves Anyone who knows more, feel free to correct me / chime in."
Meg101 replied on May 26th 2018: "Wow thanks ! I will have to request my doc about them, hopefully she is willing, as this pain is very uncomfortable. Is the nerve block you got temporary? That is to retrain the nerves? Also on a day to day basis did you alleviate most of your pain? Do you still deal with the other Rosacea symptoms? Does your pain happen mainly when you flash or it’s just ongoing? Sorry for the overload of questions! The thing is I don’t have such noticeable redness yet the burning feeling is there."
Sg321 replied on May 26th 2018: "Effexor for nerve pain and flushing. - A few doctors have told me that Effexor can help with nerve pain, in addition to helping flushing. I started on the lowest dose last week, and am not expecting much until I get up to 75mg. Good luck."
Elmo replied on May 26th 2018: "I don't know the answer to your question but I've experienced something similar...... I've had odd pains and sensations (tickling, plucking, crawling twinging, zapping, corrosive flushes ) on my face for over a year now. 6 months ago started to get thread veins and follicular scale on cheeks. I've been treated for demodex with soolantra after ....now I'm left with the same sensations along with permanent pinkish cheeks, nose & chin. I don't think its the mites I can feel they are way too tiny. But perhaps they irritate the nerves? I suffered trigeminal neuralgia 15 years ago maybe that's connected in some way? I have lots of odd things going on with my body neurologically so maybe my nerves are all frazzled, but on the face its just so bothersome!!!!
-gabapentin / lyrica / baclofen / memantine / oxtellar / ranexa / mexiletine / amitriptyline / etc -- out of all these I'd say lyrica, ranexa, mexiletine have the fewest side effects
-clonazepam / xanax as needed -- very helpful for me
-daily aspirin might be helpful -- give it a month or so before giving up
-magnesium -- it can be dilating + relaxes muscles, but if your nerve pain comes from nerves not getting appropriate nutrients / oxygen, this can be helpful. If this is helpful (or not hurtful), than a prescription low dose (long-acting) calcium channel blocker might be even better.
-butterbur, feverfew, ginger -- "natural" migraine remedies, in case the pathophysiology is similar.
-topical analgesics -- 0.5% amitriptyline eg (careful cuz i think all topical analgesics are dilators .. but worth a try. little to no systemic side effects)
off-the-menu things --
-infusions (lidocaine, ketamine, etc) can interrupt a 24/7 pain cycle. Can be followed with mexiletine (oral lidocaine analog) for longer analgesic effects
-botox
-nerve blocks (these are not permanent, can be very helpful in conditions like CRPS/hot flashes/depression/etc particularly if the pain is sympathetically mediated)
miscellaneous --
-visual imagery techniques - visualize your pain neural circuits shrinking (do this while you have pain). your body image (in your mind) can be surprisingly in sync with your actual body. Pain is not wholly driven by sensory input if that makes sense
-Acupuncture
-red light therapy -- stop immediately if burning intensifies
-meditation
I hope you get relief soon for yourself. My main point is that there are a lot of different things to try and you aren't alone. I'd be very surprised if you couldn't find anything to at least give you partial relief but it takes time."
Meg101 replied on May 25th 2018: "Thank you so much for your response! I very much appreciate it. Btw do you consider your rosacea to be neurogenic or neuropathic? Are these terms interchangeable? However, upon first course of action do you think I could benefit from propranolol and mirtazapine at nigth? Adding on to the fact that I am dealing with a lot of anxiety anyway:/ Also what does "pain is sympathetically mediated" mean?"
Laser_cat replied on May 25th 2018: "Yea mirtazapine + propranolol first sounds like a good plan (and maybe you only need the one!) Stagger start dates so you know which one is working / giving what side effects I'd probably give mirtazapine 3-4 months until you call it a failure + propranolol 6 weeks (just based on what my derm says and what I've read). I and others I know have noticed mirtazapine benefit 3-4 months down the road even though it is supposed to kick in much faster than SSRI's. I am reallllllly not a dr nor an expert in any of this ;) However I do think that derms aren't too knowledgeable in pain stuff + so I have been trying recently to read up and consult with dr google (har har). The paper on neurogenic rosacea as a separate subtype (the one by Scharschmidt et al) I think purposefully skims the surface and omits any pathophysiology. Boundaries between pain types/definitions seem to overlap but I think neuropathic pain falls under the umbrella of neurogenic pain. Neuropathic pain is when there's damage to peripheral/central nervous system (even when there's no painful stimulus). Sympathetically maintained pain is part of neuropathic pain. I think what happens is that sensing nerves (feeding into the CNS) get sensitized more and more due to stuff (eg norepinephrine) released by sympathetic efferents (coming from the CNS). Things can be both sympathetically mediated and also have sympathetically independent mechanisms. When you block the sympathetic efferents, it can resolve sympathetically maintained pain (which can come back if you locally inject norepinephrine or something like that). I was reading the other day how fibro can be majorly sympathetically maintained, perhaps due to the hyper sympathetic nervous system in these ppl. I also was diagnosed with high blood pressure around my neurogenic rosacea onset so I think for me personally I might have an over active sympathetic nervous system (high bp is odd given my weight/age). (Sympathetic nervous system = "fight or flight"). A lot and most of this stuff is over my head lol. I believe what I have is neuropathic / neurogenic. The gabapentin / amitriptyline eg is mainly for neuropathic pain, I think. I also had a stellate ganglion nerve block recently which gave me a lot of pain relief (after the initial inevitable flushing from the sudden lack of norepinephrine (providing basal vasoconstriction)) -- tbd how long that will last. But I think this means that at least a good portion of my burning is sympathetically mediated. Sometimes they give a series to retrain the nerves Anyone who knows more, feel free to correct me / chime in."
Meg101 replied on May 26th 2018: "Wow thanks ! I will have to request my doc about them, hopefully she is willing, as this pain is very uncomfortable. Is the nerve block you got temporary? That is to retrain the nerves? Also on a day to day basis did you alleviate most of your pain? Do you still deal with the other Rosacea symptoms? Does your pain happen mainly when you flash or it’s just ongoing? Sorry for the overload of questions! The thing is I don’t have such noticeable redness yet the burning feeling is there."
Sg321 replied on May 26th 2018: "Effexor for nerve pain and flushing. - A few doctors have told me that Effexor can help with nerve pain, in addition to helping flushing. I started on the lowest dose last week, and am not expecting much until I get up to 75mg. Good luck."
Elmo replied on May 26th 2018: "I don't know the answer to your question but I've experienced something similar...... I've had odd pains and sensations (tickling, plucking, crawling twinging, zapping, corrosive flushes ) on my face for over a year now. 6 months ago started to get thread veins and follicular scale on cheeks. I've been treated for demodex with soolantra after ....now I'm left with the same sensations along with permanent pinkish cheeks, nose & chin. I don't think its the mites I can feel they are way too tiny. But perhaps they irritate the nerves? I suffered trigeminal neuralgia 15 years ago maybe that's connected in some way? I have lots of odd things going on with my body neurologically so maybe my nerves are all frazzled, but on the face its just so bothersome!!!!
 Laser_cat replied on May 26th 2018: "I have flushing + burning, onset very sudden, but I think the burning has gotten progressively worse when I was still scrambling to find meds/treatment that worked for me. I think this is the case with neuropathic pain -- can get progressively worse with time instead of resolving. It is interesting you say you have burning without much redness -- I don't relate to that too much I think, but I do remember one derm saying to me that laser might not have been effective for me bc the problematic areas could have been too deep (for the laser). Maybe you're similar in that way (so would look less red), but have no idea really. I think it might be a good thing you're not getting that red -- it might mean that you could be able to handle medication that helps with nerve stuff even if it will also dilate the blood vessels. If that makes sense.... since it seems like your blood vessels are already pretty stabilized more or less? I think I got pretty good benefit from amlodipine, effexor, mirtazapine, botox. I had this nerve block lined up for a while bc I wasn't expecting such a good result from amlodipine (I've since tapered off lyrica). I'm not sure if I'll continue the nerve block route, have to see how things continue to unfold maybe. (Mine was temporary, I'd never consider a permanent one.) Response times for temporary blocks seem to be patient-dependent. Good luck with everything."
Laser_cat replied on May 26th 2018: "I have flushing + burning, onset very sudden, but I think the burning has gotten progressively worse when I was still scrambling to find meds/treatment that worked for me. I think this is the case with neuropathic pain -- can get progressively worse with time instead of resolving. It is interesting you say you have burning without much redness -- I don't relate to that too much I think, but I do remember one derm saying to me that laser might not have been effective for me bc the problematic areas could have been too deep (for the laser). Maybe you're similar in that way (so would look less red), but have no idea really. I think it might be a good thing you're not getting that red -- it might mean that you could be able to handle medication that helps with nerve stuff even if it will also dilate the blood vessels. If that makes sense.... since it seems like your blood vessels are already pretty stabilized more or less? I think I got pretty good benefit from amlodipine, effexor, mirtazapine, botox. I had this nerve block lined up for a while bc I wasn't expecting such a good result from amlodipine (I've since tapered off lyrica). I'm not sure if I'll continue the nerve block route, have to see how things continue to unfold maybe. (Mine was temporary, I'd never consider a permanent one.) Response times for temporary blocks seem to be patient-dependent. Good luck with everything."
"End of the road? Cymbalta Lyrica"
Y-gwair wrote on June 20th 2011: "Help - intense burning pain? - I had a terrible flush while lying in bed yesterday morning, no idea what triggered it, but the intense burning pain has been unbearable ever since, even when the redness goes down. I have an appointment to see a specialist in August, but I can't possibly put up with this pain until then. Are there any treatments a GP can prescribe for intense neural pain? Would drugs like amitriptyline/tegretol have any effect ? I'm absolutely desperate now.
Meg wrote on June 20th 2011: "Sorry to hear you are having flushing with pain. I know exactly what you are dealing with as I suffer from severe flushing with pain for many, many years now. Your GP should be able to help you manage the pain in the short term, but you should also get testing for the various ailments that can cause flushing to make sure it's nothing serious. After that, you can try lots of medications to find out which ones help you. Most people start with clonidine, but amitriptyline helps some too. Tegretol is usually not a first option for this. But you could try neurontin or lyrica and they are known for working better with effexor or cymbalta. Another option is narcotics like Roxicodone or something long acting like Opana ER. Or you could also try some of the migraine medications like maxalt or treximet which work as vasoconstrictors, but you can't take them all the time. The best thing to do is to work with your dr to find the safest medication to try first and then work your way up to the medications that are less safe. I hope you find relief, Meg"
 Y-gwair wrote on March 9th 2012: "End of the road? Cymbalta Lyrica - I'm now at the end of the road with rosacea medications. Clonidine, mirtazapine, atenolol, labetalol, mepacrine have done nothing to halt the progress of severe flushing and increasing pain levels. I've just spent a month on full-dose Gabapentin (3600 mg a day) which did nothing for the scalding pain. Have also tried Tramadol and morphine given by GP, which didn't have any effect on it either. I am at the end of the road, I don't feel there is any point going back to my well-known Derm as none of his suggestions have worked at all, he couldn't actually look me in the face last time we visited, so I guess he has realised this approach has been a complete failure as well. Having assured me it was a self-limiting condition on our first consultation, I feel really angry and bitter that I was given false hope about this terrible condition. I'm currently looking at medications that treat severe neuropathic pain, Lyrica and hoping to try SNRI Cymbalta. I guess these are prescribed mainly for severe pain. Has anyone found that they have any effect on flushing, or do they just mask the pain? I'm not sure if there is anything left to try if and when these fail to work for my horrific pain and disfigurement."
Y-gwair wrote on March 9th 2012: "End of the road? Cymbalta Lyrica - I'm now at the end of the road with rosacea medications. Clonidine, mirtazapine, atenolol, labetalol, mepacrine have done nothing to halt the progress of severe flushing and increasing pain levels. I've just spent a month on full-dose Gabapentin (3600 mg a day) which did nothing for the scalding pain. Have also tried Tramadol and morphine given by GP, which didn't have any effect on it either. I am at the end of the road, I don't feel there is any point going back to my well-known Derm as none of his suggestions have worked at all, he couldn't actually look me in the face last time we visited, so I guess he has realised this approach has been a complete failure as well. Having assured me it was a self-limiting condition on our first consultation, I feel really angry and bitter that I was given false hope about this terrible condition. I'm currently looking at medications that treat severe neuropathic pain, Lyrica and hoping to try SNRI Cymbalta. I guess these are prescribed mainly for severe pain. Has anyone found that they have any effect on flushing, or do they just mask the pain? I'm not sure if there is anything left to try if and when these fail to work for my horrific pain and disfigurement."Y-gwair wrote on March 13th 2012: "Saw a pain specialist from St Mary's yesterday. Confirmed that the flushing and pain are almost certainly due to generalized autonomic nervous system failure, and will be incredibly hard to treat. Lyrica is probably the best hope; if that doesn't help, stronger opiates, and beyond that trying nerve blocks. I'm really quite disturbed this was misdiagnosed as Rosacea. I've now discovered I have postural orthostatic tachycardia (pulse/systolic BP shoots up when upright), which is also probably due to the underlying dysautonomia. Taking clonidine for months has masked these symptoms which hasn't helped, I'd assumed the worsening dizziness on standing over the last few months was a drug side effect of the various drugs I'd been taking. I'm seeing Professor Mathias, consultant in autonomic and neuro-vascular medicine at St Mary's on thursday, I'm hoping he can suggest something. I have been trying to explain that I had additional issues / symptoms to my derm, who persisted with the view that they were not relevant and that the condition was rosacea when in fact the symptoms I have been describing are equally consistent with a number of other more serious problems (including adrenal and carcinoid tumours, which should be ruled out where flushing is present with racing pulse and other hyper-adrenagenic symptoms)."
