 Facial flushing and redness are usually quickly associated with rosacea, but they can in fact be
symptoms of a different medical condition. Often when you visit a
dermatologist with rosacea symptoms, the diagnosis 'rosacea' is made
based on an evaluation of your clinical symptoms, which can be assessed
through a visual examination by your doctor or through an account of the
symptoms you describe. There is currently no clinical blood test to
determine if you have rosacea. When you have redness of the face
(especially the cheeks) and not of the rest of your body, plus transient
flushing issues and burning sensations of the skin, the diagnosis is often
easily made. Facial flushing is however not always a symptom of rosacea.
Brady Barrows wrote about this in a Rosacea Forum post: "To obtain a diagnosis of rosacea requires a physician to carefully evaluate the patient's history and an actual physical exam. There is currently no clinical test for rosacea and the judgement of the physician is the current only and proper way to obtain a diagnosis of rosacea. Sometimes the patient later finds out that it was misdiagnosed and turns out to be SD or something else. There are a few rosaceans who do not experience flushing and have a correct diagnosis of rosacea. Dr. Powell in his new book points out that flushing is not an absolute requirement for a diagnosis of rosacea. There are other reputable physicians who agree. However, this subject is one of the hotly debated subjects in the rosacea world. Some physicians, notably Dr. Kligman says that rosacea is a vascular disorder and flushing is one of the distinguishing characteristics for a diagnosis. While even Dr. Powell acknowledges that flushing is probably one of the most distinguishing characteristics in a diagnosis, he says he has seen patients with rosacea who do not flush any more than the general population and these patients do not report flushing. However, the inflammation or erythema associated with rosacea can cause the burning sensation that most rosaceans complain about. Flushing continues to probably be the most talked about and most concerned subject rosaceans discuss in all the rosacea forums and groups and rightly so. It is a major concern. However, flushing avoidance is simply one way to treat rosacea. There are other treatments available so focusing only on flushing might prove to be frustrating since there are other options available and it is difficult to avoid flushing for many."
Facial flushing and redness are usually quickly associated with rosacea, but they can in fact be
symptoms of a different medical condition. Often when you visit a
dermatologist with rosacea symptoms, the diagnosis 'rosacea' is made
based on an evaluation of your clinical symptoms, which can be assessed
through a visual examination by your doctor or through an account of the
symptoms you describe. There is currently no clinical blood test to
determine if you have rosacea. When you have redness of the face
(especially the cheeks) and not of the rest of your body, plus transient
flushing issues and burning sensations of the skin, the diagnosis is often
easily made. Facial flushing is however not always a symptom of rosacea.
Brady Barrows wrote about this in a Rosacea Forum post: "To obtain a diagnosis of rosacea requires a physician to carefully evaluate the patient's history and an actual physical exam. There is currently no clinical test for rosacea and the judgement of the physician is the current only and proper way to obtain a diagnosis of rosacea. Sometimes the patient later finds out that it was misdiagnosed and turns out to be SD or something else. There are a few rosaceans who do not experience flushing and have a correct diagnosis of rosacea. Dr. Powell in his new book points out that flushing is not an absolute requirement for a diagnosis of rosacea. There are other reputable physicians who agree. However, this subject is one of the hotly debated subjects in the rosacea world. Some physicians, notably Dr. Kligman says that rosacea is a vascular disorder and flushing is one of the distinguishing characteristics for a diagnosis. While even Dr. Powell acknowledges that flushing is probably one of the most distinguishing characteristics in a diagnosis, he says he has seen patients with rosacea who do not flush any more than the general population and these patients do not report flushing. However, the inflammation or erythema associated with rosacea can cause the burning sensation that most rosaceans complain about. Flushing continues to probably be the most talked about and most concerned subject rosaceans discuss in all the rosacea forums and groups and rightly so. It is a major concern. However, flushing avoidance is simply one way to treat rosacea. There are other treatments available so focusing only on flushing might prove to be frustrating since there are other options available and it is difficult to avoid flushing for many." Unfortunately long term facial flushing episodes can worsen your rosacea, both in terms of increases baselines redness as well as increased flushing attacks and lowered flushing threshold. That means the burning often worsens too over time. Hence why trying to avoid flare ups can help to stabilize the condition. For many it's progressive by nature. One flushing episode can subside and leave your rosacea unchanged, and a year of on and off flushing might as well, but years on end usually do not :/ I also found several medical sites where specialists claim that ongoing facial flushing (for instance from menopausal hot flashes, from carcinoids or from anything else basically) can cause the development of rosacea in the long run. Flushing can become a serious, life altering thing if you don't tackle it at some point..
*Clevelandclinic states: "Repeated flushing over a prolonged period can lead to telangiectasia and occasionally to classic rosacea of the face. [..] Patients with severe flushing caused by mastocytosis can develop rosacea in less than 1 year after the onset of flushing episodes."
(Freedberg IM, Eisen AZ, Wolff K, et al (eds): Fitzpatrick’s Dermatology in General Medicine, 5th ed., vol. 1. New York: McGraw Hill, 1993, pp 142-1659.)
*Wiki states regarding hot flashes: "Excessive flushing can lead to rosacea."
*Dr. Mehmet Oz (love his show) wrote: "Hot flashes and the flushing they cause may trigger rosacea flare-ups."
*Dr. Richard Wagner wrote: "Actually, carcinoid syndrome can cause rosacea because of the chronic flushing"
And an interesting article on flushing from the Cleveland Clinic states:
"Flushing can be an exaggeration of a physiologic process or a manifestation of a serious condition that needs to be identified and treated. [The term] flushing describes episodic attacks of redness of the skin together with a sensation of warmth or burning of the face, neck and, less frequently, the upper trunk and abdomen. It is the transient nature of the attacks that distinguishes flushing from the persistent erythema of photo-sensitivity or acute contact reactions. Repeated flushing over a prolonged period can lead to telangiectasia and occasionally to classic rosacea of the face."
It goes on to give a (very thorough) definition of flushing;
"Redness of the skin may be caused by an increased amount of saturated hemoglobin, an increase in the diameter or actual number of skin capillaries, or a combination of these factors. Flushing is caused by increased blood flow through the skin, causing warmth and, because of engorgement of the subpapillary venous plexus, redness. The vasodilation of flushing may be caused by a direct action of a circulatory vasodilator substance—for example, histamine—or it may be caused by changes in the neurologic control of the cutaneous vasculature in the affected areas. In the face, neck and upper trunk, where flushing is most frequent, the neurologic control of vascular tone is predominantly exerted by autonomic vasodilator nerve fibers. These fibers are found in somatic nerves supplying the affected skin, including the trigeminal nerve. Because autonomic nerve fibers also supply eccrine sweat glands, neurally activated flushing is frequently associated with sweating (wet flushing) as opposed to flushing caused by circulating vasodilator mediators, which frequently does not involve sweating (dry flushing). The presence or absence of sweating has therefore been proposed as a clinical guide to the mechanisms of flushing, although in practice this is not always reliable. Examples of wet flushing are physiologic flushing and menopausal flushing. An example of dry flushing is niacin-provoked flushing."
It also explains why flushing predominantly happens in the facial area: "The diameter of the blood vessels of the cheeks is wider than elsewhere, the vessels are nearer to the surface and there is less tissue thickness obscuring them. This may explain why flushing occurs in that limited distribution. Polycythemia produces the characteristic ruddy complexion, but it may also cause a peculiar coloration termed erythremia, which is a combination of redness and cyanosis. The tongue, lips, nose, earlobes, conjunctivae and fingertips especially demonstrate this coloration. Erythremia results when there is a combination of increased amounts of saturated and desaturated hemoglobin."
 Clock Rosacea or Systemic Flushing
Clock Rosacea or Systemic FlushingFlushing or facial skin redness is more likely to occur when the body temperature is elevated. You could say that the body operates on a clock. Hospital physicians have known for years that the lowest body temperature of the 24 hour day is usually around 3 to 4 AM, whilst the highest temperature of the day is generally between 7 to 8 PM. The average rosacea sufferer does not have hospital waking and sleeping hours, therefore their temperature lows and highs may vary 3 to 5 hours each way. A high temperature for some may start as early as at 3 PM. The symptoms of flushing usually occur when the body becomes fatigued and/or stressed, which stimulates the sympathetic nervous system. Any activation of these nerves causes vasoconstriction of 'blood vessels' - except in the 'facial blush/flush areas' where it induces potent vasodilatation of the facial skin or flushing with the resulting 'rosacea redness'.
Stress stimulates the sympathetic nervous system.
Lack of sleep stimulates the sympathetic nervous system, with a minimum of 8 to 9 hours of sleep being needed nightly.
Anxiety (fight or flight) stimulates the sympathetic nervous system.
Increase in internal body temperature stimulates the sympathetic nervous system, whereas obviously a decrease in body temperature decreases the sympathetic system due to the parasympathetic system calming the system (source).
Heavy meals and sugar/carbohydrates can also cause flushing (see the subtopic 'Allergies/ Food allergies/intolerance/ coeliac disease' below for more on that).
Steroids can cause flushing (see the subtopic 'Drug Related Flushing' below for more on that).
Exercise Flushing
Exercise flushing is caused by the cardiovascular system pumping harder and faster when you exercise, resulting in blood vessel dilation. Not only because your blood pressure increases, but also as a natural way to release body heat. The key is to minimize vascular dilation while exercising, in order to reduce the symptoms of facial skin redness. Exercise should therefore be done moderately in a cool area, while keeping the body well hydrated to minimize the facial skin redness. It's best to adapt slowly over time to your exercise regime, so that the body is aerobic (with oxygen) instead of anaerobic (without oxygen causing redness.) Therefore, you can handle more vigorous exercise as your exercise training increases. Better cardiovascular shape and exercise means more oxygen in the blood, which constricts blood vessels (source).
Cold Weather Flushing and Warm Room Flush
These flushing flare ups result from coming from the cold into a warm room. While the rosacea sufferer is outside in the cold weather, the cardiovascular system is pumping hard. However, the extremities such as the feet, hands, ears and nose get less blood supply than the rest of the body. It's partially due to direct contact, but it is more a result of conservation of heat by internal thermostat -- causing constriction of vessels by decreasing sympathetic activity to vessels (similar to taking a 'cool' shower.) When the rosacea sufferer then enters a warm office or home, the indoor temperatures quickly warm the facial skin and extremities while the cardiovascular system is still in a moderately high exercise mode. Resulting in a flush. It can help to make the transition from cold to warm more smooth. Either by allowing the skin to adjust to a warmer indoor temperature slowly (warming up the car prior to use for instance, or wearing a facial mask/hat/scarf depending on length of exposure and severity of cold temperatures, or walking or cycling more slowly when you start to approach your work or destination). After being exposed to the cold for a long period, try to enter the building slowly so the cardiovascular system will not be as stimulated, and then proceed slowly into the warmer office/home to minimize facial redness and flushing. This is a very insightful and important pdf article about the warm room flush. I also explained the whole theory extensively in this blog post. It comes down to advising people with rosacea to avoid extreme temperature changes. So to not make your house ice cold with an air-conditioner running all the time for instance, because it means that your blood vessels will disproportionately expand once you go a place with normal temperatures. You create rebound flushing so to speak, and the advice is to keep your skin adjusted to average temperatures. There is a lot more to read there however, so please check it out if you haven't heard of it yet.
Even 'normal' and healthy people can flush
This is an explanation from the cleveland clinic of normal (physiological) flushing response: Embarrassment or anger may cause flushing in some individuals in whom the threshold for this response may be low or the reaction itself unusually intense; this is also known as blushing. If necessary, propranolol or another beta blocker may be used to alleviate this symptom. Heat causes flushing in many people and overheating can lower the threshold for flushing from other causes, such as the menopause. Overheating (for instance after exercise or a sauna visit) can cause physiological flushing because of the effect of the rise in blood temperature on the thermoregulatory center in the anterior hypothalamus. A similar mechanism is responsible for facial flushing caused by hot drinks, which produces a rise in temperature of the blood in the oral cavity, in turn leading to an increase in temperature of blood perfusing the hypothalamus. The temperature of hot coffee, rather than its caffeine, can also cause flushing. A useful maneuver for patients faced with a brief thermal exposure is to suck on ice chips carried in an insulated cup. This attenuates flushing for the first 20 to 30 minutes.
Alcohol has been left out, but can obviously also cause flushing: "Asians with certain genotypes show extensive flushing in response to low doses of alcohol. They have been found to have higher plasma levels of acetaldehyde. This abnormality is probably related to a deficiency of an isoenzyme of liver aldehyde dehydrogenase. This population can be detected by using an ethanol patch test, which produces localized erythema. A special type of alcohol flush is also associated with chlorpropamide, the oral antihyperglycemic agent. Even small amounts of alcohol provoke intense flushing within a few minutes of ingestion. This flushing is not associated with sweating but, in some cases, tachycardia, tachypnea, and hypotension may be seen. The flush is mediated by elevated acetaldehyde plasma levels and possibly by the release of prostaglandins. Alcohol ingestion can also trigger flushing in those with carcinoid tumors, mastocytosis, medullary thyroid carcinoma, and certain lymphoid tumors. Trichloroethylene, a chemical that has been abandoned in recent years because of its carcinogenic potential, can cause flushing. When inhaled following ingestion of alcoholic beverages, a striking cutaneous reaction results, consisting in the sudden appearance of erythema of the face, neck, and shoulders, a reaction that has been termed degreaser’s flush. Nausea and vomiting can also occur." Plus; alcohol is a blood vessel dilator and can cause even normal skin to blush or flush. The same goes for coffee and caffeine. Also, a night of drinking alcohol will cause your blood to have a measurable increased level of inflammation the next day. This is partly responsible for the 'hangover' feeling; it's like having the flu, scientists say. For rosacea patients, having inflammatory substances in the blood is obviously not going to be good for our skin redness either.
This is an explanation from the cleveland clinic of normal (physiological) flushing response: Embarrassment or anger may cause flushing in some individuals in whom the threshold for this response may be low or the reaction itself unusually intense; this is also known as blushing. If necessary, propranolol or another beta blocker may be used to alleviate this symptom. Heat causes flushing in many people and overheating can lower the threshold for flushing from other causes, such as the menopause. Overheating (for instance after exercise or a sauna visit) can cause physiological flushing because of the effect of the rise in blood temperature on the thermoregulatory center in the anterior hypothalamus. A similar mechanism is responsible for facial flushing caused by hot drinks, which produces a rise in temperature of the blood in the oral cavity, in turn leading to an increase in temperature of blood perfusing the hypothalamus. The temperature of hot coffee, rather than its caffeine, can also cause flushing. A useful maneuver for patients faced with a brief thermal exposure is to suck on ice chips carried in an insulated cup. This attenuates flushing for the first 20 to 30 minutes.