Y-gwair updated on March 19th 2012: "I saw Professor Mathias at St Mary's Hospital last week. After a thorough examination confirmed I have erythromelalgia, dysautonomia, Postural Orthostatic Tachycardia, and also hypermobile joints, suggesting the main underlying condition is Ehlers Danlos syndrome type 3. Not clear how Ehlers Danlos relates to the autoimmune issues, they may just be co-incidental. I'm also a bit annoyed none of the various rheumatologists I've seen picked this up either, EDS is supposedly within their field of knowledge. What I have is very difficult to treat as many of the things that might help the orthostatic problems may well make the facial erythromelalgia worse. It seems most people with EM end up on strong opiates. I will try sympathetic nerve block, but from what others have experienced they don't work terribly well for EM because of the vascular element of the pain. My real worry is that it is spreading to my feet, which go bright red and hot feeling if I walk for more than an hour, the soles have started stinging and toes feel like they have needles stuck in. If the pain gets as bad as the face, it will be impossible to walk and I'll be practically disabled by it. I've been titrating up the Lyrica, so far with zero effect. I doubt it's going to help at all."
Y-gwair updated on March 20th 2012: "[..] Doctors are so quick to assume that flushing is just rosacea, whereas I now know it can also be a symptom of serious systemic disease. Idiopathic POTS is quite common in young women too ( usually this form tends to remit with time) so if you are feeling dizzy or faint, or have any odd numbness or discomfort in your hands/feet/legs in addition to flushing, you should be investigated thoroughly for other conditions like POTs, diabetes, adrenal function, Mast Cell disease or carcinoid tumours."
Y-gwair updated on March 26th 2012: "[..[ He knows quite well that there is a condition called erythromelalgia, I told him many times that the burning was terrible. Maybe I was too polite and should have just sat there screaming, as that's literally what I've been doing virtually every night for the last year, and increasingly in public as the pain is excruciating and unremitting at times. Instead of continually reassuring us that it was definitely rosacea, that it would all get better once the clonidine, mirtazapine or whatever the next thing on the list was etc kicked in, he could have accepted the truth and referred to me to a specialist pain clinic sooner, rather than just telling me to take a single gabapentin tablet if I felt a bad night coming on (roll on the floor screaming). Erythromelalgia is a serious condition that is refractory to virtually every painkiller as I have now found out personally, leaving me somewhat bereft of hope. Beyond this point lie only stronger opiates (which I'm not sure I can tolerate, having had severe a urticarial reaction to morphine), and nerve blocks which can have unpleasant and unpredictable side effects and a poor track record in erythromelalgia anyway. Quite honestly, if the last couple of options fail to relieve the pain I will be seriously looking into a one-way trip to Dignitas in Switzerland as prospect of continuing to live with this much pain is unacceptable."
Y-gwair updated on April 10th 2012: "Just to update, I tried Duloxetine a week ago with disastrous results. Within 48 hours I developed terrible flushing in my face, and also in my tongue and palate, as if I'd eaten a mouthful of chili, and had to stop. Over the next 48 hours, I had terrible withdrawal symptoms, my hands, feet and tongue went into Raynaud's like vasospasm as the circulation cut off completely, so painful I couldn't walk and my tongue went numb and lost all sense of taste. My hands have become so painful it's virtually impossible to use my laptop because of the freezing metal casing. It's worn off a little over the last week, but I'm desperately afraid that the highly disabling severe Raynaud's may now be permanent. For some, Serotonin can be a powerful vasodilator and such drugs can potentially cause disturbance to the sympathetic nervous system with disastrous results. The same is also true of drugs like clonidine and beta blockers, which I believe triggered the Raynaud's in the first place which in turn seems to have triggered erythromelalgia in my hands and feet. Starving tissue of oxygen during vasoconstriction (hypoxia) in susceptible individuals with connective tissue disease can induce the opposite reaction of inn appropriate flushing."
Findingaway wrote on April 28th 2011: "Options for treatment of burning sensations: is there a natural treatment? - I have been experiencing an increase in burning sensations recently. For the last month, my chin has started burning and also both cheeks now, plus the last week my forehead. As mentioned many times on threads related to burning sensations, it is often seemingly not trigger related nor am I red. The burning can last for hours, days even. I have looked through many threads on this forum and found many possible treatment options, most are pharmaceutical and I wanted to avoid this if possible, although I must admit, the burning has been so frustrating that I was ready to get prescribed some Clonidine until I read a couple of rosaceans who have had bad experiences from it. Here is the list of possible medications/treatment options I found. They range from anti-depressants to blood pressure medications, NSAIDs and laser treatments. [..] The only thing I haven't tried is Aloe Vera or Borax (if you can call that natural). There must be more options??"
Melissa W. replied on April 29th 2011: "I'm sorry you are experiencing an increase in your burning symptoms. I know you mentioned RLT (Red Light Therapy) and that is the one treatment that really helped me re burning when I was dealing with flares. I haven't read your posts on your RLT experience but if you have not already done so I suggest using the red light in conjunction with your burning at a few minutes at a time and see if it helps decrease your burning sensation. With regards to why our face has the burning sensation I understand it is related to the blood flow irritating our blood vessels when it rushes into them during a flush. Why you may be experiencing it independent of a flush could be due to the vessels/nerves already being irritated from past flush reactions. Best,
Melissa"
Laser_cat wrote on February 18th, 2018: "My doctors wanted me to increase my my clonidine dosage because it is listed to help with facial flushing + menopause symptoms and it really does work very well in the short term. But in the long term I'm better off of it. Mirtazapine seems to be the antidepressant of choice on this forum, I think due to its antihistamine activity, but I don't think it's one-size-fits-all. Cymbalta might help more with the burning pain and calm the nerves (pain-modifying antidepressant) as well as increasing serotonin (+ norepinephrine) in the brain. Amitriptyline is also pain-modifying antidepressant and is a migraine med - I think migraines have a lot of similarity to what is going on with some of us (cerebral vasospasm .. where the vasodilation causes a lot of pain). I think it is fine to eventually stack some of these antidepressants (I take effexor + mirtazapine). Lyrica + gabapentin are used often for neuropathic pain + burning extremities (feet, hands, ears). Lyrica is helpful for my burning. Pizotifen blocks histamine + serotonin receptors in the brain (used for migraine, eg). Periactin is similar. Plaquenil is a solid anti-inflammatory (swelling). It doesn't help me much with the flushing or burning but it might be helpful if there are autoimmune issues. On my list still to try are baclofen, memantine, namenda, + retrying topical timolol. tldr I think there are lots of things to try. Look into drugs used for migraine, erythromelalgia, neuropathic pain (similar conditions imo)."
Melissa W. replied on April 29th 2011: "I'm sorry you are experiencing an increase in your burning symptoms. I know you mentioned RLT (Red Light Therapy) and that is the one treatment that really helped me re burning when I was dealing with flares. I haven't read your posts on your RLT experience but if you have not already done so I suggest using the red light in conjunction with your burning at a few minutes at a time and see if it helps decrease your burning sensation. With regards to why our face has the burning sensation I understand it is related to the blood flow irritating our blood vessels when it rushes into them during a flush. Why you may be experiencing it independent of a flush could be due to the vessels/nerves already being irritated from past flush reactions. Best,
Melissa"
Laser_cat wrote on February 18th, 2018: "My doctors wanted me to increase my my clonidine dosage because it is listed to help with facial flushing + menopause symptoms and it really does work very well in the short term. But in the long term I'm better off of it. Mirtazapine seems to be the antidepressant of choice on this forum, I think due to its antihistamine activity, but I don't think it's one-size-fits-all. Cymbalta might help more with the burning pain and calm the nerves (pain-modifying antidepressant) as well as increasing serotonin (+ norepinephrine) in the brain. Amitriptyline is also pain-modifying antidepressant and is a migraine med - I think migraines have a lot of similarity to what is going on with some of us (cerebral vasospasm .. where the vasodilation causes a lot of pain). I think it is fine to eventually stack some of these antidepressants (I take effexor + mirtazapine). Lyrica + gabapentin are used often for neuropathic pain + burning extremities (feet, hands, ears). Lyrica is helpful for my burning. Pizotifen blocks histamine + serotonin receptors in the brain (used for migraine, eg). Periactin is similar. Plaquenil is a solid anti-inflammatory (swelling). It doesn't help me much with the flushing or burning but it might be helpful if there are autoimmune issues. On my list still to try are baclofen, memantine, namenda, + retrying topical timolol. tldr I think there are lots of things to try. Look into drugs used for migraine, erythromelalgia, neuropathic pain (similar conditions imo)."
 This is another interesting post on The Rosacea Forum, by Laser_cat. She had a bad reaction to clonidine and in fact finds good results with a medication called amlodipine, which is a blood vessel dilator in fact, but at the right lower dose 'stabilizes' her blood vessels. It is called a calcium channel blocker, and all meds falling into that category are marked as potential rosacea worseners (and interesting side note; magnesium is a calcium channel blocker too, explaining why stomach acid pills I sometimes take, containing magnesium, make me so badly flushed!). I can't touch it myself, as my blood vessels become a volcano from any type of blood vessel dilator, but it is a very interesting read. Laser_cat also flushes and deteriorates from cold air and actually gets painful pale-white skin on occasions, which is not the case in my rosacea. Either I have pink or red hot skin, or my skin gets a more normal skin tone. I know about the ghostly white painful skin though, as my hands and fingers get it in winter from Raynaud's Syndrome. It is not a nice feeling and has to do with the blood vessels not constricting and dilating normal, but excessively. For that condition (Raynaud's), blood vessel dilating meds like amlodipine are actually prescribed and effective, which makes me wonder if Laser_cat might perhaps have something comparable in her facial blood vessels. Maybe, or maybe not! But cold air is something that actually makes my rosacea skin normal pale in tone, and cool and less painful, so there might be some different mechanisms at play here. Her blood vessels seem to respond violently to being constricted too much, from what I understand from her. Also important detail; Laser_cat takes a low dose of amlodipine (around 0.6 mg a day), not a normal or high dose. And she also takes other meds to help with flushing and burning; Effexor, mirtazapine, plaquenil, and 3 monthly botox sessions. She also has specific underlying other health conditions, including small fiber neuropathy and possibly (from what I understand) erythromelalgia. In her forum posts, she also details specific treatments she received: lidocaine infusions and nerve blocks. Either way, very good posts by her. When I googled amlodipine, I came across this scientific article, stating:
This is another interesting post on The Rosacea Forum, by Laser_cat. She had a bad reaction to clonidine and in fact finds good results with a medication called amlodipine, which is a blood vessel dilator in fact, but at the right lower dose 'stabilizes' her blood vessels. It is called a calcium channel blocker, and all meds falling into that category are marked as potential rosacea worseners (and interesting side note; magnesium is a calcium channel blocker too, explaining why stomach acid pills I sometimes take, containing magnesium, make me so badly flushed!). I can't touch it myself, as my blood vessels become a volcano from any type of blood vessel dilator, but it is a very interesting read. Laser_cat also flushes and deteriorates from cold air and actually gets painful pale-white skin on occasions, which is not the case in my rosacea. Either I have pink or red hot skin, or my skin gets a more normal skin tone. I know about the ghostly white painful skin though, as my hands and fingers get it in winter from Raynaud's Syndrome. It is not a nice feeling and has to do with the blood vessels not constricting and dilating normal, but excessively. For that condition (Raynaud's), blood vessel dilating meds like amlodipine are actually prescribed and effective, which makes me wonder if Laser_cat might perhaps have something comparable in her facial blood vessels. Maybe, or maybe not! But cold air is something that actually makes my rosacea skin normal pale in tone, and cool and less painful, so there might be some different mechanisms at play here. Her blood vessels seem to respond violently to being constricted too much, from what I understand from her. Also important detail; Laser_cat takes a low dose of amlodipine (around 0.6 mg a day), not a normal or high dose. And she also takes other meds to help with flushing and burning; Effexor, mirtazapine, plaquenil, and 3 monthly botox sessions. She also has specific underlying other health conditions, including small fiber neuropathy and possibly (from what I understand) erythromelalgia. In her forum posts, she also details specific treatments she received: lidocaine infusions and nerve blocks. Either way, very good posts by her. When I googled amlodipine, I came across this scientific article, stating:
A 45-year-old woman made an outpatient visit to our hypertension clinic. The woman was diagnosed with essential hypertension, and she had an average blood pressure of 150/90 mm Hg, a heart rate of 70 bpm and a body mass index of 26 kg m2. The patient was not receiving any treatment at the time. In her medical history, there was a previous diagnosis of rosacea, and blushing was observed. She was prescribed amlodipine (5 mg) and instructed to check her blood pressure three times a week for the next month. After 2 weeks, the patient returned to the clinic because of worsening skin flushing. The patient reported neither lifestyle changes nor the use of any other drugs or cosmetics. She reported that the ‘redness’ on her cheeks worsened after a few days and that, after a week, she started to notice an increased number of telangiectasias. Treatment with
amlodipine was discontinued, and the patient was prescribed ramipril (5 mg). After 2 additional weeks, skin flushing was reduced from constant to occasional, and there was a consistent decrease in the appearance of telangiectasias. This case suggests a possible association between treatment with calcium channel blockers (CCBs) and the exacerbation of rosacea.