Alcohol has been left out, but can obviously also cause flushing: "Asians with certain genotypes show extensive flushing in response to low doses of alcohol. They have been found to have higher plasma levels of acetaldehyde. This abnormality is probably related to a deficiency of an isoenzyme of liver aldehyde dehydrogenase. This population can be detected by using an ethanol patch test, which produces localized erythema. A special type of alcohol flush is also associated with chlorpropamide, the oral antihyperglycemic agent. Even small amounts of alcohol provoke intense flushing within a few minutes of ingestion. This flushing is not associated with sweating but, in some cases, tachycardia, tachypnea, and hypotension may be seen. The flush is mediated by elevated acetaldehyde plasma levels and possibly by the release of prostaglandins. Alcohol ingestion can also trigger flushing in those with carcinoid tumors, mastocytosis, medullary thyroid carcinoma, and certain lymphoid tumors. Trichloroethylene, a chemical that has been abandoned in recent years because of its carcinogenic potential, can cause flushing. When inhaled following ingestion of alcoholic beverages, a striking cutaneous reaction results, consisting in the sudden appearance of erythema of the face, neck, and shoulders, a reaction that has been termed degreaser’s flush. Nausea and vomiting can also occur." Plus; alcohol is a blood vessel dilator and can cause even normal skin to blush or flush. The same goes for coffee and caffeine. Also, a night of drinking alcohol will cause your blood to have a measurable increased level of inflammation the next day. This is partly responsible for the 'hangover' feeling; it's like having the flu, scientists say. For rosacea patients, having inflammatory substances in the blood is obviously not going to be good for our skin redness either.
There are a lot of possible underlying causes and medical conditions for facial flushing
 Not many
people are submitted to (blood) tests or skin scraping biopsy by their
dermatologist though, and for rosacea these are usually non
confirmative anyway. Skin biopsy can exclude an infection however, and
some doctors are able to test for demodex mites that way (but it's still
not a widely used method). Demodex mites seem to mostly be at
play (and this is still debated) with the papular subtype of rosacea;
those with persistent redness and p&p's. When your skin is 'clean'
and mainly deals with redness (erythema) and flushing, my dermatologists
told me demodex is not at play. I hope they are right :) I wrote more about demodex in rosacea here.
Not many
people are submitted to (blood) tests or skin scraping biopsy by their
dermatologist though, and for rosacea these are usually non
confirmative anyway. Skin biopsy can exclude an infection however, and
some doctors are able to test for demodex mites that way (but it's still
not a widely used method). Demodex mites seem to mostly be at
play (and this is still debated) with the papular subtype of rosacea;
those with persistent redness and p&p's. When your skin is 'clean'
and mainly deals with redness (erythema) and flushing, my dermatologists
told me demodex is not at play. I hope they are right :) I wrote more about demodex in rosacea here. David Pascoe wrote about this topic: "Cutaneous flushing—a common presenting complaint to dermatologists, allergists, internists and family practitioners—results from changes in cutaneous blood flow triggered by multiple conditions. Most cases are caused by very common, benign diseases such as rosacea or climacterum, that are readily apparent after a thorough taking of history and physical examination. However, in some cases, accurate diagnosis requires further laboratory, radiologic, or histopathologic studies to differentiate several important clinicopathologic entities. In particular, the serious diagnosis of carcinoid syndrome, pheochromocytoma, mastocytosis or anaphylaxis needs to be excluded by laboratory studies. If this work-up is unrevealing, rare causes such as medullary carcinoma of the thyroid, pancreatic cell tumor, renal carcinoma and other should be considered."
PLUS: A lot of people with rosacea suffer from other health problems, which are often overlooked by doctors. For instance, many report and complaint about bowel disturbances, different types of inflammation in the body (of the joints for instance), other autoimmune diseases, allergies, thyroid or hormone issues. Even when people manage to get these coexisting health issues diagnosed, it is often very daunting to find a doctor (usually a dermatologist) who is capable and willing to look at the bigger scheme of things and treat you appropriately. I have for instance seen an immunologist, internist, rheumatologist and a dermatologist for various inflammatory health conditions, and none of them were up to communicating with one another to come to a more coherent, overlapping treatment plan. Despite me asking for it :( I was first diagnosed with rosacea back in 2002, after 3 years of rosacea symptoms. Then I was diagnosed with having Raynaud's syndrome (causing disturbed vascularity in hands and feet, giving often red swollen fingers and feet). I was then diagnosed and re-diagnosed (through colonoscopy surgery) over the years with colitis. More specific, with microscopic lymphocytic colitis plus with irritable bowel syndrome. Then an internist detected elevated ANA levels (went from very mildly elevated, 1:40, to slightly more elevated, 1:80 over the past 4 years - has to do with how many times a sample of your blood needs to be diluted to get to zero auto antibodies in the sample, from what I remember, and the number at the end shows that number of times), but they don't deem this serious enough to start any treatment. Besides, from what I was told this elevated ANA marker is mainly an indication that there is some sort of autoimmune activity going on in the body, possible resulting in elevated inflammatory markers and levels inside. But these markers on their own don't say a whole lot and doctors often also look for clinical symptoms. Since I do not have the clinical symptoms of lupus for instance, they leave the markers for what they are and retest every few years. I also have some sort of arthritis in my knees (since puberty). Then a professor immunologist did very extensive immune blood work tests in 2011, which showed increased inflammation markers in the blood and some elevated cells which indicated an autoimmune disease. But again, these markers weren't going through the roof, so doctors left it at that. So there are a couple of underlying issues going on, but none are really treated and I am left with anti flushing medication, diet, exercise and eliminating triggers to keep my rosacea and bowel issues calm. I can look pregnant at times from the bloating, but it's not painful or anything and I try to avoid wearing tight clothes around the waist and gas producing foods.
This research shows that many rosacea patients have positive ANA levels, which are the indicator for auto immune activity.
"Fifty four of 101 rosacea patients (53.46%) had an ANA titer of 1:160 or higher. Twenty-four patients (23.76%) had the borderline ANA titer of 1:160. Titers of 1:320 and 1:640 were present in 14 (13.86%) and 9 (8.91%) patients, respectively. ANA titers of 1:1,280 to 1:2,560 were present in 7 patients (6.93%). In the control group, ANA titers of 1:160 and 1:320 were observed in 1 person each, out of 26 (7.68%) patients." Mine is mildly positive too. Negative is zero or 1:20.
Below I will discuss some other medical conditions which can cause rosacea-like symptoms, such as facial flushing, burning and redness. There are some standard tests that your doctor can order to eliminate some of these other potential causes. There is also a little summary of the experience rosacea patients have with diagnosing their rosacea/health problems.
Please note that I am not a doctor. All I do is research online and in books what rosacea might be like, look like etc. I also share whatever info I have received from my rosacea specialists and other dermatologists I see or have seen over the years. The information here is gathered by me and put in a (hopefully) comprehensive overview, including symptom description, images of diseases and comparisons with rosacea symptoms. In order to make it easier for rosacea patients - or those suffering from facial flushing - to inform themselves about other illnesses that can potentially cause their symptoms. I try to link to all the sources I used and I want to stress that I do not (and can not) give any medical advice, nor want to be responsible for people diagnosing themselves. This should be done by a qualified doctor at all times. However, as many doctors seem unsure themselves often about the causes of facial flushing, this information here might help you to get some ideas of what to test for. I tried to make it easier to oversee all this information, as it took me forever to find all this information due to it being scattered all over the internet. I also share my personal experiences and thoughts on rosacea on this blog. Pictures included in this post are mostly taken from a series of around 2,500 'special photographs' taken by the New South Wales Police Department photographers. They depict mugshots from convicted criminals in Australia, shot between 1910-1930. I chose them to illustrate how these flushing causing diseases discussed here also are 'usual suspects' in their own right.
Diseases and medical conditions which can cause facial flushing, burning and redness
Seborrheic dermatitis/eczema
Lupus erythematosus
Systemic mastocytosis (and other histamine intolerances)
Hormone imbalances/Menopause
Drug related flushing
Allergies/ Food allergies/intolerance/ coeliac disease
Erythromelalgia (EM) is also a very rare cause of facial flushing
Keratosis Pilaris Rubra faceii
Carcinoid Syndrome/pheochromocytoma
Polycythemia vera
Mixed connective tissue disease
Thyroid problems
Helicobacter infection/ SIBO
Photosensitivity
Harlequin Syndrome
Auriculotemporal Nerve Syndrome (Frey’s Syndrome)
Flushing with Pseudo carcinoid Syndrome in Secondary Male Hypogonadism
Erysipelas
Other Diseases Causing Episodic Flushing (including asthma, epilepsy, Lyme disease, POTS and ROSACEA)
Steps to take for Evaluation Of The Patient With A Flushing Disorder
Coexisting health problems which people with rosacea often mention
A little summary of the experience rosacea patients have with diagnosing their rosacea and at times underlying coexisting health problems
This wikipedia article mentions more causes for facial flushing.
Seborrheic dermatitis/eczema
 Seborrheic dermatitis, or seb derm, is often misdiagnosed as rosacea. Or patients have both conditions and one worsens the other. Seb derm is a common skin disorder that mainly manifests itself on the scalp and facial T-zone (forehead, eyebrows, sides of nose and mouth) causing scaly, itchy, red skin and stubborn dandruff. Seborrheic dermatitis can also affect the upper chest, back and other areas of your body that have many oil (sebaceous) glands. On the scalp, seborrhoeic dermatitis usually causes roughly defined, dry pink or skin colored patches with yellowish or white bran-like scales. In winter the seb derm causes my (rosacea) skin to turn scaly and rough and red. This makes the skin around my mouth and on the inner cheeks and in the eyebrows stand out in a red color. The cause of seb derm isn't fully understood yet, as far as I can tell from the information that's out there online and from the dermatologists I´ve seen. What I understand at this point in time, is that seb derm might have an underlying autoimmune component to it. The skin responds badly to a common yeast that lives on it. This normal skin inhabitant is called Malassezia (formerly known as Pityrosporum ovale). Patients with seborrhoeic dermatitis appear to have a reduced resistance to this yeast and the toxic substances that it produces. Unlike in healthy people, it creates inflammation and skin irritation in us seb derm patients. An overproduction of sebum is also mentioned as a cause and there is an increased turnover of shedding of the skin (hence the flaking). In some cases, the seb derm is actually precursor of psoriasis...
Seborrheic dermatitis, or seb derm, is often misdiagnosed as rosacea. Or patients have both conditions and one worsens the other. Seb derm is a common skin disorder that mainly manifests itself on the scalp and facial T-zone (forehead, eyebrows, sides of nose and mouth) causing scaly, itchy, red skin and stubborn dandruff. Seborrheic dermatitis can also affect the upper chest, back and other areas of your body that have many oil (sebaceous) glands. On the scalp, seborrhoeic dermatitis usually causes roughly defined, dry pink or skin colored patches with yellowish or white bran-like scales. In winter the seb derm causes my (rosacea) skin to turn scaly and rough and red. This makes the skin around my mouth and on the inner cheeks and in the eyebrows stand out in a red color. The cause of seb derm isn't fully understood yet, as far as I can tell from the information that's out there online and from the dermatologists I´ve seen. What I understand at this point in time, is that seb derm might have an underlying autoimmune component to it. The skin responds badly to a common yeast that lives on it. This normal skin inhabitant is called Malassezia (formerly known as Pityrosporum ovale). Patients with seborrhoeic dermatitis appear to have a reduced resistance to this yeast and the toxic substances that it produces. Unlike in healthy people, it creates inflammation and skin irritation in us seb derm patients. An overproduction of sebum is also mentioned as a cause and there is an increased turnover of shedding of the skin (hence the flaking). In some cases, the seb derm is actually precursor of psoriasis...
Differentiating rosacea from seb derm
 |
Seb derm treatment options
*Ketoconazole cream or shampoo (1 or 2%)
*Zinc pyrithione shampoo
*5% sulfur / 10% sulfacetamide lotion and or wash
*Lamisil cream
*Salicylic acid
*Ciclopirox cream / ciclopiroxolamine
*Elidel or Protopic cream (pimecrolimus cream or tacrolimus ointment). (Note: both made my rosacea flare, even when applied very locally on the areas around the mouth)
*Hydrocortisone or steroid creams (would absolutely warn against this in case you also have rosacea! Steroids can very quickly stir up or worsen the rosacea).
*Tar cream can be applied to scaling areas and removed several hours later by shampooing.
*Severe cases may receive a course of tetracycline antibiotics, oral antifungal medication, or sometimes, ultraviolet radiation.

.JPG) There are also more natural treatment options
There are also more natural treatment options
including raw honey and virgin coconut oil. (not scientifically proven to be effective!) Some people use apple cider vinegar or tea tree oil on their seb derm and find it helpful. Watching your diet and avoiding foods with a lot of yeast (certain breads), high levels of simple sugars and certain fermented foods also helps some patients. Dairy products might also add to the problem for some. On the other hand, some other foods have been mentioned to help combat the seb derm, including garlic (anti fungal and anti inflammatory actions), coconut oil (idem) and probiotics. For me the ketoconazole cream does the job very well. I use ketoconazole 2% and find it very effective in controlling (and in winter limiting) my seb derm rashes nowadays. Because of my very delicate and sensitive, flushing prone rosacea skin, I normally can't even tolerate a neutral base cream (I normally use nothing on my skin). However, my cheeks are the most sensitive and affected and the seb derm usually shows up around my nose and mouth folds, where my skin can handle the ketoconazole 2% cream. The alcohol in it irritates it though and for the past 4 years my (big hospital related) pharmacy makes a special cream for me. It contains 2% ketoconazolum (the active ingredient) and they make a neutral base for it from cetomacrogol, with no alcohols and no preservatives added. In my case it contains the following (30 gram tube):

.JPG) There are also more natural treatment options
There are also more natural treatment optionsincluding raw honey and virgin coconut oil. (not scientifically proven to be effective!) Some people use apple cider vinegar or tea tree oil on their seb derm and find it helpful. Watching your diet and avoiding foods with a lot of yeast (certain breads), high levels of simple sugars and certain fermented foods also helps some patients. Dairy products might also add to the problem for some. On the other hand, some other foods have been mentioned to help combat the seb derm, including garlic (anti fungal and anti inflammatory actions), coconut oil (idem) and probiotics. For me the ketoconazole cream does the job very well. I use ketoconazole 2% and find it very effective in controlling (and in winter limiting) my seb derm rashes nowadays. Because of my very delicate and sensitive, flushing prone rosacea skin, I normally can't even tolerate a neutral base cream (I normally use nothing on my skin). However, my cheeks are the most sensitive and affected and the seb derm usually shows up around my nose and mouth folds, where my skin can handle the ketoconazole 2% cream. The alcohol in it irritates it though and for the past 4 years my (big hospital related) pharmacy makes a special cream for me. It contains 2% ketoconazolum (the active ingredient) and they make a neutral base for it from cetomacrogol, with no alcohols and no preservatives added. In my case it contains the following (30 gram tube):
-2% Ketoconazolum 0,600 gram
-cera cetomagrogolis emulsion 4,500 g.