A 45-year-old woman made an outpatient visit to our hypertension clinic. The woman was diagnosed with essential hypertension, and she had an average blood pressure of 150/90 mm Hg, a heart rate of 70 bpm and a body mass index of 26 kg m2. The patient was not receiving any treatment at the time. In her medical history, there was a previous diagnosis of rosacea, and blushing was observed. She reported irregular menses over the past year, with her last menses B2 months before the visit. She was prescribed amlodipine (5 mg) and instructed to check her blood pressure three times a week for the next month. After 2 weeks, the patient returned to the clinic because of worsening skin flushing. The patient reported neither lifestyle changes nor the use of any other drugs or cosmetics. She reported that the ‘redness’ on her cheeks worsened after a few days and that, after a week, she started to notice an increased number of telangiectasias. Treatment with amlodipine was discontinued, and the patient was prescribed ramipril (5 mg). After 2 additional weeks, skin flushing was reduced from constant to occasional, and there was a consistent decrease in the appearance of telangiectasias. This case suggests a possible association between treatment with calcium channel blockers (CCBs) and the exacerbation of rosacea. Patients who presented with flushing were referred to a dermatologist. Of the 62 patients who discontinued therapy because of flushing, 34 were diagnosed with rosacea or pre rosacea. Rosacea was diagnosed in 34 patients, 23 women and 13 men, who were between 43 and 57 years of age. These patients were diagnosed with hypertension within the
last 3 to 5 years and had not previously taken CCBs. When patients with rosacea
discontinued the use of CCBs, there was a slow but consistent reduction of symptoms.In all current clinical guidelines, CCBs belong to the class of recommended first line antihypertensive drugs for the treatment of essential hypertension. One of the main clinical side effects of CCB use is flushing, which is experienced by B5% of patients. These types of side effects, which are drug and dose-related, have a greater incidence in women than in men (4.5 versus 1.5%, respectively). Rosacea is not listed as a contraindication in the Summaries of Product Characteristics of common clinically relevant CCBs. Physicians should be aware that subclinical rosacea could be the cause of treatment discontinuation or of the lack of compliance with antihypertensive therapy. When possible, it may be useful to choose another first-line antihypertensive drug instead of CCBs.
Adverse side effects that forced the interruption of the treatment with CCBs
Side effects
Flushing 23
Peripheral edema 27
Flushing and edema 39
Tachycardia 11
 I updated more about my neurontin trial on September 12th 2006: "I have to say first that I don't take too much of this medicine: usually people take up to 1200 or 1600 mg a day as an average, and my doc prescribed me 900 mg, of which I take 600 mg daily now. One tablet in the early evening and one before sleeping. The first side-effects (dizziness, bad coordination etc) have passed luckily, pretty quickly. I do have to say that I have a bad cold, stuffed nose etc. Together with a long list of side-effects this is mentioned as happening 'often', in my medication info leaflet. But nothing too bad. I have a blood pressure measuring device, because another side-effect that happens often is supposed to be hypertension, and I take all my meds to lower it... So far my blood pressure if fairly low, the way I want it (I have check ups with my GP and dermatologist every now and then and they agree this is still OK for me): I'm around 98 over 60, still while on this medicine and the diclofenac, which raises blood pressure as well. Does it still work for my burning and flushing? I think it does. I have had a bad day, but that was due to going to the football, getting all over excited, having some chips (BAAAAD for me) and having hot weather here. But I still am more pale then usual I would say and the pain has definitely become less sharp. [..] Now I don't know if the reduction in redness and flushing (and I want to emphasis it is a noticeable REDUCTION, by no means an elimination) comes from the reduction of neural burning, which definitely plays a role in my flushing (it seems to act like a trigger). [..] Still improvement: less burning pain and less red and less easily flushed. Found some more articles about gabapentin/ neurontin for hot flushes. And also for its use for anxiety (felt better already on the mirtazapine, but this has lifted my mood considerably, compared with the better face lately of course...). [..] It's certainly not a wonder drug. Today it was hot, and after being outside for a while and eating the wrong porridge I am old fashioned flushed again, for the last couples of hours. But in general it is going a bit better. Fingers crossed. See how I'll be at the end of the week. Nat"
I updated more about my neurontin trial on September 12th 2006: "I have to say first that I don't take too much of this medicine: usually people take up to 1200 or 1600 mg a day as an average, and my doc prescribed me 900 mg, of which I take 600 mg daily now. One tablet in the early evening and one before sleeping. The first side-effects (dizziness, bad coordination etc) have passed luckily, pretty quickly. I do have to say that I have a bad cold, stuffed nose etc. Together with a long list of side-effects this is mentioned as happening 'often', in my medication info leaflet. But nothing too bad. I have a blood pressure measuring device, because another side-effect that happens often is supposed to be hypertension, and I take all my meds to lower it... So far my blood pressure if fairly low, the way I want it (I have check ups with my GP and dermatologist every now and then and they agree this is still OK for me): I'm around 98 over 60, still while on this medicine and the diclofenac, which raises blood pressure as well. Does it still work for my burning and flushing? I think it does. I have had a bad day, but that was due to going to the football, getting all over excited, having some chips (BAAAAD for me) and having hot weather here. But I still am more pale then usual I would say and the pain has definitely become less sharp. [..] Now I don't know if the reduction in redness and flushing (and I want to emphasis it is a noticeable REDUCTION, by no means an elimination) comes from the reduction of neural burning, which definitely plays a role in my flushing (it seems to act like a trigger). [..] Still improvement: less burning pain and less red and less easily flushed. Found some more articles about gabapentin/ neurontin for hot flushes. And also for its use for anxiety (felt better already on the mirtazapine, but this has lifted my mood considerably, compared with the better face lately of course...). [..] It's certainly not a wonder drug. Today it was hot, and after being outside for a while and eating the wrong porridge I am old fashioned flushed again, for the last couples of hours. But in general it is going a bit better. Fingers crossed. See how I'll be at the end of the week. Nat"I updated on September 15th 2006: "Update: am now on the neurontin for about 1,5 week, and definitely an improvement in the neuro pain (burning); don't have much problem with the right cheek anymore, the one that got irritated by an ice pack. Also am less red and less easily flushed. Still flush of course and still live with all my limitations (food-wise, no heath, a fan), but clear improvement. Didn't tell my boyfriend I'm experimenting again, but he told me several times this week I look kinda pale sometimes, and if things are going better. So he's objective, lol. Only side-effect is a bad cold and my nose is full. To be continued."
And I updated on September 19th 2006: "Just saw my derm and he was very pleased and intrigued with the latest improvements. He wants me to continue with the gabapentin, together with my other meds (YES!), I was armed with some very bad and red before pics and pale after pics and medical references for gaba and hot flushes. There were 5 docs there gathered and they were impressed luckily. They wanted to keep the pics for documentation and said I was an exceptional case for them, since I'm the only one in the hospital that has such a bad case of vascular rosacea and flushing. So far it seems the attack of my flushing from different angles seems to pay off. Low dose accutane is still another option, but I can't use it on top of all the other meds I already take probably, and besides that the derm still wants to experiment with very little skin areas for IPL and Yag lasers in 4 months time. Since my other test patches are still pale (both the IPL one and the YAG). No more full face treatments EVER for me, according to him, but IF it does help locally a very long treatment plan... with a little bit treated each time. Luckily I don't seem to have to pay for them, since this is a professional hospital and no private clinic (so covered by health insurance). The gabapentin (neurontin) definitely makes my face less painful! Especially the right cheek burned non-stop before, no matter if it was red or pale and strong anti-inflammatory medication (NSAID's) didn't help to calm any of it down. Now I only feel pain and burning when I have a real full face flush, which happens every day for maybe 30 minutes, usually around 18:00 when my body temp rises I think.. I found many links for gaba helping with menopausal hot flushes, which are in essence sort of similar to our rosacea flushings, according to my derm. So that might help, just as the fact that my face burns less and triggers less flushing by that."
And I updated on September 23rd 2006: "Bad developments: the last 4 days I'm getting big red p&p's over my cheeks. Usually I never have them. And my nose cold just doesn't resolve: have got it now almost ever since I started this drug. The p&p's worry me the most. Not sure if the gabapentin is causing it. Did taper my dose down a bit today (was 900 mg, now 600) and maybe will continue to do this and see if the skin gets better. But even on this lower dose the right cheek starts to burn and hurt and throb again. This is not the way I would have liked things to go.. To be continued."
And I updated on September 19th 2006: "Just saw my derm and he was very pleased and intrigued with the latest improvements. He wants me to continue with the gabapentin, together with my other meds (YES!), I was armed with some very bad and red before pics and pale after pics and medical references for gaba and hot flushes. There were 5 docs there gathered and they were impressed luckily. They wanted to keep the pics for documentation and said I was an exceptional case for them, since I'm the only one in the hospital that has such a bad case of vascular rosacea and flushing. So far it seems the attack of my flushing from different angles seems to pay off. Low dose accutane is still another option, but I can't use it on top of all the other meds I already take probably, and besides that the derm still wants to experiment with very little skin areas for IPL and Yag lasers in 4 months time. Since my other test patches are still pale (both the IPL one and the YAG). No more full face treatments EVER for me, according to him, but IF it does help locally a very long treatment plan... with a little bit treated each time. Luckily I don't seem to have to pay for them, since this is a professional hospital and no private clinic (so covered by health insurance). The gabapentin (neurontin) definitely makes my face less painful! Especially the right cheek burned non-stop before, no matter if it was red or pale and strong anti-inflammatory medication (NSAID's) didn't help to calm any of it down. Now I only feel pain and burning when I have a real full face flush, which happens every day for maybe 30 minutes, usually around 18:00 when my body temp rises I think.. I found many links for gaba helping with menopausal hot flushes, which are in essence sort of similar to our rosacea flushings, according to my derm. So that might help, just as the fact that my face burns less and triggers less flushing by that."
And I updated on September 23rd 2006: "Bad developments: the last 4 days I'm getting big red p&p's over my cheeks. Usually I never have them. And my nose cold just doesn't resolve: have got it now almost ever since I started this drug. The p&p's worry me the most. Not sure if the gabapentin is causing it. Did taper my dose down a bit today (was 900 mg, now 600) and maybe will continue to do this and see if the skin gets better. But even on this lower dose the right cheek starts to burn and hurt and throb again. This is not the way I would have liked things to go.. To be continued."
 I updated on October 2nd 2006: "The rash continued for a week, before I became suspicious of the glycerin that the capsule is made of. Checked with the manufacturer and it appeared to be made from glycerin, made from pork skin. And pork can make me break out. So before stopping neurontin I decided to take it without the capsule and most of the acne is gone by now. But, after 3 weeks I felt my flushing became worse again and after each dose of neurontin the flushing actually increased for a while. I found out that vasodilatation and hypertension are mentioned as apparently “frequent” side effects of this drug, although this varies at different sites and others say it is only happens in 1% in controlled trials. My blood pressure raised from 90 over 68 to 120 over 80 and back though (I have a little measuring device). That is not good. And I've become very suspicious about the vasodilatation. Since I tapered off the gabapentin this week, the pain in my cheek is back but hopefully I can convince my derm. to try another medicine. He will call me tomorrow. I’ll ask him for another painkiller: I checked the internet again, and looked for neuropathic pain. There is a special condition, when one side of the face has neuropathic pain, atypical facial neuralgia or something. Anyway: I checked all the medication that is mentioned for its treatment. Amitriptyline is an antidepressant that helps often for burning pain, but I used it a little while 3 years back and it made me flush very badly, so no more. The pharmacist later explained to me that it opens up the little blood vessels in the face, so that it was on the cards. There are other drugs, like SSRI’s (Paroxetine, Citalopram Effexor). To me carbamazepine (Tegretol) seems my best next shot. I checked it’s side-effects and they are usually mild and nothing to do with hypertension, vasodilatation, flushing etc. Rash is mentioned unfortunately, but that’s the case with ALL anticonvulsants, and those are the drugs that can help blocking the pain sensations coming from the brain. I guess eventually there needs to be focus on why exactly my right cheek hurts and burns, even when it looks not very red. I will ask my derm this on the phone as well tomorrow."