-decylis oleas (cetiol V) 6,000 ML
-aqua purificata bag in box 17,700 ML
-Sorbitolum 70% crist 1,200 ML
The pharmacist removed the preservative from the cetomacrogol, which is a bit of a waxy like cream and very neutral. The above pictures were taken in a bad seb derm year, the winter of 2010 when I didn't use the ketoconazole cream yet. The white dots are metronidazole cream and zinc cream; I was silly enough by then to think the metrocream would work for the seb derm. You can read more about seb derm in this older blog post from me on the matter. Below are some other photos of seb derm skin.
-cera cetomagrogolis emulsion 4,500 g.
-decylis oleas (cetiol V) 6,000 ML
-aqua purificata bag in box 17,700 ML
-Sorbitolum 70% crist 1,200 ML
The pharmacist removed the preservative from the cetomacrogol, which is a bit of a waxy like cream and very neutral. The above pictures were taken in a bad seb derm year, the winter of 2010 when I didn't use the ketoconazole cream yet. The white dots are metronidazole cream and zinc cream; I was silly enough by then to think the metrocream would work for the seb derm. You can read more about seb derm in this older blog post from me on the matter. Below are some other photos of seb derm skin.

Lupus erythematosus

Lupus erythematosus (LE/SLE) is an autoimmune disease. It can be mistaken for rosacea (or vice versa) because lupus can also produce a red rash on the face, the so called Butterfly rash. However, it is an entirely different, systemic autoimmune disease (or autoimmune connective tissue disease) that can affect any part of the body. As with most autoimmune diseases, the immune system of a lupus patient attacks the own body, in this case its cells and tissue. Resulting in inflammation and tissue damage. It is both a type II and a type III hypersensitivity reaction in which bound antibody-antigen pairs (immune complexes) precipitate and cause a further immune response. Wiki says about it: "SLE most often harms the heart, joints, skin, lungs, blood vessels, liver, kidneys, and nervous system. The course of the disease is unpredictable, with periods of illness (called flares) alternating with remissions. The disease occurs nine times more often in women than in men, especially in women in childbearing ages 15 to 35, and is also more common in those of non-European descent. There is no cure for SLE. It is treated with immunosuppression, mainly with cyclophosphamide, corticosteroids and other immunosuppressants. SLE can be fatal. The leading cause of death is from cardiovascular disease due to accelerated atherosclerosis. Survival for people with SLE in the United States, Canada, and Europe has risen to approximately 95% at five years, 90% at 10 years, and 78% at 20 years, and now approaches that of matched controls without lupus. Lupus is Latin for wolf. In the 18th century, when lupus was just starting to be recognized as a disease, it was thought that it was caused by the bite of a wolf. This may have been because of the distinctive rash characteristic of lupus. (Once full-blown, the round, disk-shaped rashes heal from the inside out, leaving a bite-like imprint.)"
Signs and symptoms
SLE is one of several diseases referred to as "the great imitators" because it often mimics or is mistaken for other illnesses. SLE symptoms vary widely and come and go unpredictably. They range from limited skin disease at one end of the spectrum to a life threatening disease that invades organs of the body at the other. Diagnosis can thus be elusive, with some people suffering unexplained symptoms of untreated SLE for years. Common initial and chronic complaints include fever, malaise, joint pains, myalgias, fatigue, and temporary loss of cognitive abilities. Because they are so often seen with other diseases, these signs and symptoms are not part of the diagnostic criteria for SLE. When occurring in conjunction with other signs and symptoms (see below), however, they are considered suggestive.
Dermatological Micrograph can show vacuolar interface dermatitis, as may be seen in SLE. As many as 30% of sufferers have some dermatological symptoms (and 65% suffer such symptoms at some point), with 30% to 50% suffering from the classic malar rash (or butterfly rash) associated with the disease. Some may exhibit thick, red scaly patches on the skin (referred to as discoid lupus). Hair loss, mouth, nasal, urinary tract and vaginal ulcers, and lesions on the skin are other possible manifestations. Tiny tears in the delicate tissue around the eyes can occur after even minimal rubbing. Focusing in on the skin problems you could experience with lupus erythematosus:
 Discoid lesions
Discoid lesions
These are scarring, coin-shaped lesions commonly seen in areas of skin
that are exposed to light, such as the scalp and ears, and the central
portion of the face and nose. More rarely, your lips, mouth, and tongue
might be involved. These lesions can produce a scarring baldness and
because they often affect the face, you may consider getting cosmetic
treatment. Only 1 in 10 to 1 in 20 of patients who are initially
diagnosed with this type of skin involvement will eventually develop the
severe form of the disease that involves other organs in your body.
Subacute cutaneous lesions
These are non-scarring, red and scaly lesions that are very
photosensitive: they get worse when they are exposed to
ultraviolet light. They tend to occur on the face in a butterfly shape or can be more widespread on the body. Even though these lesions do not result in scarring, their extent and color change can cause major cosmetic concerns. About half of the patients who are diagnosed with this type of skin involvement will, in time, develop other organ involvement (also called systemic involvement or systemic disease), such as arthritis conditions. The butterfly rash is seen in up to 2/3 of patients with systemic disease and may be the presenting feature in up to 40%. It may vary in degree from a mild redness or “rosy cheeks”, to multiple swollen red areas or plaques.
Lupus profundus
This is a rare type of skin lupus erythematosus, in which the
subcutaneous fat is involved giving rise at first to tender nodules that
can leave, in time, saucer-like depressions in the skin surface. This
type most commonly affects the upper arms and trunk. Patients with this
type of skin involvement may have either systemic disease or disease
limited to the skin.
Lupus discoid lesions in pictures
Pictures of Lupus profundus
Other lupus symptoms
Hair loss
Hair loss
Up to 1/3 of patients with systemic lupus erythematosus get reversible
form of hair loss associated with flares of their systemic disease. They
may also note, that their hair is more brittle than previously and
breaks easily giving rise to shortened hair (“lupus hair”). Another form
of reversible hair loss that leaves distinct bald spots, alopecia
areata, may also be more common in patients with lupus erythematosus.
Vasculitis
Patients with systemic lupus erythematosus may develop inflammation of
their blood vessels. This can result in varied manifestations running a
spectrum from multiple scattered red bumps, that may crust and ulcerate
to painful nodules.
 How is lupus diagnosed?
How is lupus diagnosed?
What causes lupus erythematosus?
The skin manifestations of lupus erythematosus are the result of inflammation in the skin that is primarily mediated by inflammatory cells called T lymphocytes. How and why these T cells are activated to cause disease is still unclear. Contributing factors include a genetic predisposition and environmental factors. Genetic factors - These genes encode proteins that are important in controlling the immune system and in fighting infection. Ultraviolet light is an environmental factor that can have an adverse effect both on skin lupus and systemic lupus erythematosus. It is thought that ultraviolet light can increase cell death in the skin and thereby boost the immune response to self. Ultraviolet light can also alter the responses of the immune system itself to antigens.
The skin manifestations of lupus erythematosus are the result of inflammation in the skin that is primarily mediated by inflammatory cells called T lymphocytes. How and why these T cells are activated to cause disease is still unclear. Contributing factors include a genetic predisposition and environmental factors. Genetic factors - These genes encode proteins that are important in controlling the immune system and in fighting infection. Ultraviolet light is an environmental factor that can have an adverse effect both on skin lupus and systemic lupus erythematosus. It is thought that ultraviolet light can increase cell death in the skin and thereby boost the immune response to self. Ultraviolet light can also alter the responses of the immune system itself to antigens.
 How is lupus diagnosed?
How is lupus diagnosed?
The specific skin forms of lupus erythematosus have a characteristic
appearance. To confirm the diagnosis, your doctor can perform a skin biopsy of the affected skin. Examination of a small sample of this skin
under the microscope can allow a more definite diagnosis as the
microscopic tissue changes are characteristic. In addition, a small
sample may be obtained for an immunofluorescence test. Also, Lupus
erythematosus is a condition in which there is antibody production to
self-tissues, and these may be detected in the skin with this test. 97% of those with lupus will also have a positive antinuclear antibody blood test (ANA). It’s very common to get somewhat different results at different labs.
However, if a person has active lupus, the ANA will likely be positive
at most laboratories most of the time. Fully healthy people should have an ANA level of zero. However, between 0:20 and 0:40 can still be considered a normal value by many immunologists. 0:40 is the starting value of a mild positive outcome and 0:80 is generally accepted as a positive test value. The figures double, so the next value is 0:160, then 0:320 and so on. Some people with severe autoimmune diseases can have NA levels that cross the 1000 mark. Other autoantibodies will also be
present in the bloodwork of a lupus patient. Usually, your doctor will first request a complete blood count
(CBC). Your blood is made up of red blood cells, white blood
cells, platelets and serum. The complete blood count measures the
levels of each. In cases of lupus, these blood tests may reveal low
numbers. (Source). Other blood tests can be ordered for Antibodies to double-stranded DNA (anti-dsDNA), Antibodies to histone, Antibodies to phospholipids (aPLs), Antibodies to Ro/SS-A and La/SS-B (Ro and La are the names of proteins in the cell nucleus), Antibodies to Sm and RNP. Here all these tests and their function are further explained. - I have an ANA of 1:80 these days, which is not high enough (nor specific enough) to suspect lupus according to my immunologist. Some advise from someone in one of my health groups:
"There is the ENA antigen group which you can google. Someone with lupus can be positive for the ssA and the ssB which can be related to Lupus or Sjogren's as well as four other antibodies.. if you had the inflammatory ones you probably had C reactive protein, Sed rate, ... there is DsDNA antibody, then there are your Complements 3 and 4... and all your Immunoglobulins., google all those.. Maybe you had some of those already.. it gives a pretty good picture of things but may not necessarily show a specific AID"
 The difference between rosacea and lupus
The difference between rosacea and lupusDiscoid lupus erythematosus can mimic many other skin diseases including psoriasis, fungal infection of the skin, and other rare inflammatory skin disorders. Or a common form of light sensitivity called polymorphous light eruption. In this condition, itchy bumps or welts may appear within minutes to hours after sun exposure. The malar rash of acute cutaneous lupus erythematosus can mimic rosacea. A rule of thumb might be that lupus lesions can appear all over the body, whereas rosacea is usually limited to the face (and sometimes neck or upper chest for a small percentage of people). Rosacea is also associated with facial flushing and lupus less so. Rosacea can also manifest itself in the eyes (ocular rosacea) and lupus won't. The same goes for p&p's (papulas or little red pimples), which do occur in rosacea and not in lupus. Corticosteroids work well for lupus usually, but often worsen rosacea, especially after discontinuation.
 The National Rosacea Society writes about the diagnosis between rosacea and lupus
The National Rosacea Society writes about the diagnosis between rosacea and lupus and makes an interesting observation about ANA levels in the blood of both lupus and rosacea patients (one of the diagnostic tools for lupus..): Link "Lupus erythematosus -- long known as an autoimmune disorder -- and rosacea share several signs and symptoms: facial redness, sensitivity to sunlight, and a tendency to affect women more than men. In fact, physicians have sometimes turned to blood tests to tell them apart. Now, researchers have discovered that those tests may not be as indicative as once thought. The blood tests look for elevated levels of antinuclear antibodies (ANAs), proteins produced by the immune system that target the nuclei of normal cells. Patients with lupus usually have high concentrations of ANAs in their blood, and this was thought by some to differentiate the disease from rosacea. However, a new study of 101 rosacea patients and 26 people with healthy skin, conducted by researchers in the Department of Dermatology at the Medical University of Lodz, Poland, found that 53.5 percent of the rosacea patients showed significantly increased levels of ANA in their blood, while only two of the control group with healthy skin had high levels of ANA. Patients with subtype 2 (papulopustular) rosacea were more likely to have significant ANA levels (32.7 percent of patients) than those with subtype 1 (erythematotelangiectatic) rosacea (16.8 percent of patients). After two years of follow-up, none of the patients with an elevated ANA developed an apparent autoimmune disorder. The researchers concluded that ANA blood tests should not be relied upon alone for differential diagnosis of lupus versus rosacea. However, ANA-positive patients may need additional studies as indicated by other findings, and should be followed over time."
 Posts on forums about this topic
Posts on forums about this topicBurnt1970 wrote on May 28th 2007: "This is what I'm dealing with right now. When my first derm diagnosed me with Rosacea 4 years ago, it was at first sight with no testing. My grandmother had Lupus pretty severely, and though I was tested for that 2 1/2 years ago (which came back negative), something else could be very much at work. The derm I saw a couple of weeks ago questions if I do have Rosacea since he was concerned about how sharply my redness cuts off. There are very defined borders on my neck. Also, my level of photosensitivity to fluoro lights concerned him (he watched me turn 20 shades of red right in front of his eyes). Another thing that's been happening over the past few months is red, blotchy rashes under my eyes. They have a bit of a sting and scaliness to them. IN FACT, just yesterday I laughed so hard about something that I cried. The result of the tears were nasty rashes appearing immediately under each eye, which is still somewhat there today. If this is autoimmune or allergy related, I've been eating aspirin like candy and taking antihistamines daily. I'm noticing some relief in color and other issues because of it."
Shantelle wrote on the Rosacea Forum about lupus: "Hi all. In regards to the above posts...Yes, Lupus is not as common in males as it is in females (Ratio Females 9:1 Males). Lupus can present itself in many different forms and symptoms (all inflammatory), often masquerading as other diseases or health issues. The butterfly rash is not seen in every Lupus patient, but if it does appear it can certainly masquerade itself as Rosacea (Type 1). Inflammatory hand and feet symptoms are common symptoms of lupus, particular if the person has systemic lupus or Raynaud's (Raynaud's is often seen in patients with autoimmune disease) or chronic cutaneous lupus affecting the hands or feet (lupus chilblains/ lupus pernio). If anyone thinks that they might have lupus, they should see their GP for a referral to a Rheumatologist (multiple inflammatory symptoms) or Dermatologist (symptoms all skin related). Lupus symptoms information:
http://www.dermnet.org.nz/immune/cutaneous-lupus.html
http://www.lupus.org/webmodules/weba...268&zoneid=526
http://www.hopkinslupus.org/lupus-info/"
Armabella wrote on July 18th 2013: "Hypothyroid and Rosacea or Lupus. Hi, my my wife has a hypothyroid condition which supposedly is caused by an autoimmune disorder. She started taking Levothyroxine when she was 23 but stopped for a while in her early thirties because she wanted to try something natural. After a year of taking the natural substitute, tests didn't look too good so she went back on the levothyroxine drug and this is when her Rosacea started. 3 years have gone by and in this time she saw two dermatologists who told her that her flare was Rosacea. Recently however, she went to a doctor who did some blood tests and is saying that her rosacea could be Lupus butterfly rash. We don't really trust this doctor because my wife doesn't have any other symptoms of lupus and her skin rash does look like rosacea, but we wanted to get opinions of other people in other parts of the world who might have experienced something similar. Is there anyone out there who has these two conditions (Rosacea/Hypothyroid) and does anyone know if there is a link between these two disorders or even between rosacea and lupus? Since they are both thought to be autoimmune diseases, could rosacea be lupus or a kind of lupus?"
Hugobb replied: "Hello armabella, I think that lupus rashes may vary from the classic 'butterfly shape'
and sometimes it can be very similar to rosacea. In addition, it is
known that some drugs can induce lupus-like symptoms. If you have any
doubt, you should seek a second opinion or maybe she wants to do a
biopsy. Remember that having a lupus rash doesn't necessarily mean
having systemic lupus. You should take a look at this article."
Jrlhamcat2 wrote on October 18th 2012: "I thought there might be some interest in this short report about four ANA-positive patients with a rosacea-like condition who were successfully treated with plaquenil. The full text is available here. Interestingly, the patients did not report having any flushing. I think this study probably reinforces the point that a red face is a fairly non-specific symptom with a variety of causes and treatments. They're saying an anti-malarial cleared up a rosacea-like rash in a small group of patients who were originally diagnosed with rosacea but after further testing actually (or additionally?) had a form of lupus."
Kimberly replied on October 31st 2012: "Anti-Ro/SSA antibodies were also found in all 4 patients." I've been tested for those, and I didn't have them. Just the ANA and anti-histone. Anti-Ro antibodies are linked to sjogrens and photosensitivity."
Jrlhamcat2 wrote on October 18th 2012: "I thought there might be some interest in this short report about four ANA-positive patients with a rosacea-like condition who were successfully treated with plaquenil. The full text is available here. Interestingly, the patients did not report having any flushing. I think this study probably reinforces the point that a red face is a fairly non-specific symptom with a variety of causes and treatments. They're saying an anti-malarial cleared up a rosacea-like rash in a small group of patients who were originally diagnosed with rosacea but after further testing actually (or additionally?) had a form of lupus."
Kimberly replied on October 31st 2012: "Anti-Ro/SSA antibodies were also found in all 4 patients." I've been tested for those, and I didn't have them. Just the ANA and anti-histone. Anti-Ro antibodies are linked to sjogrens and photosensitivity."
Most important information from this link:
"The
4 patients with rosacea-like cutaneous LE were 3 women and 1 man (F/M
ratio 3:1), with a mean age at disease onset of 54 years (range 41–69).
The mean duration of disease was 13 months (range 6–24). On admission to
our hospital, all 4 patients presented with erythema that was localized
to the central face and was associated with a few raised, smooth round
erythematous or erythematous-violaceous papules ranging from 2 to 3 mm
in diameter over the malar areas and forehead (Fig. 1a); the skin
lesions were accompanied by intense burning and, occasionally, by slight
to moderate pruritus. In all 4 cases the onset of the above cutaneous
picture had been sudden, and the patients had noticed aggravation of the
rash after sun exposure. Before our observation, all 4 patients had
been given treatments for rosacea in other institutions, including
tetracyclines, azithromycin or metronidazole orally, in combination
with topical metronidazole, with no benefit. The patients were not
treated for other concomitant diseases. After LE was diagnosed, we
evaluated the patients for systemic symptoms and signs associated with
LE, which were lacking in all 4 cases; moreover, none of them fulfilled
the American College of Rheumatology criteria for the diagnosis of
systemic LE (SLE) (13). The possible association with Sjögren’s syndrome
or other autoimmune disorders was excluded. The 4 patients were treated
with oral hydroxychloroquine 400 mg/daily, which induced a complete
clearing of the skin lesions (Fig. 1b) with a mean resolution time of 7
weeks (range 5–8 weeks). Hydroxychloroquine was discontinued 1 month
following complete resolution. The patients were warned against exposure
to sunlight and they were advised to apply total-block sunscreens in
bright sunlight. Currently, all patients are alive and free of disease,
with a mean time of follow-up of 4 years (range 2–7 years), with neither
relapses nor evolution into SLE.
Fig. 1. (a) Redness with small erythematous papules involving the central face in patient 1. (b) Complete resolution after hydroxychloroquine therapy. (c) Histology showing a pattern of lichenoid interface dermatitis (haematoxylin and eosin (H&E) stain; original magnification, × 100). (d) Medium-power view demonstrating the hydropic degeneration of the epidermal basal cell layer; in the dermis, a mixed inflammatory infiltrate associated with mucin deposition is evident (H&E stain; original magnification, × 200). The erythrocyte sedimentation rate was moderately elevated in only one patient (case 3) at disease onset (53 mm in the first hour; normal < 20), and reverted to normal after resolution. Antinuclear antibodies (ANA) were present, up to 1/640 with a fine speckled pattern, in all 4 cases. Anti-Ro/SSA antibodies were also found in all 4 patients. All the other immunological parameters evaluated, notably anti-double stranded-DNA antibodies, were normal or negative. Anti-Ro/SSA antibodies, re-evaluated in clinical remission at the time of writing this paper, remained positive in all 4 patients. The 4 patients demonstrated similar histological changes in biopsy specimens taken from facial papular lesions surrounded by erythema. These changes include epidermal atrophy, hydropic degeneration of the epidermal basal cell layer, and a superficial perivascular and periappendageal lymphohistiocytic infiltrate (Fig. 1c). Abundant dermal deposition of mucin was seen (Fig. 1d). In all 4 patients, direct immunofluorescence performed on biopsy specimens taken from lesional skin revealed granular deposits of immunoglobulin (Ig)M and IgG (case 3) or IgM alone (remaining cases) at the dermoepidermal junction; dermoepidermal granular deposition of C3 component of complement was also demonstrated in 2 patients (cases 1 and 4).
Although an erythematous eruption involving the face with sun exposure as triggering event is a classical cutaneous finding within the spectrum of LE, the presentation in our 4 cases is unique in that it resembled acne rosacea (12). However, the absence of pustules, telangiectasia, flushes and ocular signs, in addition to the lack of response to classical therapies for rosacea led us to test the patients for ANA and other autoantibodies, allowing us to diagnose LE. The 4 patients responded dramatically to hydroxychloroquine and there were neither relapses nor evolution into SLE after a mean follow-up of 4 years. The very rapid response to antimalarials may be explained by the fact that more superficial LE skin lesions, including erythema and papules, as in our patients, usually respond more rapidly than scaly, atrophic and scarring lesions. The absence of recurrence after treatment withdrawal may be due to the less aggressive nature of this atypical presentation of cutaneous LE. Anti-Ro/SSA antibodies, which are closely related to photosensitivity, are possibly the laboratory hallmark for this presentation, as for SCLE (7). However, our patients were unlikely to have SCLE due to the absence of typical annular or psoriasiform lesions. While classic discoid lupus was easily ruled on the basis of clinicopathological criteria, the tumidus variant should also be considered. However, the typical skin lesions in LE tumidus are erythematous, urticaria-like, non-scarring plaques, and its histology lacks changes of interface dermatitis as seen in our cases and typically shows a dermal infiltrate (3, 14). The strong mucin deposits found in our cases might suggest reticular erythematous mucinosis (REM) (15). Based on its possible association with autoimmune diseases, notably LE, the commonly observed photosensitivity, the deposition of IgM at the dermoepidermal junction found in some patients with REM and the good response to antimalarials, it has been classified among the specific cutaneous lesions of LE (14). However, similarly to lupus tumidus, REM is regarded as an example of dermal cutaneous LE and anti-Ro/SSA antibodies are usually lacking in this subset (15).
Systemic mastocytosis
Part of this information is based on my mastocytosis blog post.
Mastocytosis is a rare disease
characterized by an increase in mast cell number and activity in a
variety of tissues. Mast cells normally produce substances that
serve protective, inflammatory and regulatory functions in the body. In
mastocytosis, these substances are abnormally abundant, causing
various skin and systemic symptoms. Many of the substances produced by mast cells - including histamine - are potent dilators that can cause skin flushing. All the classic symptoms of rosacea such as facial redness, telangiectasia, flushing and papules can be mimicked by certain forms of mastocytosis. Physicians emphasize that it is common for bouts of flushing due to mastocytosis to trigger true rosacea in patients who are not genetically predisposed to the disorder.
What is histamine
Histamine is a chemical which your immune system makes. Histamines act like bouncers at a club. They help your body get rid of something that's bothering you -- in this case, an allergy trigger or "allergen." Histamines start the process that hustles those allergens out of your body or off your skin. They can make you sneeze, tear up, flush or itch - whatever it takes to get the job done. They are part of your body's defense system. When you have allergies, some of your triggers - such as pollen, pet dander, or dust - seem harmless. But your immune system sees them as a threat and responds. Your body's intention is good. But its overreaction gives you those all-too-familiar allergy symptoms, which you then try to stop with an antihistamine. Histamine also has some good (as in normal) functions: it takes part in the regulation of local blood circulation, in capillary permeability, contraction and relaxation of smooth muscles and blood vessels, secretion of hydrochloric acid in stomach, immediate hypersensitivity responses, allergic processes, inflammatory ones as part of the immune response to external pathogens, tissue healing, and its action has also been observed as neurotransmitter in the nervous system. Therefore it is also indispensable for the efficient functioning of many metabolic processes in the body. And histamine is also present in some foods: it depends on the food how high or low the histamine content is. Some foods naturally high in histamines include aged and fermented foods and alcohol (especially red wine). Some people may be sensitive to that. Hence, why some foods are more prone to cause an allergic reaction to people than others. If you eat foods high in histamine or have an allergy and are exposed to an allergen, this is what happens: First, it sends a chemical signal to "mast cells" in your skin, lungs, nose, mouth, gut, and blood. The message is: "Release histamines," which are stored in the mast cells. When they leave the mast cells, histamine boost blood flow in the area of your body the allergen affected (in our rosacea case it boosts blood flow to the skin of the face, making us more red, hot and even itchy). This causes inflammation, which lets other chemicals from your immune system step in to do repair work. Histamines then dock at special places called "receptors" in your body.
 Symptoms of Mastocytosis
Symptoms of Mastocytosis
Symptoms include skin flushing, itching, nausea, diarrhea, vomiting, headache, heart racing and breathing difficulties. Any physician such as your primary care physician or general practitioner can test for this disorder. Because mast cells play a role in allergic reactions, the symptoms of mastocytosis often are similar to the symptoms of an allergic reaction. Other possible symptoms are:
What is histamine
Histamine is a chemical which your immune system makes. Histamines act like bouncers at a club. They help your body get rid of something that's bothering you -- in this case, an allergy trigger or "allergen." Histamines start the process that hustles those allergens out of your body or off your skin. They can make you sneeze, tear up, flush or itch - whatever it takes to get the job done. They are part of your body's defense system. When you have allergies, some of your triggers - such as pollen, pet dander, or dust - seem harmless. But your immune system sees them as a threat and responds. Your body's intention is good. But its overreaction gives you those all-too-familiar allergy symptoms, which you then try to stop with an antihistamine. Histamine also has some good (as in normal) functions: it takes part in the regulation of local blood circulation, in capillary permeability, contraction and relaxation of smooth muscles and blood vessels, secretion of hydrochloric acid in stomach, immediate hypersensitivity responses, allergic processes, inflammatory ones as part of the immune response to external pathogens, tissue healing, and its action has also been observed as neurotransmitter in the nervous system. Therefore it is also indispensable for the efficient functioning of many metabolic processes in the body. And histamine is also present in some foods: it depends on the food how high or low the histamine content is. Some foods naturally high in histamines include aged and fermented foods and alcohol (especially red wine). Some people may be sensitive to that. Hence, why some foods are more prone to cause an allergic reaction to people than others. If you eat foods high in histamine or have an allergy and are exposed to an allergen, this is what happens: First, it sends a chemical signal to "mast cells" in your skin, lungs, nose, mouth, gut, and blood. The message is: "Release histamines," which are stored in the mast cells. When they leave the mast cells, histamine boost blood flow in the area of your body the allergen affected (in our rosacea case it boosts blood flow to the skin of the face, making us more red, hot and even itchy). This causes inflammation, which lets other chemicals from your immune system step in to do repair work. Histamines then dock at special places called "receptors" in your body.
 Symptoms of Mastocytosis
Symptoms of MastocytosisSymptoms include skin flushing, itching, nausea, diarrhea, vomiting, headache, heart racing and breathing difficulties. Any physician such as your primary care physician or general practitioner can test for this disorder. Because mast cells play a role in allergic reactions, the symptoms of mastocytosis often are similar to the symptoms of an allergic reaction. Other possible symptoms are:
- Fatigue
- Skin lesions (urticaria pigmentosa) and itching
- Abdominal discomfort
- Food and drug intolerance
- Infections (bronchitis, rhinitis, and conjunctivitis)
- Ear/nose/throat inflammation
- Anaphylaxis (shock from allergic or immune causes)
- Episodes of very low blood pressure (including shock) and faintness
- Bone or muscle pain
- Decreased bone density
- Headache
- Ocular discomfort
- Malabsorption
Diagnosing mastocytosis
Doctors can diagnose urticaria pigmentosa (cutaneous mastocytosis, see above) by seeing the characteristic lesions that are dark-brown and fixed. A small skin sample (biopsy) may help confirm the diagnosis. By taking a biopsy from a different organ, such as the bone marrow,
the doctor can diagnose systemic mastocytosis. Using special techniques
on a bone marrow sample, the doctor looks for an increase in mast
cells. Another sign of this disorder is high levels of certain mast-cell chemicals and proteins in a person's blood and sometimes in the urine, called Tryptase.