I updated on October 2nd 2006: "The rash continued for a week, before I became suspicious of the glycerin that the capsule is made of. Checked with the manufacturer and it appeared to be made from glycerin, made from pork skin. And pork can make me break out. So before stopping neurontin I decided to take it without the capsule and most of the acne is gone by now. But, after 3 weeks I felt my flushing became worse again and after each dose of neurontin the flushing actually increased for a while. I found out that vasodilatation and hypertension are mentioned as apparently “frequent” side effects of this drug, although this varies at different sites and others say it is only happens in 1% in controlled trials. My blood pressure raised from 90 over 68 to 120 over 80 and back though (I have a little measuring device). That is not good. And I've become very suspicious about the vasodilatation. Since I tapered off the gabapentin this week, the pain in my cheek is back but hopefully I can convince my derm. to try another medicine. He will call me tomorrow. I’ll ask him for another painkiller: I checked the internet again, and looked for neuropathic pain. There is a special condition, when one side of the face has neuropathic pain, atypical facial neuralgia or something. Anyway: I checked all the medication that is mentioned for its treatment. Amitriptyline is an antidepressant that helps often for burning pain, but I used it a little while 3 years back and it made me flush very badly, so no more. The pharmacist later explained to me that it opens up the little blood vessels in the face, so that it was on the cards. There are other drugs, like SSRI’s (Paroxetine, Citalopram Effexor). To me carbamazepine (Tegretol) seems my best next shot. I checked it’s side-effects and they are usually mild and nothing to do with hypertension, vasodilatation, flushing etc. Rash is mentioned unfortunately, but that’s the case with ALL anticonvulsants, and those are the drugs that can help blocking the pain sensations coming from the brain. I guess eventually there needs to be focus on why exactly my right cheek hurts and burns, even when it looks not very red. I will ask my derm this on the phone as well tomorrow."I updated on October 4th 2006: "I made a mistake: I said glycerin but the capsule is made of GELATINE."
I last updated on April 12th 2011: "I used gabapentin for some time, after I was so silly to fall asleep on a cool pack, that was too frozen still. So I had nerve pain for 6 months :S The neurologist I saw prescribed it to me, after Lyrica made me flush. At first, the gabapentin made me more pale. I was over the moon. But after a week or so, can't remember exactly how long it was, it seemed to make me more flushed. I looked it up and found that it can act as a vasodilatator. So I stopped with it. It did help a bit with the neuro pain though. And luckily that resolved after 6 months by itself. But I understand you have it constantly, and not from some injury to the skin like I had? I would just try it and see how it works for you. You can always stop again with it if you find that it aggravated your skin.. best wishes Nat"
 You can read this article;
You can read this article; UNDERSTANDING NEUROPATHIC PAIN
"Neuropathic pain, in contrast to nociceptive pain, is described as "burning", "electric", "tingling", and "shooting" in nature. It can be continuous or paroxysmal in presentation. Whereas nociceptive pain is caused by the stimulation of peripheral of A-delta and C-polymodal pain receptors, by algogenic substances (eg. histamine bradykinin, substance P, etc.) neuropathic pain is produced by damage to, or pathological changes in the peripheral or central nervous systems. The hallmarks of neuropathic pain are chronic allodynia and hyperalgesia. Allodynia is defined as pain resulting from a stimulus that ordinarily does not elicit a painful response (eg. light touch). Hyperalgesia is defined as an increased sensitivity to a normally painful stimuli. Primary hyperalgesia, caused by sensitization of C-fibers, occurs immediately within the area of the injury. Secondary hyperalgesia, caused by sensitization of dorsal horn neurons, occurs in the undamaged area surrounding the injury.
On the best treatment options
As previously mentioned, most neuropathic pain responds poorly to NSAIDS and opioid analgesics. The mainstay of treatment are predominantly the tricyclic antidepressants (TCA's), the anticonvulsants and the systemic local anesthetics. Other pharmacological agents that have proven efficacious include the corticosteroids, topical therapy with substance P depletors, autonomic drugs and NMDA receptor antagonists.
Tricyclic antidepressants (TCA's)
The TCA's have been successfully used for the treatment of neuropathic pain for some 25 years. The mechanism of action for the alleviation of neuropathic pain is thought to be due to the inhibition of re-uptake of serotonin and norepinephrine within the dorsal horn, however, other possible mechanisms of action include alpha-adrenergic blockade, sodium channel effects and NMDA receptor antagonism. Amitriptyline is the prototypical tertiary amine. Other tertiary amines include imipramine, doxepin, clomipramine and trimipramine. Unlike the dosing regimen utilized for the treatment of depression doses of TCA's for treatment of neuropathic pain are considerably less. The typical dosing schedule for amitriptyline may be simply 10 mg orally at bedtime with a gradual escalation every three days, in 10 mg increments, to a maximum to 30 to 50 mg orally at bedtime. Furthermore, the onset analgesia usually occurs over several days versus the two weeks that are required for the onset of the antidepressant effects of the drugs. The side effect profile of the TCA's include sedation and anticholinergic effects. Since these side effects are more prominent with the tertiary amines prudence would dictate the use of a secondary amine such as nortriptyline or desipramine, particularly in the elderly population who are more sensitive to the side effects.
SSRI antidepressants
The recently introduced selective serotonin reuptake inhibitors (SSRI's) have not proven to be as effective against neuropathic pain as anticipated. Fluoxetine (Prozac) only appears to relieve pain in patients with co-morbid depression. Paroxetine (Paxil) has found some utility in the treatment of chronic, daily headaches. In general, the SSRI's are partially effective in the treatment of diabetic neuropathy, but not to the extent of the TCA's. Venlafaxine (Effexor) may have some analgesic effects since, like the TCA's, it inhibits the reuptake of both serotonin and norepinephrine. Its side effect profile is similar to the other SSRI's and can include agitation, insomnia, or somnolence, gastrointestinal distress and inhibition of sexual functioning. Anticholinergic side effects are less bothersome than with the TCA's.
Anti-convulsants
The anticonvulsant medications can be particularly effective treatment for neuropathic pain that is described as burning and lancinating in nature. Commonly used medications in this category include phenytoin, carbamazepine, valproic acid, clonazepam and gabapentin. The mechanism of action of the anticonvulsant medications is thought to involve membrane stabilization. Evidence also suggests that some of the agents, such as carbamazepine and phenytoin can depress both segmental and descending excitatory pathways in the CNS and at the same time facilitate inhibitory mechanisms. For example, carbamazepine has been shown to inhibit the electrical C and A fiber evoked neuronal responses of spinal nerve ligated rats. Valproic acid, on the other hand, has been reported to increase gamma-amino butyric acid (GABA) levels in the substantia nigra and corpus striatum. Gabapentin, which we will be discussing subsequently, reportedly increases extracellular GABA levels throughout the brain, including the thalamus and causes the release of GABA from glial cells. However it is unlikely that Gabapentin increases GABAergic tone because neither GABAa nor GABAb antagonists reverse the analgesic effects of Gabapentin. Because of the significant risks of the blood dyscrasias and liver dysfunction, baseline and periodic monitoring of blood chemistries and liver function tests are highly recommended when prescribing phenytoin, carbamazepine, or valproic acid. Although clonazepam, a benzodiazepine, is usually used for the treatment of petite mal and myoclonic seizures, it has been successfully utilized to treat the lancinating and pain associated with phantom limb pain. Its mechanism of action may be associated with its reputed ability to enhance the inhibitory action of GABA within the CNS, and also possibly secondary to increased serotonin levels.
"Neuropathic pain, in contrast to nociceptive pain, is described as "burning", "electric", "tingling", and "shooting" in nature. It can be continuous or paroxysmal in presentation. Whereas nociceptive pain is caused by the stimulation of peripheral of A-delta and C-polymodal pain receptors, by algogenic substances (eg. histamine bradykinin, substance P, etc.) neuropathic pain is produced by damage to, or pathological changes in the peripheral or central nervous systems. The hallmarks of neuropathic pain are chronic allodynia and hyperalgesia. Allodynia is defined as pain resulting from a stimulus that ordinarily does not elicit a painful response (eg. light touch). Hyperalgesia is defined as an increased sensitivity to a normally painful stimuli. Primary hyperalgesia, caused by sensitization of C-fibers, occurs immediately within the area of the injury. Secondary hyperalgesia, caused by sensitization of dorsal horn neurons, occurs in the undamaged area surrounding the injury.
On the best treatment options
As previously mentioned, most neuropathic pain responds poorly to NSAIDS and opioid analgesics. The mainstay of treatment are predominantly the tricyclic antidepressants (TCA's), the anticonvulsants and the systemic local anesthetics. Other pharmacological agents that have proven efficacious include the corticosteroids, topical therapy with substance P depletors, autonomic drugs and NMDA receptor antagonists.
Tricyclic antidepressants (TCA's)
The TCA's have been successfully used for the treatment of neuropathic pain for some 25 years. The mechanism of action for the alleviation of neuropathic pain is thought to be due to the inhibition of re-uptake of serotonin and norepinephrine within the dorsal horn, however, other possible mechanisms of action include alpha-adrenergic blockade, sodium channel effects and NMDA receptor antagonism. Amitriptyline is the prototypical tertiary amine. Other tertiary amines include imipramine, doxepin, clomipramine and trimipramine. Unlike the dosing regimen utilized for the treatment of depression doses of TCA's for treatment of neuropathic pain are considerably less. The typical dosing schedule for amitriptyline may be simply 10 mg orally at bedtime with a gradual escalation every three days, in 10 mg increments, to a maximum to 30 to 50 mg orally at bedtime. Furthermore, the onset analgesia usually occurs over several days versus the two weeks that are required for the onset of the antidepressant effects of the drugs. The side effect profile of the TCA's include sedation and anticholinergic effects. Since these side effects are more prominent with the tertiary amines prudence would dictate the use of a secondary amine such as nortriptyline or desipramine, particularly in the elderly population who are more sensitive to the side effects.
SSRI antidepressants
The recently introduced selective serotonin reuptake inhibitors (SSRI's) have not proven to be as effective against neuropathic pain as anticipated. Fluoxetine (Prozac) only appears to relieve pain in patients with co-morbid depression. Paroxetine (Paxil) has found some utility in the treatment of chronic, daily headaches. In general, the SSRI's are partially effective in the treatment of diabetic neuropathy, but not to the extent of the TCA's. Venlafaxine (Effexor) may have some analgesic effects since, like the TCA's, it inhibits the reuptake of both serotonin and norepinephrine. Its side effect profile is similar to the other SSRI's and can include agitation, insomnia, or somnolence, gastrointestinal distress and inhibition of sexual functioning. Anticholinergic side effects are less bothersome than with the TCA's.
Anti-convulsants
The anticonvulsant medications can be particularly effective treatment for neuropathic pain that is described as burning and lancinating in nature. Commonly used medications in this category include phenytoin, carbamazepine, valproic acid, clonazepam and gabapentin. The mechanism of action of the anticonvulsant medications is thought to involve membrane stabilization. Evidence also suggests that some of the agents, such as carbamazepine and phenytoin can depress both segmental and descending excitatory pathways in the CNS and at the same time facilitate inhibitory mechanisms. For example, carbamazepine has been shown to inhibit the electrical C and A fiber evoked neuronal responses of spinal nerve ligated rats. Valproic acid, on the other hand, has been reported to increase gamma-amino butyric acid (GABA) levels in the substantia nigra and corpus striatum. Gabapentin, which we will be discussing subsequently, reportedly increases extracellular GABA levels throughout the brain, including the thalamus and causes the release of GABA from glial cells. However it is unlikely that Gabapentin increases GABAergic tone because neither GABAa nor GABAb antagonists reverse the analgesic effects of Gabapentin. Because of the significant risks of the blood dyscrasias and liver dysfunction, baseline and periodic monitoring of blood chemistries and liver function tests are highly recommended when prescribing phenytoin, carbamazepine, or valproic acid. Although clonazepam, a benzodiazepine, is usually used for the treatment of petite mal and myoclonic seizures, it has been successfully utilized to treat the lancinating and pain associated with phantom limb pain. Its mechanism of action may be associated with its reputed ability to enhance the inhibitory action of GABA within the CNS, and also possibly secondary to increased serotonin levels.
 Carbamazepine has proven to be particularly effective against glossopharyngeal neuralgia, post herpetic neuralgia, trigeminal neuralgia, and diabetic neuropathies. Should carbamazepine prove ineffective, it can be replaced with phenytoin. Unlike the other anticonvulsants, valproic acid has found some success in treating migraine headaches. The combination of an anticonvulsant with a TCA can be synergistic.
Carbamazepine has proven to be particularly effective against glossopharyngeal neuralgia, post herpetic neuralgia, trigeminal neuralgia, and diabetic neuropathies. Should carbamazepine prove ineffective, it can be replaced with phenytoin. Unlike the other anticonvulsants, valproic acid has found some success in treating migraine headaches. The combination of an anticonvulsant with a TCA can be synergistic.Gabapentin (Neurontin)
1-(aminomethyl) cyclohexane-acetic acid, is an anti-epileptic drug which was introduced in 1993 and was originally approved for the treatment of partial seizures with or without secondary generalization. Recently, however, reports have documented its efficacy in the treatment of various neuropathic pain states such as complex regional pain syndrome, deafferentation neuropathy of the face, postherpetic neuralgia, sciatic type pain, and HIV-related neuropathy. The effective dose range is 30-300 mg/kg (systemic) and >37.5 mg/kg (IT). Gabapentin is reportedly completely ineffective in altering threshold responses to acute nociceptive stimuli at doses up to 300 mg/kg.53-56 Presently the mechanism of action as either an anticonvulsant or an analgesic is unknown. The antinociceptive effects are likely to be due to actions within the spinal cord, because 1000 times the IT dose is required to produce equianalgesic effects when given intraperitoneally. Gabapentin binds to the alpha 2 delta calcium channel subunit. However, the relationship between binding at this site and the analgesic properties of gabapentin have not been determined. The NMDA receptor complex may be a potential spinal locus for neuropathic pain relief , but it has not been conclusively found that this is the major site of action. Gabapentin has a relatively benign side effect profile and is well tolerated if dosing proceeds in a gradually escalating manner. It has few if any drug interactions and is primarily renally excreted. Although expensive, it does not require the routine monitoring of blood chemistries and liver functions tests like carbamazepine and phenytoin. To date, little evidence suggests the efficacy of felbamate or lamotrigine in the treatment of neuropathic pain. Further investigation is necessary. Autonomic drugs which are proven beneficial in the treatment of neuropathic pain include the alpha-2 agonists (eg. Clonidine) and alpha-1 antagonists (eg. prazosin, terazosin).
I recently read an interesting medical article, in which the author described a patient who had come to hospital with severe facial flushing and burning of the face and ears. Read more about the distinction between rosacea and EM in this blog post of mine.
"Erythema associated with pain and warmth on face and ears: a variant of erythermalgia or red ear syndrome?"
The article describes how Erythermalgia (another term for erythromelalgia) is a rare disorder of the skin, that is characterized by attacking of skin redness, pain and increased skin temperature. It mainly happens to the skin of the extremities, which means the hands, the feet and the face. It also can extend to the neck, face, ears and even the scrotum. The article describes the case of an 18-year-old woman who had a 3 years history of redness, pain and warmth of the skin of her face and ears only. Over time, the attacks (of flushing and heat and pain) became more regular and severe for her. She had these red hot flushing episodes on average several times a month, lasting from two to more than ten hours each time, and sometimes the attacks lasted days even. She noticed that the episodes always started on her cheeks and then radiated quickly to her ears and forehead. She did not get scales on her skin and she neither sweated or got a headache during these attacks. The most painful areas were the cheeks. The symptoms disappeared completely between episodes, and left no skin damage. When doctors examined her skin, they noticed skin redness (see picture from the patient on the left). They also noticed that her skin had an increased temperature during a flare and that her face and ear skin was tender. When she cooled her skin, the flare went down again. When doctors used a dermatoscope to look more closely at her skin, it showed that blood vessels inside the patches of skin redness were more dilated during the flare, and that they constricted again when the skin had been cooled with ice. She also noticed that warmth and movement could trigger the attacks or worsen the symptoms while cleaning her teeth, eating, drinking, brushing her hair, touching or rubbing the ears. She preferred to stay in a cold environment during the flares. She also had flushing and pain attacks when she was laying down, at night. This really affected her quality of sleep. In the past, the patient had been diagnosed with seborrheic dermatitis and was treated with oral antihistamines, topical steroids and tacrolimus, and cool facial masque. The symptoms had poor response to these therapeutics, except for the cooling face masque. Because of intolerable pain, she had to spray cold water or use a cold masque on her face all day long. She never got red hands or feet and had no history of migraine, episodic headaches or neck injury.
 The researchers first considered the girl to have other health conditions that could cause the facial flushing and heat and redness, including
The researchers first considered the girl to have other health conditions that could cause the facial flushing and heat and redness, including seborrheic dermatitis (not the case as her skin showed no scales and flakes), relapsing polychondritis (inflammation of the nose and ear cartilage and other connective tissues in many organs, causing them to become inflamed and tender), chondrodermatitis nodularis chronica helicis, (another inflammatory condition affecting the ears). They ruled out contact dermatitis as well as photosensitivity, because the redness also calmed down again spontaneously, which is not usually seen with contact dermatitis and photosensitivity unless it is treated. The researchers especially suspected facial flushing to be a factor in this girls symptoms. But they stated that facial flushing is usually a symptom of an underlying medical condition or reaction to certain substance, like alcohol, drugs, allergy, emotions, exercise, food additives, skin disorders, etc. "Patients with facial flushing experience a suddenly facial reddening, feel hot face, and always associate with other symptoms relating with the nosogenesis. The reddening may extend to the neck and upper chest, even the whole body, but the patients lack cutaneous pain. Harlequin syndrome is a benign condition showing a sudden onset of unilateral facial flushing and sweating, the present case lacked sweating and showed symmetrically facial redness associated with pain and warmth, Harlequin syndrome can also be excluded."
The doctors came finally to the conclusion that this patient had a rare form of erythermalgia (erythromelalgia). They also considered the option of Red Ear Syndrome (RES). Normally patients with this condition also suffer from red hot feet and hands. Not just a red hot face and ears. But in this case, doctors diagnosed her with a special form of erythromelalgia, that only affected her face and ears. They found out that the symptoms went down a bit (but not fully) after the patient was given oral antihistamine medication. The same happened when they applied topical steroid cream on her skin (be veeeery careful with this as a rosacea patient!! Steroid creams can worsen rosacea or even cause it in sensitive people with a predisposition for blushing and burning). Doctors also found that her skin improved mildly from a cream called Protopic (tacrolimus). However, what really helped control all these patients symptoms, was a combination treatment of aspirin and paroxetin; an SSRI type of antidepressant, also known under the names Paxil and Seroxat. Her face flushing and redness also improved markedly after having been treated with oral gabapentin (a nerve pain medication), and indomethacin (a non-steroid anti inflammatory drug), and topical lidocaine compounds (a local anesthetic (numbing medication) and cold masque for 3 days; but 2 weeks after she stopped using these three medications her symptoms returned. She was then treated with the aspirin 0.1, twice a day; paroxetine 10 mg daily, which resulted in complete disappearance of her symptoms after having been treated for 2 weeks. Without any treatment, the patient remained symptom free for 6 months and was still under follow-up. There are many treatment options for EM, but none work for everyone and they all have varying response success. No treatment is consistently effective, and to predict the efficacy for a specific treatment is also impossible.
 Lumbar sympathetic block was reported in a case showing successful response in a refractory EM recently. I will write another blog post soon about these sympathetic blocks for vascular rosacea. Most times, EM starts later in life, often in women's 50's or 60's. But interestingly enough, the case described, and another case referred to in the research above, mentions the onset of EM of only the face to be very young: 14 years of age and in the case of the girl described above 15 years of age. There has also been a case described by Ramirez and Kirsner of a man who's symptoms of ear burning started at the age of 50. The reasons for the younger age onset for EM of the face remains unknown, but because there are not that many cases of it known, it could also be a coincidence, the researchers wrote. They also think that dilation of the blood vessels in the skin is at least partially responsible for the symptoms this girl had. But unfortunately for us, they conclude that the exact mechanisms are not fully understood.
Lumbar sympathetic block was reported in a case showing successful response in a refractory EM recently. I will write another blog post soon about these sympathetic blocks for vascular rosacea. Most times, EM starts later in life, often in women's 50's or 60's. But interestingly enough, the case described, and another case referred to in the research above, mentions the onset of EM of only the face to be very young: 14 years of age and in the case of the girl described above 15 years of age. There has also been a case described by Ramirez and Kirsner of a man who's symptoms of ear burning started at the age of 50. The reasons for the younger age onset for EM of the face remains unknown, but because there are not that many cases of it known, it could also be a coincidence, the researchers wrote. They also think that dilation of the blood vessels in the skin is at least partially responsible for the symptoms this girl had. But unfortunately for us, they conclude that the exact mechanisms are not fully understood.Erythromelalgia, or EM was first described in 1878 and is a rare skin disorder, characterized by redness, increased temperature and pain of the skin of the hands, feet and only sometimes the face (it rarely also affects the neck, ears, nose and scrotum). These attacks happen on irregular intervals. Its symptoms may be triggered by warmth or moderate exercise, and can be prevented or relieved by cooling. Very much like neurogenic, subtype 1 rosacea thus. It is only very rarely that this condition only manifests itself on the face (and not also on the hands and feet). It could be that people like myself, with facial flushing, burning and redness, have been misdiagnosed with rosacea when we in fact could have this rare form of erythromelalgia. Although it is normal for erythromelalgia to ALSO give red, hot and flushed hands and feet, together with a possible flushed face. I have Raynaud's syndrome on my hands, so they can go white or red and swollen in the cold or heat, but it is nothing like EM redness and pain, for me personally.. Or, it could be that our type of rosacea has some similarities with erythromelalgia's flushing of the skin, and that by further understanding erythromelalgia, we might perhaps also be able to learn a bit more about this still poorly understood problem of facial flushing and burning that can come with rosacea.
Erythromelalgia flushing of the face compared with my own rosacea flushing of the face:
 In the article above, the researchers write that there have been more (rare) cases described in the medical literature of patients with erythromelalgia flushing of only the face and ears, and without the characteristic flushing and burning of hands and feet and legs.
In the article above, the researchers write that there have been more (rare) cases described in the medical literature of patients with erythromelalgia flushing of only the face and ears, and without the characteristic flushing and burning of hands and feet and legs.
"EM includes primary and secondary forms. It is considered that the mutations in SCN9A, encoding the sodium channel protein Na(v)1.7 subunit, are responsible for the primary type, while neuropathological and microvascular functional changes may be for the secondary one."
 Red Ear Syndrome (RES) has some similar clinical features as EM. It always occurs in one, or less frequently in both ears. Sometimes the redness and flushing also radiates to the back of the neck, the forehead or even the jaw. Its attacks may be spontaneous, or triggered by touch, exertion, heat or cold stimuli, neck movements, stress, cleaning the ear, etc. RES also includes 2 subtypes: the primary and secondary. The primary form seems to start spontaneously and doctors have not found a cause for it yet. It commonly occurs in young people and is associated with migraine, while the secondary form happens more often to adults, and is linked to problems, injuries or pain of the neck disks. cervical disorders and pain or injuries of the jaw joint.
Red Ear Syndrome (RES) has some similar clinical features as EM. It always occurs in one, or less frequently in both ears. Sometimes the redness and flushing also radiates to the back of the neck, the forehead or even the jaw. Its attacks may be spontaneous, or triggered by touch, exertion, heat or cold stimuli, neck movements, stress, cleaning the ear, etc. RES also includes 2 subtypes: the primary and secondary. The primary form seems to start spontaneously and doctors have not found a cause for it yet. It commonly occurs in young people and is associated with migraine, while the secondary form happens more often to adults, and is linked to problems, injuries or pain of the neck disks. cervical disorders and pain or injuries of the jaw joint.
So erythromelalgia can look a lot like neurogenic (subtype 1) rosacea. Especially as in rare cases, erythromelalgia only manifests itself as redness and flushing and burning of the face (so not on the hands and feet as well). The case of the young woman described above showed the exact same symptoms as I have during a flare with (as it stands for now) the diagnosis rosacea.