 How can Mastocytosis cause facial flushing?
How can Mastocytosis cause facial flushing?This article explains that mast cells are cells of the immune
system that are found around blood vessels in the skin, gastrointestinal
tract, respiratory tract and genitourinary tract. They contain several substances, of which histamine is the most common.
They are released upon contact with certain foreign
substances. In the most common form of mastocytosis, there are a greater
number of mast cells in the tissues. And therefore there is also too much histamine release. These mast cells cause a typical skin response in which hives immediately develop after stroking the skin with a blunt object. People with mastocytosis also experience symptoms throughout the body caused by the release of large amounts of histamine and other chemicals. The flushing occurs suddenly on the face and upper trunk. Many patients cannot identify a trigger that causes the flushing, but some identify exercise, heat, or emotional anxiety as a possible trigger. The red, hot face is often accompanied
by palpitations, low blood pressure, dizziness, chest pain, explosive
diarrhea, nausea or fatigue. Medications such as opioid narcotics like
morphine and codeine, and aspirin or other non-steroidal
anti-inflammatory drugs like ibuprofen or naproxen can also start a
flushing attack.
Pictures of Mastocytosis induced red skin
 (Source of the first picture. This woman writes a blog about her life with mastocytosis actually). The girl of the pictures on the right said about them: "The pictured episode was triggered by activity and allergens. It lasted about six or seven hours. MCAD (Mast Cell Activation Disease) flushing feels rather like a combination of sunburn and windburn, a sort of stinging sensation. I can feel a flushing episode before it becomes visible and also for a little while after it visibly fades. An episode can last a half hour or so for a very mild one to several days for a major one. During bad episodes, the reddened area is slightly swollen/raised." Here are more pictures of mastocytosis. This is the blog from the woman in the bottom left picture: Mastocytosis Musings. And this is the blog about mastocytosis flushing from the woman in the picture right from her.
(Source of the first picture. This woman writes a blog about her life with mastocytosis actually). The girl of the pictures on the right said about them: "The pictured episode was triggered by activity and allergens. It lasted about six or seven hours. MCAD (Mast Cell Activation Disease) flushing feels rather like a combination of sunburn and windburn, a sort of stinging sensation. I can feel a flushing episode before it becomes visible and also for a little while after it visibly fades. An episode can last a half hour or so for a very mild one to several days for a major one. During bad episodes, the reddened area is slightly swollen/raised." Here are more pictures of mastocytosis. This is the blog from the woman in the bottom left picture: Mastocytosis Musings. And this is the blog about mastocytosis flushing from the woman in the picture right from her. Treatment of mastocytosis
Treatment of mastocytosisThe treatment of mastocytosis is mainly symptomatic. Patients should avoid known histamine-degranulating agents. Patients can take antihistamine medication. Usually doctors chose a combination treatment with an H1 antihistamine (hydroxyzine 10-20 mg for instance) and H2 antihistamine (cimetidine 200-500 mg for instance). Oral administration of the mast cell stabilizing agent disodium cromoglycate has proved effective in some patients. Photochemotherapy has been reported to cause symptomatic relief as well as objective reduction in the population of mast cells and the urinary excretion of MIAA.
Other histamine-related conditions that cause flushing; mast cell issues
It is also possible that someone who flushes a lot does not in fact have mastocytosis (or anything other than rosacea and faulty functioning blood vessels), but instead Mast cell activation Syndrome. Mastocytosis causes too many mast cells in your body, but Mast cell activation Syndrome does not create statistically more mast cells in the body, but instead makes the normal number of mast cells malfunction, being hyper-reactive and causing symptoms such as flushing, hives, burning feeling, easy bruising, itchiness, lightheadedness/ dizziness, diarrhea, headaches, pain and redness of the eyes and brain fog. To name a few symptoms (check the rest of the possible symptoms out here). This is what my doctor thinks I have. My tryptase blood test came back negative, so I don't have mastocytosis. But he does suspect a histamine component to my flushing, as I flush (violently) from foods high in histamine, from pollen, from perfume and many other triggers that can be linked to histamine release in the body - which then in turn dilates the blood vessels. I also get persistent cold urticaria every winter and heat rash every summer. I am currently trying medication aimed to control Mast cell activation Syndrome: Montelukast (Singulair), ranitidine and Xyzal. Photos of my own cold urticaria in winter and heat rash in summer (showing the difference in skin within hours after being exposed to heat for extended time - those rashes in the 4th picture also were all gone again after several hours):
 DAO deficiency
DAO deficiency
DAO deficiency means there is not enough of the specific digestive enzyme present in the body, which is responsible for breaking off the histamine that is in food. Diamine oxidase enzyme or DAO is located in the intestinal mucosa mainly, and starts working during the digestion of food. When there is an alteration in the metabolism of histamine and there is not enough DAO activity, the imbalance between ingested histamine and histamine released from the storage cells leads to histamine accumulation in the blood, which causes health symptoms such as flushing, sneezing and itching, but also possibly: migraine, headaches and/or dizziness. Irritable Bowel Syndrome (diarrhea, constipation), Crohn disease, stomach pain, nausea and/or vomiting. Hypotension, hypertension and/or arrhythmia. Hives, oedema, atopic skin, eczema and/or rach. Nose congestion, rhinitis, asthma and/or sneezing. Muscle pain, fibromyalgia and/or fatigue. Bone pain. It has been observed that most patients with low functional DAO activity present other related symptoms, especially migraine. 20% of patients experience 1 or 2 of these associated symptoms, 41.3% of patients experience 3 or 4 of these symptoms and 33.8% present more than 5. Migraine is always the most highlighted syndrome when interviewing the patients due to its disabling character. With DAO deficiency, unlike with a food allergy, the occurrence of symptoms or adverse effects is not linked to the intake of specific food; by contrast it can be related to a wide variety of food with different histamine contents (even to foods with low histamine levels). A special blood test can detect the DAO enzymatic deficiency. Once confirmed, the treatment consists in a diet low in histamine and other amines that enhance its accumulation.
Y-gwair wrote: Quote Originally Posted by lilyian. "If you did actually have a mast cell problem, it is easily controlled with prescription histamine blockers. Best thing to do is to get checked out my an allergist. People with these illnesses don't really have allergies, but the source of the problem is still mast cells which are what cause allergy problems." This is not true, H1/H2s will only control SOME symptoms caused by release of histamine (like itching), but mast cells actually produce about 60 different vasoactive substances which antihistamines have no effect on. It's true that mast cell activation is not a true allergy, but there are still many allergy doctors that don't understand this and only test the limited parts of the immune system that they know about. Also many don't understand the difference between mastocytosis (which is where your bone marrow produces increased number of genetically altered mast cells) and mast cell activation (where you have a normal number of mast cells which have become abnormally over-reactive). The kind of doctor you need to see with these disorders is an immunologist specializing in allergic disease. Ideally, they will test tryptase (which is a substance that stimulates the production of extra mast cells in mastocytosis), Diamine Oxidase, which is an enzyme that breaks down histamine, histamine levels in urine/blood. They also look to see if you vitamin D levels are low, as this is also a marker for high circulating histamine. (Scarletnat: oh boy, my vitamin D levels are very very low, despite sun tanning my body everyday for an hour at mid day if possible, never understood why levels stayed so low..). If you are in the US, they will also test for prostaglandin D2 and leukotrines. They should also do a very detailed investigation of your immune system, breakdown of all immunoglobulins, rheumatological markers and many other relevant things. After quite a few misdiagnoses, I've finally found the true reason for my flushing, which is deficiency in Diamine oxidase, linked to mast cell activation causing high levels of unknown vasodilatory and neurological irritant substances. If I'd listened to my idiot dermatologist, I'd still be mucking around with clonidine and beta blockers, both of which were making my condition worse. Doxepin is a tricyclic, which are a group of medications that cause mast cell degranulation, along with many, many other common medications including virtually all painkillers except paracetamol."
Y-gwair wrote: Quote Originally Posted by lilyian. "If you did actually have a mast cell problem, it is easily controlled with prescription histamine blockers. Best thing to do is to get checked out my an allergist. People with these illnesses don't really have allergies, but the source of the problem is still mast cells which are what cause allergy problems." This is not true, H1/H2s will only control SOME symptoms caused by release of histamine (like itching), but mast cells actually produce about 60 different vasoactive substances which antihistamines have no effect on. It's true that mast cell activation is not a true allergy, but there are still many allergy doctors that don't understand this and only test the limited parts of the immune system that they know about. Also many don't understand the difference between mastocytosis (which is where your bone marrow produces increased number of genetically altered mast cells) and mast cell activation (where you have a normal number of mast cells which have become abnormally over-reactive). The kind of doctor you need to see with these disorders is an immunologist specializing in allergic disease. Ideally, they will test tryptase (which is a substance that stimulates the production of extra mast cells in mastocytosis), Diamine Oxidase, which is an enzyme that breaks down histamine, histamine levels in urine/blood. They also look to see if you vitamin D levels are low, as this is also a marker for high circulating histamine. (Scarletnat: oh boy, my vitamin D levels are very very low, despite sun tanning my body everyday for an hour at mid day if possible, never understood why levels stayed so low..). If you are in the US, they will also test for prostaglandin D2 and leukotrines. They should also do a very detailed investigation of your immune system, breakdown of all immunoglobulins, rheumatological markers and many other relevant things. After quite a few misdiagnoses, I've finally found the true reason for my flushing, which is deficiency in Diamine oxidase, linked to mast cell activation causing high levels of unknown vasodilatory and neurological irritant substances. If I'd listened to my idiot dermatologist, I'd still be mucking around with clonidine and beta blockers, both of which were making my condition worse. Doxepin is a tricyclic, which are a group of medications that cause mast cell degranulation, along with many, many other common medications including virtually all painkillers except paracetamol."
 Differences between mastocytosis and rosacea
Differences between mastocytosis and rosaceaPeople with mastocytosis often not only flush in their faces, but also on their chest and neck. They experience general hot flash symptoms and feelings. Whereas many rosacea patients just feel their face burn and the rest of their bodies can feel cold at the same time. People with mastocytosis also often have addition symptoms, like sneezing and allergy-related symptoms, unlike most people with rosacea. For people with mastocytosis, episodic bright red flushing can occur spontaneously, after rubbing the skin or after exposure to alcohol or mast cell degranulating agents. Flushing attacks may be accompanied by headache, dyspnea and wheezing, palpitations, abdominal pain, diarrhea and syncope and may closely resemble the flushing episodes of the carcinoid syndrome, especially the foregut variety which are also mediated by histamine. Rosacea may develop rarely. The flushing of cutaneous mastocytosis typically lasts more than 30 minutes. In urticaria pigmentosa, the diagnosis is established by demonstrating that gentle rubbing of the lesional skin causes local itching, redness, and whealing (Darier’s sign). This reaction is caused by local histamine release. Darier’s sign may also be demonstrated in skin without lesions.
 This is a very interesting article about the differentiation between rosacea flushing and Mastocytosis flushing, characterized by either sweating flushes or dry flushes.
This is a very interesting article about the differentiation between rosacea flushing and Mastocytosis flushing, characterized by either sweating flushes or dry flushes.
In it, the author states about flushers who also sweat during a flushing attack, that their flushing tends to be a cholinergic nerve discharge and more typical of mast cell disease. "Why does it matter whether or not you sweat when you flush? Why is that so important in trying to distinguish between mast cell-related flushing and other causes of flushing?" There are many different substances, the author continues, that can cause flushing, and which ones are at work is related to the specific cause of the flushing. In Table 1 (see below), the specific mediators of flushing due to various causes are listed. It should be noted that “With the exception of carcinoids, flushing due to tumors is rare and tends to occur in advanced stages.” So, while there are very benign causes of flushing, such as changes in temperature, emotional state, or exertion, as well as eating spicy food, flushing can also be a symptom of a serious physical condition.
The sympathetic nervous systems' neurons release acetylcholine,
which causes both sweat gland activity and dilation of blood vessels. So, when you see someone both sweating and “turning red,” you are probably witnessing flushing that is due the cholinergic effects of the sympathetic nervous system. In contrast, when histamine is released by mast cells in the skin, it has the effect of dilating blood vessels, but the histamine does not have an effect on the sweat glands. So when we see flushing without sweating, it’s more likely to be caused by histamine release in the skin. There’s only one caveat to this explanation: When a person is going into shock, they will often begin sweating profusely and anaphylaxis can send someone into shock. So, sweating in the later stages of a mast cell crisis is to be expected — it’s only in the early stages that we expect flushing without sweating." - One of the recurrent topics on the rosacea forum is how a lot of rosaceans there don't seem to sweat much. Me included. It's interesting to finally read about the sweat factor in flushing. It could indicate that in my specific type of vascular rosacea symptoms, the biggest trigger is not the sympathetic nervous system, as I always assumed, but histamine release.
Table 1. The mediators of flushing
| Condition | Specific mediators |
|---|---|
| Foods, beverages, alcohol | Tyramine (present in ergot, mistletoe, ripe cheese, beer, red wine, and putrefied animal matter), histamine, sulfites, nitrites, alcohol, aldehyde, higher chain alcohols, monosodium glutamate (MSG), capsaicin (which is what makes chili peppers hot), and cigua toxin (fish) |
| Menopause | Estrogen fluctuations |
| Mastocytosis, anaphylaxis, and mast cell-related disorders | Histamine, prostaglandin D2, leukotrienes, tumor necrosis factor α (alpha), vascular endothelial growth factor, interleukins, heparin, and acid hydrolases |
| Carcinoid syndrome (symptoms and lesions produced by the release of serotonin from carcinoid tumors of the GI tract that have metastasized to the liver) | 5-hydroxytryptamine (5-HT; no flushing but diarrhea), substance P, histamine, catecholamines, prostaglandins, kallikrein, kinins, tachykinins, neurotensin, neuropeptide K, vasoactive intestinal polypeptide (VIP), gastrin-related peptide, and motilin |
| Pheochromocytoma (a usually benign neoplasm in the adrenal gland’s medullary tissue) | Catecholamines (epinephrine, norepinephrine, dopamine), vasoactive intestinal polypeptide (VIP), calcitonin-gene-related peptide, and adrenomedullin |
| Medullary carcinoma of the thyroid | Calcitonin, prostaglandins, histamine, substance P, levodopa, ketacalcin, adrenocorticotropic hormone, and corticotropin-releasing hormone |
| Pancreatic cell carcinoma | Vasoactive intestinal polypeptide (VIP), prostaglandin, and gastric inhibitory polypeptide |
| Renal cell carcinoma | Prostaglandins and pituitary down-regulation |
| Neurologic | Substance P and catecholamines |
Queta wrote on October 30th 2009: "It was Histamine Intolerance All along.. Just want to update people on my progress because it may help someone else. I have struggled with rosacea for years and years, since I was at least 12 years old. I have flushing, bloodshot eyes, swelling of my eyelids, nose, chin and forehead. Then someone on this site talked about something called Histamine Intolerance. I looked it up and thought I would try a new supplement (and very expensive, unfortunately) called Histame which is supposed to help those who have trouble eating histamine rich foods. Well, guess what? My skin is not only clear but much, much less puffy. My eyes are not bloodshot but white. I look so much healthier. For me, it was Histamine Intolerance all along. That is probably why my skin and my diet were so interrelated, and why taking a mast cell inhibitor like quercetin helped me. Anyway, I am now one happy camper. I still stick to a low histamine diet, which most docs who treat Histamine Intolerance seem to recommend, but my face looks great. My whole appearance has improved. If you seem to react to high histamine foods (tomatoes, smoked fish, aged cheese, etc.) you might want to give it a whirl. Histame is very expensive, though, but I don't have much choice for myself. My body really seems to be lacking in DAO, one of the enzymes that helps the body deal with histamine. Regards Queta "
Queta had earlier written on May 16th 2009: "Hi, Just want to put in a plug for quercetin/bromelain supplementation. I kid you not, my rosacea is 95% gone now. I have been on this combo for a few months now. Quercetin is known to inhibit mast cells, which appear to play a role in rosacea. I take 2 capsules of quercetin/bromelain before each meal and my snack (so 4 times per day) and my rosacea is definitely getting better all the time. The day before yesterday I did the dreaded smile test where I smile in the car vanity mirror. Normally my face looks weird when I smile-my cheeks puff out too far and it looks like I have too much fluid in my face or something. The other day I did it and guess what? I looked almost completely normal. Just wanted to share...if anyone out there thinks that supplements don't work I have to say I was in your camp but tried this out of frustration and fear of getting worse and worse. The visible veins on the end of my nose are almost gone now, too. It's been really amazing. I do still have to watch my diet, but this combo has taken my rosacea to a whole new level. Feel free to respond with any comments or questions. Cheers and all good things, Queta "
Lilyian wrote on January 21st 2008: "J, You are right on target with mastocytosis. However, the skin version is called urticaria pigmentosa. That consists of brown/reddish spots that appear on the skin always in the same places. Now, some people with that will have systemic symptoms, such as diarrhea, itching everywhere, burning feelings everywhere, flush, hives, throat tightening, difficulty breathing, anaphylactic shock and more. All masto patients have symptoms unique to themselves. So, one might just have red brown spots while another might have no spots, just itchy bumps on face and yet have the severe GI distress.There is another disease exactly like masto, called Idiopathic Anaphylaxis (IA) (some docs call is Mast Cell Activation Disorder - MCAD). The symptoms triggers and medications for both diseases are exactly the same. The difference is the cause. Masto is caused by having too many mast cells or having mutated ones. IA is when the mast cells are completely normal, but way too sensitive. When triggered, the mast cells degranulate (release histamines -- like when the person who is deathly allergic to bees gets stung by a bee). So, the patient starts experiencing allergy type symptoms, even though he might test negative to all allergies. I have IA (Idiopathic Anaphylaxis), although my doc (one of the most renowned mast cell researchers) really thought I had systemic masto (skin plus body symptoms). The only way to diagnose systemic masto is through a bone marrow biopsy, which I eventually had done. I tested negative, so I get labeled as having IA. It is tricky for me to know if my flushing was rosacea or my IA. I think it was 90% my IA and 10% rosacea perhaps. My histamine blocker meds were like magic. I never thought they would work, so you can imagine my surprise when I took them and saw that all my flushing disappeared! Not I only flush if my symptoms start to trigger; it is a warning sign to me if my face flushes and gets hot. I take 180 mg Allegra in the morning and 10 mg zyrtec in the early evening (among other histamine blocker meds) every day. Flushing can certainly point to IA or masto. The problem is that most docs don't know how to identify the diseases or diagnose it. Even if they think that they can diagnose it, they are usually wrong. There are only a handful of masto researchers in the country, and they are scattered at the main facilities, such as Univ Of Michigan, Mayo, and NIH. I absolutely cannot recall if you can diagnose UP by a skin biopsy; you cannot diagnose systemic masto that way. Does this help you figure out anything? Please feel free to as me more questions is it will help."
Hoselio wrote on December 7th 2013: "I went to my family doctor for my usual flushing problems (contact flushing, flushing from exertion, heat, ect.) and told him some of my other symptoms (clogged runny nose when I eat, bright red itchy feet when I get out of the shower or stand up sometimes, heart palpitations, can't breathe properly through my nose, can only breathe properly by taking short quick breaths, and mild dermographia) and he told me that he thinks that I might have mastocytosis. I asked him if he could put me on Remeron since I also have severe depression & anxiety due a lot of bad things piling up on me lately, and he said that he wants to try a less potentially harmful antidepressant along with a mast cell inhibitor and antihistamine. So I ended up getting a prescription for Prozac, Cromolyn Sodium (oral) and Allegra."
Jrlhamcat2 replied: "I don't have experience with ketotifen or other mast cell inhibitors but would suggest making sure you've given the cromolyn sodium and Allegra a good long trial at a high dosage first, if you haven't already. I'm currently taking them and seeing a huge improvement, even though it's the worst time of the year for my skin. It does take up to a couple months and a rather large dosage, though. I'm currently on: Nalcrom (trade name for cromolyn sodium/sodium cromoglicate): 200mg 4x/day. Fexofenadine (generic Allegra): 120mg 2x/day. Both of these have had absolutely no adverse effects for me as far as I can tell over the two months I've been taking them, unlikely everything else I've tried. Ketotifen and Montelukast can help but can have some unpleasant effects, so it's worth ensuring that something safer won't work first. It might be worth talking more with someone who specialises in allergy & immunology and mast cell disorders, specifically since ruling out systemic disorders with these symptoms seems to require a long list of tests, and even smart and helpful GPs can't be familiar with all of it in my experience. Did your GP test serum tryptase levels since he suspects mastocytosis? As you probably know, some of what you described sounds like POTS, which is linked to various autoimmune, mast cell, and connective tissue disorders. A good immunologist might be able to give you most of the tests you need and suggest the right kind of specialist if any further testing would be useful."
Menopausal flushing
 About 80% of postmenopausal women experience flushing associated with
sweating. A similar syndrome may also occur in men with prostate cancer
receiving treatment with gonadotropin-releasing hormone analogues, such
as buserelin. About 65% of postmenopausal women have hot flushes for 1
to 5 years, 26% for 6 to 10 years, and 10% for more than 11 years. source link
About 80% of postmenopausal women experience flushing associated with
sweating. A similar syndrome may also occur in men with prostate cancer
receiving treatment with gonadotropin-releasing hormone analogues, such
as buserelin. About 65% of postmenopausal women have hot flushes for 1
to 5 years, 26% for 6 to 10 years, and 10% for more than 11 years. source linkSigns and symptoms
There is considerable variation in the frequency, intensity and duration of hot flashes among individuals. A typical hot flush begins with a sensation of warmth or heat in the head and face, followed by facial flushing that may radiate down the neck and to other parts of the body. It is associated with an increase in temperature and pulse rate and followed by a decline in temperature and then by sweating. Visible skin changes occur in about 50% of women. Each hot flush may last for 1 to 30 minutes (but lasts 4 minutes on average, although the numbers differ per online source). Wiki states: "Hot flashes, a common symptom of menopause and perimenopause, are typically experienced as a feeling of intense heat with sweating and rapid heartbeat and may typically last from two to thirty minutes for each occurrence, ending just as rapidly as they began. The sensation of heat usually begins in the face or chest, although it may appear elsewhere such as the back of the neck, and it can spread throughout the whole body. Some women feel as if they are going to faint. In addition to being an internal sensation, the surface of the skin, especially on the face, becomes hot to the touch. This is the origin of the alternative term "hot flush", since the sensation of heat is often accompanied by visible."
Excessive flushing can lead to rosacea
Other symptoms are drenching perspiration, a sensation of overheating before the onset of flushing and sweating, and waking episodes at night with the typical symptoms. Alcohol can enhance a menopausal flush. It is not yet entirely clear what causes hot flashes. The hot flash event may be repeated a few times each week or every few minutes throughout the day. Hot flashes may begin to appear several years before menopause starts and last for years afterwards. Some women undergoing menopause never have hot flashes. Others have mild or infrequent flashes. The worst sufferers experience dozens of hot flashes each day. In addition, hot flashes are often more frequent and more intense during hot weather or in an overheated room, as the surrounding heat apparently making the hot flashes themselves both more likely to occur, and more severe.
 Causes of menopausal flushing
Causes of menopausal flushingThere are indications that reduced levels of estrogen are to blame and are the primary cause of hot flashes. Rapid estrogen withdrawal is more likely to cause hot flashes than a low estrogen level by itself. Hot flashes may also be due to a change in the hypothalamus' control of temperature regulation. And another source blames very high levels of gonadotropins as the ovaries fail.
Young women
If hot flashes occur in a young woman's menstrual cycle, it might be a symptom of a problem with her pituitary gland; seeing a doctor is highly recommended. In younger women who are surgically menopausal, hot flashes are generally more intense than in older women, and they may last until natural age at menopause.
Men
Hot flashes in men can have various causes. One is a possible sign of low testosterone. Another is andropause, or "male menopause". Men with prostate cancer or testicular cancer can also have hot flashes, especially those who are undergoing hormone therapy with antiandrogens, also known as androgen antagonists, which reduce testosterone to castrate levels.There are also other ailments and even dietary changes which can cause it. Men who are castrated can also get hot flashes.
Treatment options for menopausal hot flashes
Treatment options include hormone replacement therapy, selective estrogen receptor modulators, selective serotonin reuptake inhibitors (SSRI's), mirtazapine, isoflavones, the use of natural phytoestrogens (like ginseng and flaxseed). Also used are progestogen, eg norethisterone or megestrol, and the anticonvulsant gabapentin. Examples of useful SSRI's are paroxetine (20 mg daily), fluoxetine (20 mg daily), citalopram (20 mg daily). Veralipride, an antidopaminergic drug, can cause reductions in the frequency and intensity of menopausal flushing in premenopausal women pretreated with goserelin (a gonadotropin-releasing hormone agonist) for endometriosis. Neurotransmitters that may be involved in the pathogenesis of hot flushes include norepinephrine and other noradrenergic substances. The central noradrenergic system in the hypothalamus triggers the hot flushes via α2-adrenergic receptors on the noradrenergic neurons. Thus, clonidine, an α2-adrenergic agonist, effectively alleviates hot flushes through reduction of noradrenergic release.
The differences between menopausal hot flashes and rosacea
Treatment options include hormone replacement therapy, selective estrogen receptor modulators, selective serotonin reuptake inhibitors (SSRI's), mirtazapine, isoflavones, the use of natural phytoestrogens (like ginseng and flaxseed). Also used are progestogen, eg norethisterone or megestrol, and the anticonvulsant gabapentin. Examples of useful SSRI's are paroxetine (20 mg daily), fluoxetine (20 mg daily), citalopram (20 mg daily). Veralipride, an antidopaminergic drug, can cause reductions in the frequency and intensity of menopausal flushing in premenopausal women pretreated with goserelin (a gonadotropin-releasing hormone agonist) for endometriosis. Neurotransmitters that may be involved in the pathogenesis of hot flushes include norepinephrine and other noradrenergic substances. The central noradrenergic system in the hypothalamus triggers the hot flushes via α2-adrenergic receptors on the noradrenergic neurons. Thus, clonidine, an α2-adrenergic agonist, effectively alleviates hot flushes through reduction of noradrenergic release.
The differences between menopausal hot flashes and rosacea
Hot
flashes tend to last shorter than a typical rosacea flare (often only
minutes whereas a rosacea flush can take a lot longer to build up and
calm down again). Rosacea, unlike menopausal hot flashes, is usually not
associated with sweating and a rapid pulse. Neither does it typically
spread further than the face. The hot flashes sometimes associated with
menopause may bring on a flare-up or even the initial onset of rosacea. A
Swedish study also noted that postmenopausal women with rosacea may be
more likely to experience migraine headaches.
This kind of vascular dilation is caused by an adrenaline rush. Adrenaline facial skin flushing is the same as systemic flushing, but it is hormone released. Stress is the body's reaction to a perceived threat. Adrenaline and hormones are then released and the nervous system is activated, sharpening our senses, but simultaneously our pulse rises, muscles tense and our immune system begins to shut down. Adrenaline activity can also cause acne in both men and women as a reaction to mental or physical stress. In women, half of their testosterone is produced by the ovaries with the other half being produced by the adrenal glands. Estrogen smoothes out the testosterone produced by the ovaries, but when the estrogen level drops several days before the menstrual periods, sometimes acne can pop up. Especially when the adrenal glands overproduce due to stress or fatigue. The adrenal glands can also be stressed continually in both men and women, resulting in too much testosterone and overstimulation of the sebaceous glands. Similarly, in the male an overabundance of testicular testosterone especially with overstimulated adrenal glands, can cause the overstimulation of sebaceous glands. Getting enough sleep and finding ways to relax will naturally help relieve stress and reduce the adrenaline reaction that follows. Beta blockers block the release of the stress hormones adrenaline and noradrenaline. (Source)
Forum posts about menopausal hot flashes
Irishgenes wrote on January 28th 2006: "This is my first post this year, as I have been cured of rosacea by finding the right amount of estrogen for my body. Although Climara is a bioidentical form of estrogen, the patch form was never enough for me, and I continued to suffer even wearing two patches at a time. The patch also does not last the length of time that they claim. These standard doses are just not good for most women, and that is why the majority of women discontinue hormone replacement therapy. I used compounded Tri-Est capsules for years, but lately I have discovered compounded estrogen skin gel. With the gel, I can modify the dose from time to time as needed. The gel is made up in gm doses, which is 1/4 tsp. I have bought a set of measuring spoons called "dash, pinch, and smidgen" which measures 1/8, 1/16, and 1/32 tsp. Thus, I can adjust the dose on days when I need a little extra or feel like I have too much (easily recognized by bloat and breast pain). These are all the symptoms I have had which have been cured by the right dose of bioidentical estrogen: heart palpitations, flushing, fever of 2 degrees at times, chest pain, gastroesophageal reflux, arm & leg cramps, severe migraine headaches, hunger pains & weight gain, high blood pressure, depression, irritability, urinary urgency, forgetfulness, dry eyes, diarrhea, and ROSACEA! Yes, there are estrogen receptors in every body system. As soon as my estrogen dips too low, I get (among other things) red, swollen, dry, scaley, & itchy eyes and lids. As soon as my dose is absorbed, it all goes away like magic. I have ceased all expensive supplements and all drugs, and I have had no rosacea for about a month now. I eat whatever I want, including former "trigger" foods (and SUGAR, Brady!) I can go in the sun without fear. I will report back in the summer to tell you if I have stayed rosacea-free.