And some people with rosacea turn out to have erythromelalgia as well, for instance in the case of AEB:
AEB wrote on May 27th, 2016: "I started with facial flushing, which then spread to my ears, and a few months later chest and arms--brought on by stress but most of all heat. My diagnosis is rosacea and erythromelalgia because of the intensity of redness and burning and the times/ways it presents. So you may want to ask your doctor about that too and maybe do some research of your own (since it's rare and many drs haven't heard of it, I've found). The testing can be exhausting but gives you more treatment options and the relief of knowing what you're dealing with!"
Rosacea Forum post: Neurogenic rosacea; my battle
Rosacea Forum post: Whats all this phantom burning about eh Neurogenic Rosacea AKA Burning but no flush
Rosacea Forum post: 'Neurogenic rosacea -- my battle.
Rosacea Forum post: Neuropathic rosacea
Rosacea Forum post: Gabapentin and Pregabalin
Rosacea Forum post: Anyone Tried Gabapentin
Rosacea Forum post: Painful burning possible hormone connection
Rosacea Forum post: Type 1 rosacea KPRF flushing and considering ETS
Rosacea Forum post: Neurogenic rosacea turned out to be Lyme disease
Rosacea Forum post: Facial burning w little to no redness
Rosacea Forum post: Anyone any experiences with Lyrica
Rosacea Forum post: Worsening of painful facial redness
Rosacea Forum post: Please please help Burning sooo bad!
Rosacea Forum post: Anyone have Neurogenic Rosacea (nose swelling)
Rosacea Forum post: Could this be Rosacea Burning face never flushing
Rosacea Forum post: Anyone Tried Gabapentin
Pubmed research: Neuropathic Pain - A Maladaptive Response of the Nervous System to Damage
David Pascoe, 'How Do You Treat Neurogenic Rosacea?'
David Pascoe, 'Neuropeptide PACAP Modulators for Neurogenic Rosacea'
Laser_cat: 'Neurogenic rosacea -- my battle.
Pubmed research: Mechanisms of neuropathic pain
"Just wondering if anyone else has experience with face and neck flushes? I seem to now also be getting very red cheeks, face and neck. Comes and goes. Also red ears. (This is on top of the usual feet/hands burning). If you do, is there anything you used that helped cleared it up? [..] Like tonight for example - very cold night. Feet are fine but cheeks are burning... Thanks in advance, Craig"
Mads replied in October 2013: "Hi Ocker, Yes, I get flushes or flaring of face, neck, ears and scalp. My EM started in my right knee, then feet etc.working its way up my body rather like a fungus spreading.. I had very acute onset (2-3 months), which has now remained completely widespread and chronic(8 months now). I'm struggling. Really struggling! Most research states EM is progressive. To help minimize - very difficult and very much trial/error. Depends what you respond to - all of us need an individualized poly-pharmacy approach. I responded moderately to lidocaine so 'theoretically' my EM is linked to sodium channel blockers or analogs of such like mexiletine. Other folk respond to serotonin antagonists. I have listed things that i have tried with/without luck in my profile section. This is an awful thing isn't it. Do you know what type of EM you might have? Mine is primary, idiopathic, God bless. Please pm me if you wish to offload/chat about symptoms etc. Hoping you have a 'comfortable' night as possible. Mads"
Mads replied in October 2013: "Hi Ocker, Yes, I get flushes or flaring of face, neck, ears and scalp. My EM started in my right knee, then feet etc.working its way up my body rather like a fungus spreading.. I had very acute onset (2-3 months), which has now remained completely widespread and chronic(8 months now). I'm struggling. Really struggling! Most research states EM is progressive. To help minimize - very difficult and very much trial/error. Depends what you respond to - all of us need an individualized poly-pharmacy approach. I responded moderately to lidocaine so 'theoretically' my EM is linked to sodium channel blockers or analogs of such like mexiletine. Other folk respond to serotonin antagonists. I have listed things that i have tried with/without luck in my profile section. This is an awful thing isn't it. Do you know what type of EM you might have? Mine is primary, idiopathic, God bless. Please pm me if you wish to offload/chat about symptoms etc. Hoping you have a 'comfortable' night as possible. Mads"
Clarissajo replied in October 2013: "Ocker, I too have this occur frequently.... EM can hit me in the face, ears, and chest as well as arms, hands, feet, legs. Unfortunately I don't know anything about pharmaceuticals for EM, my doctors have only suggested aspirin, which I cannot take for other reasons. I'm interested in learning more about possible meds for this condition. I do keep feet elevated and try to stay as cool as possible. [..] I currently take Lyrica (pregabalin) which has similar effects. I didn't realize that it was so similar to gabapentin until very recently.... apparently a lot of people take either gabapentin OR lyrica, and usually choose gabapentin because it's less expensive. My neurologist is prescribing the Lyrica plus Cymbalta because that combo is very effective against my fibromyalgia pain, and also she says the Lyrica helps prevent seizures which I have a tendency to have. Thanks again!Take care, JoAnn"
Gaga replied in October 2013: "Mine started with my face and ears. I had that for about 2 years. I was sure I must have Lupus due to other symptoms but doctors just said I had red face syndrome and red ear syndrome. The ears are so touchy sore that just my hair touching the tops of my ears feels like my ears are raw skin. When my cheeks get real bright which is every day, several times and sometimes constantly for days, I look like a clown. I get so explosively hot and my head sweats too. My feet started about 2 years ago. My feet also go numb due to Spinal Stenosis but they are sore. My big toes and the foot just behind the big toe hurt so bad and are so sore. The soles of my feet are deep red even when the hot feeling eases off. The only help I've had with my feet is to rub with a menthol liniment to give a false cool feeling and then turn a fan on them. Wetting my head with cool water sometimes eases the warmth of my face but not my ears. Today it felt like the heat was attacking my spine. This is just awful."
LibbyK replied in October 2013: "I've been having persistent redness and occasional episodes of heat in my face - mostly nose and upper cheeks. We thought it could be lupus but my ANA test was fine. I suspect it may be rosacea with an EM flare here and there. I've been using only products for sensitive skin (helps a little as I do have dry, sensitive skin) and wearing makeup to cover the red when I go out. I haven't tried any drugs."
 \Mary replied in October 2013: "I’ve had neck and facial flushing for over three years now. There seems to be no way that I know of to get rid of the flushing. It does come and go. What I do take daily to help for the pain is Gabapentin…it works great for me!!! Now when I was in my 30’s and I got Rosacia I used Metrogel that I got from my Dermatologist and I still use it and that helps a tiny bit for burning along with medication."
\Mary replied in October 2013: "I’ve had neck and facial flushing for over three years now. There seems to be no way that I know of to get rid of the flushing. It does come and go. What I do take daily to help for the pain is Gabapentin…it works great for me!!! Now when I was in my 30’s and I got Rosacia I used Metrogel that I got from my Dermatologist and I still use it and that helps a tiny bit for burning along with medication."Flaming replied in August 2015: "I have burning in my neck and face. Started about eight months ago. It is very bad at night. I keep a cooler beside my bed and use a gel lack wrapped in a dish towel to cool my face. I tried aspirin when I was first diagnosed and it helped a bit when it I took it at 4 am when the pain was at its worse. I could only tolerate (does was super high: 1200 mg’s) for five night before my stomach pain put a stop to that. I have secondary EM and my doctor hopes that this short trial with aspirin shows that I could benefit from lidocaine infusion. I hope to get that in the Fall. It was my pain doctor who diagnosed me. I think rosacea and EM are very different, so shouldn’t be hard to differentiate for a medical doc. My pain doc isn’t an Em expert, but she could diagnose it. My GP thought it was hot flashes from menopause. Even I knew that was not the case. Hot flashes (and rosacea) do not hurt!!! {Scarlet Nat: Incorrect; neuropathic rosacea does hurt}. I see a neurologist today who is supposedly the only person in town (Vancouver) who knows anything about EM. Here’s hoping she can help. First, I have to get the dang EMG testing over with prior to the consult today. If I have anything helpful for to report, I will post, for sure. Take care, all."
 Anaesthetic injection could ease hot flushes and flushing
Anaesthetic injection could ease hot flushes and flushingInjecting a local anaesthetic into the neck is associated with a 50% reduction in hot flushes among women with moderate to severe symptoms. They can also help curb facial flushing.
What are hot flushes?
Hot flushes are sudden feelings of heat or warmth starting in the face and extending to the neck and chest area, sometimes accompanied by sweating and flushing of the skin. They are associated with menopause, but can also occur in patients taking oestrogen-blocking medications, typically for breast or prostate cancer. Walega estimated that hot flushes affect more than 80% of menopausal women. To deliver the treatment, the physician uses guided imaging to inject a local anaesthetic into what is called the stellate ganglion, an area between the thyroid gland (around the "voice box") and the carotid artery. "The patient feels a sense of intense pressure from the physician's finger [guiding the needle], and the pain is moderate," said Walega. "In 30 seconds, we're done." The researchers got the idea of attacking extreme hot flushes by treating the stellate ganglion from unintended consequences of a pain study published in The Lancet in 2007. "Patients reported their pain was still there, but their hot flushes were gone," Walaga said.
Anaesthetic injection
For this study, scheduled for presentation at the American Society of Anaesthesiologists' annual meeting in San Francisco, the researchers recruited 40 women between 35 and 65 years old. All were either in natural or surgically (when the ovaries are removed) induced menopause. Half of the women received a stellate ganglion blockade injection of bupivacaine hydrochloride, a local anaesthetic. The others were given a placebo, an injection of sterile saline. Participants kept track of their hot flushes for two weeks preceding the injection and six months afterward. The researchers found that stellate ganglion blockade reduces the incidence of hot flushes by half, especially in women with moderate or severe hot flushes, and the benefits appear to last for at least six months. Subjects also reported experiencing less depression after getting the bupivacaine injections, and they demonstrated improved verbal recall of spoken words. Walega said the treatment is safe when done by specially trained physicians using X-ray fluoroscopy to guide the injection. The stellate ganglion sits near the carotid artery, the vertebral artery and the spinal cord. "Injecting any of those arteries with anaesthetic could cause a seizure and loss of consciousness, and it could do damage to the spinal cord," he explained. As for the risk of radiation exposure from the fluoroscopy, it is equivalent to that of a chest X-ray, he added.
Resetting the thermostat
Why might these injections work? Walega said he thinks the ganglion may play a role in turning certain nerves on or off. "It's complex and there's so much else we don't know," Walega said. "We might be resetting the thermostat." Walega now plans to do a larger study with more than 200 participants, he noted. Dr Grace Forde, an attending physician and pain management specialist at Syosset Hospital in New York, noted that a large percentage of the patients receiving the placebo also reported an improvement in their hot flushes. "Invasive procedures often have a much stronger placebo effect," she noted. Walega estimated that the treatment, if proven effective in a larger study, would cost between $750 and $1000. Forde, who was not associated with the study, said she thinks the benefits of the treatment probably outweigh the risks. "You can't put a price on quality of life. I personally think it's worth it." Because this study was presented at a medical meeting, the data and conclusions should be viewed as preliminary until published in a peer-reviewed journal.
More information
 Palmitoylethanolamide (PEA)
Palmitoylethanolamide (PEA)I was also tipped on the supplement palmitoylethanolamide (PEA) for the treatment of pain, inflammation and even of mast cell instability. I ordered it this week and will give it a try as soon as it comes in. So far I have had bad reports with mostly all supplements however. Only Alpha Lipoic Acid seemed to help slightly, the rest either did nothing (a few) or made my flushing worse (most). But will try it anyway. So what is palmitoylethanolamide (PEA)? It is a fatty acid, produced in the body to combat pain and inflammation, by boosting your natural cannabinoids and protecting the nerves throughout your body. My rosacea is both vascular and neuropathic, meaning it shows itself through constant dilating of the blood vessels - flushing, redness - as well as giving me a lot of nerve pain in the face; my skin always feels tight, burned up and uncomfortable. And when I get massively flushed or more red than usual, it feels on fire, literally like someone threw something hot or acid-like on it. So the nerves in my facial skin have become hypersensitive after twenty years of rosacea flushing, inflammation and swelling. hence, this supplement sounds good so far :) What else? Palmitoylethanolamide (PEA) can also be found in soy lecithin, soybeans, egg yolk, peanuts, and alfalfa. However, most of these might not be a suitable option for people with food sensitivities (soy can be a trigger for rosacea as well as the high-histamine peanuts. Eggs can also be a trigger for some). As a supplement, PEA is available in tablet, capsule, and powder form and is considered a strong and safe natural painkiller and anti-inflammatory. More than 30 clinical trials so far have confirmed it can relieve complex pain (but also stated that more large-scale scientific research is needed). This scientific article concluded:
"PEA represents a promising addition to our therapeutic armamentarium for neuropathic pain, with potential for good tolerability and a low propensity for side effects."