Irishgenes wrote on January 28th 2006: "This is my first post this year, as I have been cured of rosacea by finding the right amount of estrogen for my body. Although Climara is a bioidentical form of estrogen, the patch form was never enough for me, and I continued to suffer even wearing two patches at a time. The patch also does not last the length of time that they claim. These standard doses are just not good for most women, and that is why the majority of women discontinue hormone replacement therapy. I used compounded Tri-Est capsules for years, but lately I have discovered compounded estrogen skin gel. With the gel, I can modify the dose from time to time as needed. The gel is made up in gm doses, which is 1/4 tsp. I have bought a set of measuring spoons called "dash, pinch, and smidgen" which measures 1/8, 1/16, and 1/32 tsp. Thus, I can adjust the dose on days when I need a little extra or feel like I have too much (easily recognized by bloat and breast pain). These are all the symptoms I have had which have been cured by the right dose of bioidentical estrogen: heart palpitations, flushing, fever of 2 degrees at times, chest pain, gastroesophageal reflux, arm & leg cramps, severe migraine headaches, hunger pains & weight gain, high blood pressure, depression, irritability, urinary urgency, forgetfulness, dry eyes, diarrhea, and ROSACEA! Yes, there are estrogen receptors in every body system. As soon as my estrogen dips too low, I get (among other things) red, swollen, dry, scaley, & itchy eyes and lids. As soon as my dose is absorbed, it all goes away like magic. I have ceased all expensive supplements and all drugs, and I have had no rosacea for about a month now. I eat whatever I want, including former "trigger" foods (and SUGAR, Brady!) I can go in the sun without fear. I will report back in the summer to tell you if I have stayed rosacea-free.
It seems like I must have had every menopausal symptom there is, but other women have symptoms like fibromyalgia, carpal tunnel, and chronic fatigue which may be related to estrogen deficiency. For those who are perimenopausal, there is no need to suffer for 15 years or more until you reach menopause. Your estrogen levels start declining in your 30's, and just because your doctor tested your estradiol on one day does not mean it did not dip down too low the next day. For practical advice on how to use bioidentical estrogen for various symptoms from your 30's on up, I strongly recommend the wonderful book, "Natural Hormone Balance for Women" by Dr. Uzzi Reiss. He gets into the nitty-gritty of EXACTLY what to do and how to do it, so that you will become an expert at dosing yourself. Of course, you will still have to find a doctor who will prescribe it for you, but with the gel, you won't be stuck with a standardized dose. If you are perimenopausal and have symptoms on just a few days a month, you can use just a little gel on those days. Dr. Reiss doesn't discuss rosacea in the book, but then who knew that rosacea could be caused by estrogen deficiency? I started getting the eyelid symptoms in my late 30's (along with the migraines), but thought I had an allergy. As for the migraines, I hate to think of all the hours of pain and vomiting-- the codeine, Imitrex shots & then pills, and trips to the ER for Toradol shots. Now when I get the first inkling of a migraine, I rub on a smidgen of estrogen gel and it is gone. No more pain pills for me! The gel takes about an hour to absorb, but Dr. Reiss mentions sublingual estrogen drops for migraines that work even quicker, and I plan to get a prescription for those soon. For those women who have rosacea in your 20's, I would suggest finding a different birth control pill if you are currently on the pill or maybe going off the pill to see if it helps. (See Dr. Vliet's book for a list of the best bc pills, which are those with a high estrogen to progestin ratio.) For those women who got rosacea in childhood, estrogen deficiency now may be making your rosacea worse, but you obviously won't be cured by estrogen. For guys (if you've read this far), don't try this at home! "
 Ruthuk wrote on January 3rd 2012: "Hello, I was diagnosed with premature ovarian failure (early menopause) in May. I've been struggling badly with hot flushes, despite being on an increasingly high dose of HRT. More recently I've noticed that my face is almost permanently red. In real life I was the palest person you could imagine, although not troubled by blushing. Now my skin looks suspiciously healthy most of the time and if I get hot (by which I mean any temperature above really freezing), do any sort of light exercise, have a glass of wine, I go bright red on my nose, and pretty red on my cheeks, rest of face, neck and upper chest. It seems to get worse over the course of the day too. But it is not a "normal" hot flush in that it just doesn't go away ... I am therefore wondering about rosacea. I believe that menopause often triggers rosacea, or perhaps my versions of hot flushes are just not the normal ones? My main problem, because I can live with the redness (and it's not the searing red I've seen in bad rosacea cases just very pink, like after you get out of a hot bath), is that I am UNBELIEVABLY HOT. It's making my life a misery. Rosacea or just menopause? It's weird that the HRT isn't taking the heat away, which is why I'm thinking I must have something else ...I'd be very grateful for any info."
Ruthuk wrote on January 3rd 2012: "Hello, I was diagnosed with premature ovarian failure (early menopause) in May. I've been struggling badly with hot flushes, despite being on an increasingly high dose of HRT. More recently I've noticed that my face is almost permanently red. In real life I was the palest person you could imagine, although not troubled by blushing. Now my skin looks suspiciously healthy most of the time and if I get hot (by which I mean any temperature above really freezing), do any sort of light exercise, have a glass of wine, I go bright red on my nose, and pretty red on my cheeks, rest of face, neck and upper chest. It seems to get worse over the course of the day too. But it is not a "normal" hot flush in that it just doesn't go away ... I am therefore wondering about rosacea. I believe that menopause often triggers rosacea, or perhaps my versions of hot flushes are just not the normal ones? My main problem, because I can live with the redness (and it's not the searing red I've seen in bad rosacea cases just very pink, like after you get out of a hot bath), is that I am UNBELIEVABLY HOT. It's making my life a misery. Rosacea or just menopause? It's weird that the HRT isn't taking the heat away, which is why I'm thinking I must have something else ...I'd be very grateful for any info."
Judworth replied: "Hello Ruthuk, Do you get any sensitivity or pain with the flushing? I am approaching menopause & find that the 'hot flushes' that I get with menopause is a very different feeling to a rosacea flush/heat. I am taking beta blockers for rosacea & it appears to be helping confine my hot flushes to my body! Judy"
And Judworth wrote on May 2nd 2014: "Hello Wendy, I do hope that you don't mind me replying. I am 56 next month (sadly still perimenopausal) but my rosacea HAS got better over the years. It started when I was 44 and I would get hourly flushing............ now although I flush, get P&P's, the real attacks are maybe 2-5 times a month (I know as I keep a rosacea diary!). The longer the months between periods are, I find things are so much better, it's only the build up to yet another one that will cause me pain. I hope that gives you some hope for the future? Hugs Judy"
Flushing is a side effect of sildenafil citrate in 12% of patients. Systemic administration of morphine can cause flushing of the face, neck, and upper shoulders, which is believed to be histamine-mediated. Patients can develop facial flushing, generalized erythema, or both after epidural or intra-articular administration of glucocorticoids.
Here is a list of the drugs that can cause facial flushing:
-All vasodilators (e.g., nitroglycerin, prostaglandins)
-All calcium channel blockers
-Nicotinic acid (not nicotinamide)
-Morphine and other opiates
-Amyl nitrite and butyl nitrite
-Cholinergic drugs (e.g., metrifonate, anthelmintic drug)
-Bromocriptine used in Parkinson’s disease
-Thyrotropin-releasing hormone (TRH)
-Tamoxifen
-Cyproterone acetate
-Oral triamcinolone
-Cyclosporine
-Rifampin
-Sildenafil citrate
Steroids, steroid withdrawal syndrome and flushing
Steroid rosacea is an 'avoidable condition', and not only results sometimes from topical steroid use but also from the use of a vitamin A derivative called Roaccutane. In addition to disfigurement, steroid rosacea is accompanied by severe discomfort and pain. Withdrawal of the steroid is inevitably (first) accompanied by exacerbation of the disease; a trying experience for a patient and physician. Most dermatologists know not to prescribe a steroid for rosacea. (Source)
Forum posts from rosacea patients about drug related flushing
 Ruthuk wrote on January 3rd 2012: "Hello, I was diagnosed with premature ovarian failure (early menopause) in May. I've been struggling badly with hot flushes, despite being on an increasingly high dose of HRT. More recently I've noticed that my face is almost permanently red. In real life I was the palest person you could imagine, although not troubled by blushing. Now my skin looks suspiciously healthy most of the time and if I get hot (by which I mean any temperature above really freezing), do any sort of light exercise, have a glass of wine, I go bright red on my nose, and pretty red on my cheeks, rest of face, neck and upper chest. It seems to get worse over the course of the day too. But it is not a "normal" hot flush in that it just doesn't go away ... I am therefore wondering about rosacea. I believe that menopause often triggers rosacea, or perhaps my versions of hot flushes are just not the normal ones? My main problem, because I can live with the redness (and it's not the searing red I've seen in bad rosacea cases just very pink, like after you get out of a hot bath), is that I am UNBELIEVABLY HOT. It's making my life a misery. Rosacea or just menopause? It's weird that the HRT isn't taking the heat away, which is why I'm thinking I must have something else ...I'd be very grateful for any info."
Ruthuk wrote on January 3rd 2012: "Hello, I was diagnosed with premature ovarian failure (early menopause) in May. I've been struggling badly with hot flushes, despite being on an increasingly high dose of HRT. More recently I've noticed that my face is almost permanently red. In real life I was the palest person you could imagine, although not troubled by blushing. Now my skin looks suspiciously healthy most of the time and if I get hot (by which I mean any temperature above really freezing), do any sort of light exercise, have a glass of wine, I go bright red on my nose, and pretty red on my cheeks, rest of face, neck and upper chest. It seems to get worse over the course of the day too. But it is not a "normal" hot flush in that it just doesn't go away ... I am therefore wondering about rosacea. I believe that menopause often triggers rosacea, or perhaps my versions of hot flushes are just not the normal ones? My main problem, because I can live with the redness (and it's not the searing red I've seen in bad rosacea cases just very pink, like after you get out of a hot bath), is that I am UNBELIEVABLY HOT. It's making my life a misery. Rosacea or just menopause? It's weird that the HRT isn't taking the heat away, which is why I'm thinking I must have something else ...I'd be very grateful for any info."Judworth replied: "Hello Ruthuk, Do you get any sensitivity or pain with the flushing? I am approaching menopause & find that the 'hot flushes' that I get with menopause is a very different feeling to a rosacea flush/heat. I am taking beta blockers for rosacea & it appears to be helping confine my hot flushes to my body! Judy"
And Judworth wrote on May 2nd 2014: "Hello Wendy, I do hope that you don't mind me replying. I am 56 next month (sadly still perimenopausal) but my rosacea HAS got better over the years. It started when I was 44 and I would get hourly flushing............ now although I flush, get P&P's, the real attacks are maybe 2-5 times a month (I know as I keep a rosacea diary!). The longer the months between periods are, I find things are so much better, it's only the build up to yet another one that will cause me pain. I hope that gives you some hope for the future? Hugs Judy"
Some drugs and medications are known to have the potential to induce facial flushing. Some of them are: morphine, sodium monoglutamate, nitrates, calcium channel blockers, TRH injection, nicotinic acid and alcohol. Other potential suspects are corticotropin- releasing hormone and doxorubicin.
Note: Topical steroids can cause flushing or worsen existing rosacea
Flushing is a side effect of sildenafil citrate in 12% of patients. Systemic administration of morphine can cause flushing of the face, neck, and upper shoulders, which is believed to be histamine-mediated. Patients can develop facial flushing, generalized erythema, or both after epidural or intra-articular administration of glucocorticoids.
Here is a list of the drugs that can cause facial flushing:
-All vasodilators (e.g., nitroglycerin, prostaglandins)
-All calcium channel blockers
-Nicotinic acid (not nicotinamide)
-Morphine and other opiates
-Amyl nitrite and butyl nitrite
-Cholinergic drugs (e.g., metrifonate, anthelmintic drug)
-Bromocriptine used in Parkinson’s disease
-Thyrotropin-releasing hormone (TRH)
-Tamoxifen
-Cyproterone acetate
-Oral triamcinolone
-Cyclosporine
-Rifampin
-Sildenafil citrate
Steroids, steroid withdrawal syndrome and flushing
prolonged time with topical steroids, the least severe consequence is that the rosacea may at first respond and clear up (especially the p&p subtype 2), but inevitably the signs of steroid atrophy will emerge with thinning of the skin and marked increase in telangiectasis. The complexion becomes dark red often. Soon the surface can become studded with round, follicular, deep papulopustules, firm nodules and even secondary comedones. The appearance of the facial skin redness can soon become shocking with a flaming red, scaling, papule-covered face. Steroid creams can in the long term thin the epidermis permanently. At worst, those with no rosacea symptoms but a predisposition for the illness will find that steroid use can trigger the rosacea to erupt. Or those with existing rosacea can find that even a simple steroid inhaler for asthma can sent their rosacea into a much worse state. Oral prednisone can do the same thing but most notorious are the topical cortisone creams. It can take a long time and the help of a dermatologist to wane skin off of a steroid cream addiction and things get worse before they get better. Although many people don't have lasting damage from short term hydrocortisone cream use (the least heavy form of topical steroids), in my own case a simple hydrocortisone cream changed my life forever, and for the worse :( Back in 1999 I had normal skin, but already blushed from alcohol or when I went out dancing for instance in a hot place. But it never bothered me, nor did I ever have a hot flushed feeling. But three days of hydrocortisone cream use on my face for an eczema flare sent me right into rosacea misery. The flushing never went away again in my case.