It is also claimed that PEA can activate the cannabinoid receptors, protect the brain and heart, improve mood, reduce allergies, and may help fight the common cold. PEA also activates the energy-boosting, fat-burning, and anti-inflammatory PPAR alpha. This research paper states: "Palmitoylethanolamide (PEA), the naturally occurring amide of palmitic acid and ethanolamine, reduces pain and inflammation through an as-yet-uncharacterized mechanism. Here, we identify the nuclear receptor peroxisome proliferator-activated receptor-alpha (PPAR-alpha) as the molecular target responsible for the anti-inflammatory properties of PEA." In an analysis of 12 human studies, PEA supplements reduced chronic and neuropathic pain intensity without any serious adverse effects. It has to be used for at least 2 weeks to achieve pain relief. PEA was typically given over 3-8 weeks at dosages between 300 and 1200 mg/day. Taking it over a longer period of time strengthens its effects without causing tolerance. Normal dose is 300 or 600 mg/day, however: "At least 600 mg/day may be needed to relieve nerve pain, while doses of 1,2 g/day were used for diabetic nerve pain." You can read more favorable research outcomes in this article. One important benefit of it I like to name here is that PEA is said to reduce gut inflammation. I have a chronic low grade inflammatory condition of the gut (microscopic colitis) and it appears that many people with rosacea have in fact some issue or another with their gut and bowels (you can read my blog post about the link here). AND also depression! For what it's worth, I am truly not sure if this is really the wonder supplement that article makes it out to be :)
 PEA Reduces Gut Inflammation
PEA Reduces Gut Inflammation"PEA was successfully used to relieve symptoms of inflammatory bowel disease (IBS) in animals. Mice with chronic gut inflammation have low PEA levels, while PEA supplements normalized bowel movement and prevented damage to the gut lining. In tissues taken by biopsy from people with ulcerative colitis, PEA lowered inflammatory cytokines and the buildup of neutrophils, immune cells that worsen symptoms and contribute to gut damage."
"In a recent study of 58 people with depression, PEA (1,2 g/day) given over 6 weeks greatly and rapidly improved mood and overall symptoms. PEA was added to antidepressant treatment (citalopram) and lowered symptoms by an impressive 50%. This clinical study was a follow-up on numerous studies in which PEA improved symptoms of depression in animals."
PEA Reduces Histamine and Allergies
"PEA is a safe histamine-release blocker. People with allergies, histamine issues, and Th2-dominance will likely benefit from it. In animal and cell-based studies, PEA improved eczema and skin allergies by lowering mast cell activation and blocking the release of histamine. [..] In dogs with eczema, PEA helped soothe symptoms by reducing skin inflammation and itching. PEA reduced inflammatory substances (TNF alpha) and increased endocannabinoids in the skin (2-AG), which altogether strongly diminishes the allergic response." And there is more scientific info for now... Boring boring! But I want to share it anyway.
Blog posts from 2006, when I tried neurontin

 October 2006: I’m having problems with my right cheek ever since I fell asleep on an ice pack :S So silly... I can hit myself for it over and over again, but there's no real point. I felt a flush when I woke up in the middle of the night and took a cold pack from the freezer and wrapped it up in a cloth and wanted to have it on my cheek for only a little while, 5 minutes max, but because of the remeron, I fell straight asleep again (it really knocks you out half an hour after you took it, a real sleeping med actually as well). That happened while staying with friends in Ireland. Next day I instantly felt it was bad news, that affected cheek was stiff and burning and glowing and had some weird nerve pain. It has been one month now and the burning is pulsing, throbbing and almost constant. Nicely accompanied by redness. I will ask my dermatologist next week for a painkiller, but when I read about Lyrica, one of the side-effects mentioned is facial flushing! I know it is only rare, but still…we are so much more prone to such side-effects, with our bad blood vessels..
October 2006: I’m having problems with my right cheek ever since I fell asleep on an ice pack :S So silly... I can hit myself for it over and over again, but there's no real point. I felt a flush when I woke up in the middle of the night and took a cold pack from the freezer and wrapped it up in a cloth and wanted to have it on my cheek for only a little while, 5 minutes max, but because of the remeron, I fell straight asleep again (it really knocks you out half an hour after you took it, a real sleeping med actually as well). That happened while staying with friends in Ireland. Next day I instantly felt it was bad news, that affected cheek was stiff and burning and glowing and had some weird nerve pain. It has been one month now and the burning is pulsing, throbbing and almost constant. Nicely accompanied by redness. I will ask my dermatologist next week for a painkiller, but when I read about Lyrica, one of the side-effects mentioned is facial flushing! I know it is only rare, but still…we are so much more prone to such side-effects, with our bad blood vessels..Update: just saw my dermatologist and convinced him to let me try neurontin, but My God what a hard work it was to convince him. Got myself sort of into a difficult situation now. My GP is a very nice woman, and open for almost all my requests. I always bring some medical proof to support my requests. I've seen her a lot the last month, due to this nasty cheek, and she just prescribed me an antihistamine I wanted to try; hydroxyzine. Now the assistant would discuss with her today about neurontin. In the meanwhile my dermatologist called, he's just back from holiday. I explained my problems and asked for a 2 week trial of neurontin. He agreed, thought it was a good way of trying to figure out if it is a neuropathic problem or not. Then the GP's assistant called me back, saying the GP DOESN'T want to prescribe me the neurontin, because it is for epilepsy she thinks, and she totally disagrees. That is very unusual for her.. to explicitly say no. I feel that she must have grown tired of my constant demands for this and that, and I'm like a walking medicine cabinet, lol. SO, now I do have a prescription for the drug for two weeks and the green light from the dermatologist, which is most important of course, but I don't want to piss my GP off, since she is a very nice woman and has been invaluable for me over the past years. I don't want her to get really annoyed once she reads in her memo's (they all share it in one electronic database thing) that I DO take that neurontin now. What's best? I was thinking to just try it out, discuss it with the derm. in 2 weeks time, once (if) I can continue with it, let him write her a letter or give her a call and explain it to her. Unconventional medicine it seems, but it just might help me, you know? SIGH! Rolling Eyes Why is it all so difficult sometimes. The derm says it is quite hard to damage nerves, especially when the skin itself isn't really burned or damaged. Which isn't the case with me. But the cheek is still clearly red and marked where the cold pack was and I feel it constantly throbbing and it feels like I had acid smacked on it :( To be continued.. *Ok, I take 300 mg. at night now, second night last night, and when I woke up I was pale. I mean PALE, as a ghost. It has been a long time back since I looked like this. Now, after I ate something and started being busy I am back to my pink cheeks and the burning is still there, but not as sharp. Also I don't feel so spaced out as Wednesday. Have a bit more headaches, but that should pass I reckon. I will continue this drug for at least one or two weeks and then see and evaluate. I will also buy a blood pressure measurer today. Can buy one very cheap, and check it daily.
 Update. I have to say first that I don't take too much of this medicine: usually people take up to 1200 or 1600 mg a day as an average, and my doc prescribed me 900, of which I take 600 mg daily now. One tablet in the early evening and one before sleeping. The first side-effect (dizziness, bad coordination etc) have passed luckily, pretty quickly too. I do have to say that I have a bad cold, full nose etc. Together with a long list of side-effects, this is mentioned as happening 'often', in my meds enclosure leaflet. But nothing too bad. I have a blood pressure measuring thing, because another side-effect that happens often is supposed to be hypertension, and I take already another host of pills to lower that... So far my blood pressure if fairly low, the way I want it (I have check ups with my GP and dermatologist every now and then and they agree this is still ok for me): I'm around 98 over 60, still while on this medicine and the diclofenac, which raises blood pressure as well. And the bonus question: Does it still work for my burning and flushing? I think it does. I have had a bad day, but that was due to going to the football (soccer), getting all over excited when my team came back from a 3-1 score in the last 15 (I say 15!!) minutes to 3-4 in the last seconds, so that made me jump on my seat a lot. I also sinned on some chips (BAAAAD for me) and having hot weather here isn't helping either. But I still am more pale then usual I would say and the pain has definitely become less sharp. See how I'll be at the end of the week.(And my team won, yeaahhhh).
Update. I have to say first that I don't take too much of this medicine: usually people take up to 1200 or 1600 mg a day as an average, and my doc prescribed me 900, of which I take 600 mg daily now. One tablet in the early evening and one before sleeping. The first side-effect (dizziness, bad coordination etc) have passed luckily, pretty quickly too. I do have to say that I have a bad cold, full nose etc. Together with a long list of side-effects, this is mentioned as happening 'often', in my meds enclosure leaflet. But nothing too bad. I have a blood pressure measuring thing, because another side-effect that happens often is supposed to be hypertension, and I take already another host of pills to lower that... So far my blood pressure if fairly low, the way I want it (I have check ups with my GP and dermatologist every now and then and they agree this is still ok for me): I'm around 98 over 60, still while on this medicine and the diclofenac, which raises blood pressure as well. And the bonus question: Does it still work for my burning and flushing? I think it does. I have had a bad day, but that was due to going to the football (soccer), getting all over excited when my team came back from a 3-1 score in the last 15 (I say 15!!) minutes to 3-4 in the last seconds, so that made me jump on my seat a lot. I also sinned on some chips (BAAAAD for me) and having hot weather here isn't helping either. But I still am more pale then usual I would say and the pain has definitely become less sharp. See how I'll be at the end of the week.(And my team won, yeaahhhh). End of October 2006
End of October 2006My face was burning again and stupidly I took a cold pack from the freezer last night, wrapped it up well, but... fell asleep on it, again! Woke up with a pulsating flushed cheek, super red. I took extra diclofenac pills today, to bring the inflammation down hopefully. My right cheek has been very painful for 2 weeks now, even when it looks pale sometimes. The pain goes all over the cheek, from the ear to the nose, so over the cheekbone of the cheek. It is a burning, sharp pain, almost electrical. On the apple of that cheek, my skin has started to flake a bit. I am sure the incident with the cold pack in Ireland has really damaged both the skin and the nerves in that cheek. I have been eating the following lately:
-white beans; cooked and then baked crispy in a pan with oil. It doesn't seem to make me flushed. It has not too much histamine, tyramine or salicylates, or niacin content (B3 - can cause a flush).
-organic turkey meat
-soy beans
-sweet potatoes
-salad, with carrot, coconut oil, green beans and broccoli.
On Sunday I took 75 mg of carbamazepine. My skin was pink by then. At night I had a bad flushing attack however. Maybe I ate too many white beans! When I woke up my right cheek was burning and pretty red. And mt left cheek was red and swollen too. I don't know now if the carbamazepine is helping, or making me more flushed than normal. I also have to consider the chance that diclofenac is making the redness worse... One derm I see says it is fine to take for rosacea, another says that I shouldn't, as NSAID medication can worsen rosacea flushing and he compares it to steroids even (in the way it can trigger rosacea). I don't know what to belief and primarily want the nerve pain gone. because nerve pain means pain signals, means triggering of the blood vessels, means more flushing, means more pressure on the nerves, means more pain. I am getting exhausted by the worries and the constant battling of the nerve pain and flushing. I am actually a bit anxious at this point, a nagging background noise, constantly putting me on edge. I know from experience that anxiety makes my rosacea and flushing worse. Darn..... Also, as soon as I eat something and use my face muscles, the nerve pain gets worse. That isn't helping my anxiety either. My skin is pretty pink during the days now.
Start of November 2006
The week before my menstruation, my skin was terrible. Red, flushed and pimples on top. I went to a concert of Keane, an English band, on the 7th of November, and my skin behaved reasonably until the evening itself, when I stayed too long in a warm restaurant (oh the embarrassment of looking like a flaming lighthouse and people staring at me), and then in Ahoy I kept flushing. It was hard to enjoy the music.. I have stopped taking fish oil supplements, as I am convinced now it triggers my flushing and redness. High in histamine... fish oil.. I was silly to even try it I think.. The day after I started mexiletine (50 mg) for the nerve pain. The hours after taking it, I looked fairly pale. But in the evening I had a football (soccer) match to attend of the local team in town, and it was a skin nightmare; so flushed and red. I was burning up. I ate lamb meat instead of turkey meat that day, so perhaps that was the culprit. Or the mexiletine.. Once I started flushing, it continued for the entire evening. The next day I went back to my old regime and my skin cooled down a bit in the ays after. On Monday I added a claritine antihistamine to the mix, which made me more pale for some hours (I should say: less red). But after dinner I was red and flushed for hours again. I had eatenorganic beef, potaties and sald. Bleh, what misery this skin condition is at the moment :( The good news however is that the nerve pain in my right cheek seems to slowly but surely decrease. I stopped fish oil altogether. Might try alpha lipoic acid and/or vitamine C supplements soon. I am taking less diclofenac also, I feel I get more red when I take it. November/December 2006
November/December 2006Just saw my derm and he was very pleased and even a bit intrigued it seemed with the latest improvements. He wants me to continue with the gabapentine (neurontin), together with my other meds (YESS!), I was armed with some very bad and red before pics and pale after pics and with medical references about gabapentin working for hot flushes. There were 5 docs there gathered and they were impressed luckily. They wanted to keep the pics for documentation and said I was an exceptional case for them, since I'm the only one in the hospital that has such a bad case of vascular rosacea and flushing. Hmm, what an honor... :/ So far it seems that my strategy to attack my flushing from different angles is paying off. Low dose accutane is still another option, but I can't use it on top of all the other meds I already take probably and besides that, the dermatologist still wants to experiment with small scale IPL and Yag lasers treatments in the upcoming 4 months time. Since my other test patches are still a bit paler (both the IPL one and the YAG). No more full face treatments EVER for me, according to him (he agrees with Dr Chrouch on this one), but IF it does help locally, we will be facing a very long treatment plan...Luckily I don't seem to have to pay for them, since this is a professional hospital and no private clinic :) However, I am a bit skeptical and am only going to try another small area treatment with the machines here, to give it a chance. But my main trust and expectations are with Dr Chrouch, and not this old fashioned machine in this general hospital, where I have the dubious honor to be the exceptional case .. :S The gabapentin (neurontin) definitely makes my face less painful! Especially the right cheek burned non-stop before, no matter if it was red or pale and strong anti-inflammatories didn't help to calm any of that down. Now I only feel pain and burning when I have a real full face flush, which happens every day for maybe 30 minutes, usually around 18:00 when my body temp rises I think.. I found many links for gaba helping with menopausal hot flushes, which are in essence sort of similar to our rosacea flushings (linked to the sympathic nervous system being overactive or out of wack), according to my derm. So that might help, just as the fact that my face burns less and that by itself triggers less flushing. However there are also bad developments: the last 4 days I'm getting big red p&p's over my cheeks. Usually I never have them. And my nose cold just doesn't resolve: have had it now for almost the full time that I shave used this drug. The p&p's worry me the most. Not sure if the gabapentin is causing it. Did taper my dose down a bit today and maybe I will continue to do this and see if the skin get's better. But even on this lower dose the right cheek starts to burn and hurts and throbs again. :( This is not the way I would have liked things to go.. To be continued.. Oh and I had a mega flush after eating a bad of peanuts. Yeh what was I thinking... chuck full of histamine. It went OK for about half an hour after munching the bag full of them, then a mega flush came up and kept me up all night, with fan and cold packs. When will I ever learn. I also find that vitamine C tablets make me much more flushed and red. So exit multi vitamins in general for me. I had also cut down on my propranolol, god knows why, probably just to do something different in hope of improvement, but since I am back at taking 40 mg every 6 hours (so 4 times a day), I feel in general that my flushing is a little bit better controlled again. Although it's still a daily, hourly struggle to control the flushing and burning and redness I should add. I also went out to dinner with a friend and was a donkey, because I succumbed to eating a slice of pizza from her plate then feeling fatalistic about it, I ordered a huge ice cream with whipped cream for desert and wolfed it all down, also tasting my friends tiramisu. The weekend after my skin was a nightmare: very red and sore. I'm back on the health train now, taking 30 mg mirtazapine at night, moxonidine 4 times a day, propranolol 4 times a day and 1 50 mg pill of diclofenac at night. I also started to take fish oil again at night... I am so indecisive there, but I keep reading how it is supposed to control inflammation.
 Late(r) December 2006
Late(r) December 2006The nerve pain seems back lately and my skin is a right mess. Red, angry, flushed, painful. I'm tied to the house and the fan, what an utter misery this all is. My skin feels very tight and painful. I stopped taking fish oil several days ago, but don't see any effect, so still undecided on that one. My fingers are also red and swollen again. For several years, the doctor (GP) gave me penicillin for it, as a skin scrape (ell they took a round piece of skin out of my finger actually to investigate) showed streptococcus bacteria, but by now it has become clear that they were utterly useless (aaargghh, 2 weeks of pills for years and years in winter): I am having a condition called Raynaud's Syndrome! In hospital they put electrodes on my finger, then placed the hand in a bowl of water and slowly added ice cubes to the water, measuring my fingers blood vessels response. Raynaud's without a doubt. They advised against my anti flushing medication, and in favour of blood vessel DILATORS (shudder), but I said straight up that there is no chance in hell that I will take anything that makes my blood vessels dilate even more. They understood, going by my fire red face at that point. But penicillin is not going to do anything for my red swollen 'winter hands', we finally figured out by now. I just accept them. They're peanuts compared to my throbbing face.
The rash continued for a week, before I became suspicious of the glycerin that the shell/capsule of the pills is made of.
This might sound crazo, but I do have a weird immune system, that seems to react with flushing and inflammation to other substances, like gelatin or latex. I checked with the manufacturer and it appeared to be made from gelatin, made from pork skin. Ahum... I react to that stuff. So before stopping neurontin I decided to take it without the shell and most of the bad acne is gone by now. BUT, after 3 weeks I felt my flushing became worse again and after each dose of neurontin the flushing actually increased for a while. I found out that vasodilatation and hypertension are mentioned as appearing “frequent”, although this varies with different sites on the net, and others say it is only happens in 1% in controlled trials. My blood pressure increased from 90 over 68 to 120 over 80 (I have a little measure device). That is not good. And I've become very suspicious about the vasodilatation. Since I tapered off the gabapentin this week the pain in my cheek is back but hopefully I can convince my derm. to try another medicine. He will call me tomorrow. I’ll ask him for another painkiller: I checked the internet again, and looked for neuropathic pain. There is a special condition, when one side of the face has neuropathic pain, atypical facial neuralgia or something. Anyway: I checked all the medication that is mentioned there. Amitryptiline is an antidepressant that helps often for burning pain, but I used it a little while 3 years back and it made me flush very badly, so no more. The pharmacist later explained to me that it opens up the little blood vessels in the face, so that it was on the cards. There are other drugs, like SSRI’s (Paroxetine, Citalopram Effexor). To me carbamazepine (Tegretol) seems my best next shot. I checked it’s side-effects and they are usually mild and have nothing to do with hypertension, vasodilatation, flushing etc. Rash is mentioned unfortunately, but that’s the case with ALL anticonvulsants, and those are the drugs that can help blocking the pain sensations coming from the brain. I guess eventually there needs to be focus on why exactly my right cheek hurts and burns, even when it looks not very red. I will ask my derm this on the phone as well tomorrow.
 December 2006
December 2006 I've been taking neurontin for about 3 or 4 weeks now and at first it worked wonders, making me more pale and helping a lot with my neuropathic and burning pain. But after a couple of weeks I'm getting the feeling that it actually starts to make me a bit more red and even flushed sometimes. Very difficult to tell though and lately my right cheek is playing up again and has another sunburn-like reaction, so I take diclofenac (NSAID) with it to hopefully calm this redness and burning/ flushing on the right side down a bit... I noticed that "vasodilatation" and "hypertension" are mentioned as "frequent" side effects for neurontin. That is not flushing (which is noted for Lyrica), but still not good news. I wonder why I seemed to get more pale at it initially.. So to be really sure I have continue taking it for some time. When I didn't se improvement and only deterioration, I stopped taking it for some time and I had less frequent flushing. Then added the neurontin again, being a proper scientific researcher by now (or at least trying to be) and yep, within a day and for the few days I took it again, I had increased flushing, after an initial 'paling' effect (that's not a word, is it?) So I'll start trying another painkiller by Monday; Tegretol (carbamazepine). Carbamazepine doesn't have vasodilatation, flushing, hot flash or anything mentioned as side-effect. Flushing is mentioned with all the tricyclics, and my pharmacist explained that this drugs can widen the little blood vessels in the face), modern SSRI antidepressant (which give facial flushing as well often), anticonvulsants like Carbamazepine, phenytoin, gabapentin (or Lyrica) and lamotrigine and eventually certain antiarrhythmics, such as lidocaine and mexiletine. Also there are opiods, but they can cause facial flushing AS WELL (SIGHT................). So for anyone else I would bet on either gabapentine, which is registered as helpful for menopausal hot flashes as well (does something with the calcium channels and regulates body temperature, which is promising for us), or the carbamazepine, which I will try myself by next week, so I'll update on that one as well. They there is Trileptal (oxcarbazepine), which is a derivative from carbamazepine (Tegretol), like Lyrica from neurontin, but Trileptal has a high incidence of facial acne and depression, and I rather give the Tegretol a fair chance first. Besides: Tegretol has a proven track for the treatment of neuropathic pain and Trileptal has still studies running for this.
 Also have to add (shamed deeply) that I used a cool pack again 4 days ago and seemed to be back at square one with the right cheek: have a sunburn like reaction going on again, with redness, fierce burning, flushing and even some dryness/ scaling of the skin, so not good. I don't want to learn obviously :( Taking oral diclofenac now to help calm down the burn reaction and am at a low dose of gabapentin. Not sure at all now what causes what and it's a pretty difficult time for experimenting... UPDATE: ok, finally stopped with the gabapentin. It seams to really make my flushing worse now... Don't have a clue why it did work for the first weeks, but I stopped with it a while and then took it again in a three double blind trial mode, and the flushing went up, so I guess it has to do with the vasodilating action it can have.... Sad, but when I flush less I also have less burning and pain, so for me the priority lies with keeping my skin unflushed. It seems a bit like dragging water to the see if I continue taking this med and thereby aggravate the flushing : ( Another small chapter in this rosacea diary....
Also have to add (shamed deeply) that I used a cool pack again 4 days ago and seemed to be back at square one with the right cheek: have a sunburn like reaction going on again, with redness, fierce burning, flushing and even some dryness/ scaling of the skin, so not good. I don't want to learn obviously :( Taking oral diclofenac now to help calm down the burn reaction and am at a low dose of gabapentin. Not sure at all now what causes what and it's a pretty difficult time for experimenting... UPDATE: ok, finally stopped with the gabapentin. It seams to really make my flushing worse now... Don't have a clue why it did work for the first weeks, but I stopped with it a while and then took it again in a three double blind trial mode, and the flushing went up, so I guess it has to do with the vasodilating action it can have.... Sad, but when I flush less I also have less burning and pain, so for me the priority lies with keeping my skin unflushed. It seems a bit like dragging water to the see if I continue taking this med and thereby aggravate the flushing : ( Another small chapter in this rosacea diary.... January 2007
January 2007Things are progressively getting worse again. My skin is very red and reactive all day and I flush and burn a lot more again. I'm not sure why exactly. I do notice generally that I am doing better in the summer than in the winter. The fingers of my hands are very swollen and red as well and last month a temporary replacing dermatologist wasn't too sure about it and made me undergo some more blood tests to rule out increased ANA levels and some systemic conditions. Last week she called and there was only one blood test back, but it was not good: there are an alarming amount of "cryoglobulines" in my blood and new tests are needed to find out of there is an underlying condition, like lupus or others..I was tested on lupus before, and it came out negative, but she said that is no guarantee and it might have been masked or something. 13 February I have to see an immunologist and he or she we will look further into this. Somewhere I hope something will come out of this, so that there can be something done about my inflamed face and blood vessels altogether. But I have had so many tests in the past and so many disappointments, that I am preparing myself for the old answer that there is nothing to be found and I have to deal with it. To be continued.. I am currently not taking any medication for the neuropathic pain, but I did start with clonidine this week. Instead of the moxonidine I have been taking for almost 3 years. In Holland the brand I use is not available anymore this year and the generic gives me bad headaches. Apart from that I started to doubt recently if it still works for me, giving the bad state my skin is in. I also read about one of the side effects of it being facial flushing and vasodilatation and that raised some alarm bells. I contacted the manufacturers and they tried to find out if the drug causes only vasodilatation to the main big blood supplying arteries in the body or also to the peripheral blood vessels, in the face and hands for instance. They came back on it 2 weeks later and couldn't find anything about it. Clonidine on the other hand does have reports of vasoconstriction of the peripheral blood vessels and it supposedly helps for hot flushes, so I discussed it with Dr. Tony Chu, my doc in London, who has good experiences with it and gave me the green light for it. I have been using it now for a couple of days, together with 30 mg mirtazapine (Remeron) at night, which still works ok for me (for the flushing and as a mild antihistamine and antidepressant) and propranolol (40 mg, 3 times a day, also for the flushing) AND fish oil at night. Will post some bad flushing pics later.












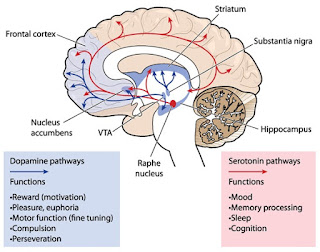

































No comments:
Post a Comment
scarletrosacea@gmail.com