Steroid rosacea is an 'avoidable condition', and not only results sometimes from topical steroid use but also from the use of a vitamin A derivative called Roaccutane. In addition to disfigurement, steroid rosacea is accompanied by severe discomfort and pain. Withdrawal of the steroid is inevitably (first) accompanied by exacerbation of the disease; a trying experience for a patient and physician. Most dermatologists know not to prescribe a steroid for rosacea. (Source)
Cigarette Flushing
Smoking, a vascular
dilator which robs the skin of oxygen, is a potent initiator of telangiectasis and the symptoms of facial skin redness. The smoker may have a variety of medical problems such as high blood pressure and mineral deficiencies which can cause the appearance of
telangiectasis. I discussed smoking, nicotine and rosacea also in this other blog post.Forum posts from rosacea patients about drug related flushing
 There are really many, many forum posts about steroid-induced rosacea. It is a very serious potential side effect of steroid use and made many victims along the way, some who never had flushing issues prior to taking steroids or roaccutane. Brady Barrows collected a few anecdotal threads on steroid induced rosacea.
There are really many, many forum posts about steroid-induced rosacea. It is a very serious potential side effect of steroid use and made many victims along the way, some who never had flushing issues prior to taking steroids or roaccutane. Brady Barrows collected a few anecdotal threads on steroid induced rosacea.Metiner wrote on February 20th 2013: "Hi, I know that steroid-induced rosacea is actually not rosacea, but mimics it. Therefore it might heal. I had rosacea in a tiny area on my face and I was given a steroid cream. I used it for about 10 days. A few months after I went off it, my rosacea exploded on my entire face and looks horrible. Now, do I have steroid-induced rosacea? Even though I already had rosacea before using the creams? The horrible change before and after steroids are unbelievable. My rosacea was very mild and small for about 6 months, and then I applied steroid on it for 10 days. In about 4 months the rosacea got so bad that my face was unrecognizable. Therefore it makes me think I might have steroid-induced rosacea. I appreciate your thoughts.. "
Bloem replied: "I used steroid creams before I knew I had rosacea. It was pretty strong. It got really bad for a month - 6 weeks. And it slowly got better, but it took like a year. It did get better, but it never went away completely. The only thing that helped was avoiding triggers, (creams etc that stung) and IPL. People can hardly tell now. Whatever the cause, if it is really bad now, it's probably due to the steroids and it will get a lot better. It takes a lot of time."
 Steph623 wrote on April 9th 2012: (its a very long post, I shortened it a bit) ":( Unhappy Steroid Induced Rosacea? Hi. New to the forum, but not new to skin problems. I'm 47 years old and have had a history of hormone-related acne. When I was younger (in my late 20s) I was treated, successfully, with Accutane. That settled the worst of my acne, but I struggled with it on and off for years due to endometriosis and polycystic ovarian disease. [..] About 14 months ago or so, my formerly pretty oily skin was becoming very dry. It was uncomfortably so but any use of moisturizers would usually set off a round of pimples. This is just the nature of my skin. With all the dryness, is started developing scaly patches. Well, stupid me, I decided to treat the scaly patches with steroid cream. I'd done this in the past, but only for very brief periods.[..] Eventually, I was treating pretty much everything from the bottom of my eyes down to the middle of my neck with a thin film of the stuff, twice a day. [..] About 4 months ago, I started getting these weepy bumps that were tender or itchy. They looked like pimples to a degree, but had an entirely different nature about them than I was used to (and goodness knows I had years of experience with acne). They couldn't be popped and they seemed to spread in clusters over my cheeks and chin. They also started getting a 'flushed' look to them. I started to suspect rosacea since I am of celtic heritage and I know my grandmother had rosacea, so I wasn't entirely unfamiliar. Well, last week, I'd about had it with all of this irritation and finally went to my long-time dermatologist - someone I hadn't needed to see in a number of years. He took one look at me and said, 'Looks like rosacea.' I told him what I had been using: desonide, tea tree and he said, 'Stop the steriod!' Although, he didn't explain why other than to say that it can worsen rosacea. In addition, he gave me an prescription for doxycycline 50 mg 1x/day and a topical gel called Aczone (dapsone). Well, that night I did not use the desonide nor the tea tree but only applied the Aczone and took my doxycycline. The next day my skin looked pretty good. It was 24 hours after THAT that all hell broke loose. I woke up feeling like my face was on fire and I looked in the mirror and nearly fainted. My face was bright red from the eyes down to my mid-neck and it had dozens of the painful, weepy pimple-things that made my entire face look like the skin of an orange! I was horrified. My first thought was that I was allergic to the new Aczone. My second thought was this was some sort of 'purge' as I had gone through that lovely phase a few times in my life. Well, I stuck it out for 4 days and each day it has gotten worse. The pain is now accompanied by severe itching and when I smile, my skin looks all atrophied and wrinkly. Trying to calm myself down and think rationally, Friday evening I began researching [..] which led me to the information on steroid-induced rosacea. I'm now starting to think that I have steroid-induced rosacea. [..] I would appreciate any comments, recommendations or feedback anyone could give me. I've read a number of posts by Ghost here and I'm very intrigued by his account of treating demodex. Thanks for reading."
Steph623 wrote on April 9th 2012: (its a very long post, I shortened it a bit) ":( Unhappy Steroid Induced Rosacea? Hi. New to the forum, but not new to skin problems. I'm 47 years old and have had a history of hormone-related acne. When I was younger (in my late 20s) I was treated, successfully, with Accutane. That settled the worst of my acne, but I struggled with it on and off for years due to endometriosis and polycystic ovarian disease. [..] About 14 months ago or so, my formerly pretty oily skin was becoming very dry. It was uncomfortably so but any use of moisturizers would usually set off a round of pimples. This is just the nature of my skin. With all the dryness, is started developing scaly patches. Well, stupid me, I decided to treat the scaly patches with steroid cream. I'd done this in the past, but only for very brief periods.[..] Eventually, I was treating pretty much everything from the bottom of my eyes down to the middle of my neck with a thin film of the stuff, twice a day. [..] About 4 months ago, I started getting these weepy bumps that were tender or itchy. They looked like pimples to a degree, but had an entirely different nature about them than I was used to (and goodness knows I had years of experience with acne). They couldn't be popped and they seemed to spread in clusters over my cheeks and chin. They also started getting a 'flushed' look to them. I started to suspect rosacea since I am of celtic heritage and I know my grandmother had rosacea, so I wasn't entirely unfamiliar. Well, last week, I'd about had it with all of this irritation and finally went to my long-time dermatologist - someone I hadn't needed to see in a number of years. He took one look at me and said, 'Looks like rosacea.' I told him what I had been using: desonide, tea tree and he said, 'Stop the steriod!' Although, he didn't explain why other than to say that it can worsen rosacea. In addition, he gave me an prescription for doxycycline 50 mg 1x/day and a topical gel called Aczone (dapsone). Well, that night I did not use the desonide nor the tea tree but only applied the Aczone and took my doxycycline. The next day my skin looked pretty good. It was 24 hours after THAT that all hell broke loose. I woke up feeling like my face was on fire and I looked in the mirror and nearly fainted. My face was bright red from the eyes down to my mid-neck and it had dozens of the painful, weepy pimple-things that made my entire face look like the skin of an orange! I was horrified. My first thought was that I was allergic to the new Aczone. My second thought was this was some sort of 'purge' as I had gone through that lovely phase a few times in my life. Well, I stuck it out for 4 days and each day it has gotten worse. The pain is now accompanied by severe itching and when I smile, my skin looks all atrophied and wrinkly. Trying to calm myself down and think rationally, Friday evening I began researching [..] which led me to the information on steroid-induced rosacea. I'm now starting to think that I have steroid-induced rosacea. [..] I would appreciate any comments, recommendations or feedback anyone could give me. I've read a number of posts by Ghost here and I'm very intrigued by his account of treating demodex. Thanks for reading."Prem replied on May 5th 2012: "I think I may also have steroid induced rosacea. I'm not sure if I do have rosacea, but either way....my eyes also burn, and I have dry rough scaly skin that is spreading. It sounds just like yours. I used steroid cream for about 5 months, I stopped it now. So yeah... it's become worse and worse over the past 5 months. Could you please look at my post and help tell me if it is rosacea?" -Here, here, here and here are more Forum Threads about steroid induced rosacea.
Allergies, Food intolerance & coeliac disease
Please also read my Food blog post if interested in this topic :) Not everyone with rosacea has food triggers, but many do. Triggers can vary per person, but there are some foods that are more often causing flushing issues than others. Some of them include spicy foods, monosodium glutamate
(MSG), a food additive often found in Asian food for instance. Nitrites
and sulfites (additives in many foods), thermally hot foods and
beverages, alcohol and caffeine. Foods high in histamine or sugar can also cause redness or flushing for some.Heavy Meal and Sugar/Carbohydrate Flushing
Facial skin flushing or vascular dilation can be caused by stress on the digestive system (eating heavier meals), resulting in a higher blood flow to the digestive system with the residual blood being heavier to the face (so more blood flow circulation to help digest all that food, and therefore also more blood that circulates to the face area, causing more flushing issues). The digestion process itself also produces some heat and increased temperature in the body, a bit more for women and children than it does for men. You can limit this type of flushing by eating smaller meals, spaced out over the day, with some healthy snacks to keep your blood sugar level stable and prevent the digestion system from being 'bombarded' all at once with a massive meal. This will also maintain the proper blood sugar content for energy to prevent fatigue or exhaustion. Various foods stimulate blood flow differently.
Simple carbohydrates such as donuts, white wheat products, sugars, alcohol, etc. enter the bloodstream quickly, causing hyperglycemia (high glucose spikes). This rapid influx of sugar into the bloodstream is a potent vasodilator. Carbohydrates are needed for energy and are a part of most people's meals; however try to switch from simple to complex carbohydrates. Whole grain products instead of 'white' rice and flour, for instance. However, in the next paragraph things will get more messed up and complicated, because complex carbs actually also heat the body up when they get digested.... Why is all this so complex for us rosaceans?
Fiber intake prolongs digestion and prevents
the sudden influx of sugars into the bloodstream (with the resultant facial skin
flushing for some). (source).
 Foods That Make You Hotter
Foods That Make You Hotter
Ice cream: It turns out the fat content in ice cream actually makes your body warmer. Foods that contain more fat, protein, and carbohydrates often heat the body up a little bit while digesting food. The sheer temperature difference gives a cooling sensation, but when your body starts to digest, you feel warm because your body has to provide energy to digest that food product. Fat is notorious for moving slowly through the digestive system so it takes more energy to digest that fat. Anytime you are putting more energy through the system, whether it be digestion or weight lifting, your body has a tendency to heat up.
Brown rice: Complex carbohydrates like rice and other whole grains are also harder to digest, making the body warmer during the process. Anything with a lot of complex carbohydrates and processed foods like rice and cereal products can be more warming than cooling. But they also keep your blood glucose level more stable, which is a benefit again.
Beer: Alcohol can dehydrate you and make your body flushed - a process called vasodilatation, which is caused by the widening of blood vessels. This can cause your skin to heat up. When the body starts to vasodilate, you can flush pretty heavily. It is going to be warming, especially in the surface capillaries in your face.This also depends on how much alcohol you consume in one sitting. The more alcohol someone drinks, the more flushing will occur. (source).
 Foods That Make You Hotter
Foods That Make You HotterIce cream: It turns out the fat content in ice cream actually makes your body warmer. Foods that contain more fat, protein, and carbohydrates often heat the body up a little bit while digesting food. The sheer temperature difference gives a cooling sensation, but when your body starts to digest, you feel warm because your body has to provide energy to digest that food product. Fat is notorious for moving slowly through the digestive system so it takes more energy to digest that fat. Anytime you are putting more energy through the system, whether it be digestion or weight lifting, your body has a tendency to heat up.
Brown rice: Complex carbohydrates like rice and other whole grains are also harder to digest, making the body warmer during the process. Anything with a lot of complex carbohydrates and processed foods like rice and cereal products can be more warming than cooling. But they also keep your blood glucose level more stable, which is a benefit again.
Beer: Alcohol can dehydrate you and make your body flushed - a process called vasodilatation, which is caused by the widening of blood vessels. This can cause your skin to heat up. When the body starts to vasodilate, you can flush pretty heavily. It is going to be warming, especially in the surface capillaries in your face.This also depends on how much alcohol you consume in one sitting. The more alcohol someone drinks, the more flushing will occur. (source).
Watermelon: As a general rule, the higher the water content in a food, the more likely it will keep your temperature down. Watermelon is chock-full of water, which slows down digestion and takes less energy from the body. Note that melons are high in salicylate, another substance that can worsen some rosaceans flushing, for those sensitive to salicylates. If you flush from aspirin, you might also flush from high contents of salicylates in food.
Leafy greens: Most raw fruits and vegetables are 80-95% water, and anything that contains a lot of water is very easy to digest and goes through the digestive system very quickly, giving you a cooling sensation. Easy digestion means less energy and heat.
Peppers: Spicy foods can make you sweat, which provides a cooling sensation. Peppers are often consumed in countries close to the equator because they are perceived as cooling foods primarily because they influence the body when you perspire, and through evaporative cooling, you feel cooler. It doesn’t cool you to the core, but it cools the skin. Note, this is obviously not wise to eat for anyone with rosacea and flushing issues. This tip only applies to the general population with normal skin I think.
Inflammatory foods
Internal inflammation can happen for a host of different reasons: using high temperatures when cooking food, eating processed foods, sugar, trans fats etc. A high level of inflammation within the body can cause many health problems and stir up both rosacea and facial flushing. Inflammatory foods include sugar, processed food, any food that went into the deep fry, alcohol. According to the Traditional Chinese doctors I visited, garlic, unions, ginger, spices, predator fish types, lamb, citrus fruits, tomatoes, strawberries, chocolate and dairy and wheat products also cause inflammation in the body of those struggling with inflammatory skin diseases including rosacea and eczema.
Top 10 anti-inflammatory foods
1. Wild Alaskan Salmon: Salmon contains anti-inflammatory omega-3s (wild is better than farmed) and has been known to help numerous ailments. Note, fish can be high in histamine and heavy chemicals like mercury and can actually worsen flushing for some. It's trial and error with what fish types your rosacea tolerates and which not.
2. Kelp: High in fiber, this brown algae extract helps control liver and lung cancer, douses inflammation, and is anti-tumor and anti-oxidative. Kombu, wakame and arame are good sources.
3. Extra Virgin Olive Oil: The secret to longevity in Mediterranean culture, this oil provides a healthy dose of fats that fights inflammation, can help lower risks of asthma and arthritis, as well as protect the heart and blood vessels.
4. Cruciferous Vegetables: Broccoli, brussel sprouts, kale and cauliflower are all loaded with antioxidants. Naturally detoxifying, they can help rid the body of possible harmful compounds.
5. Blueberries: Blueberries not only reduce inflammation, but they can protect the brain from aging and prevent diseases, such as cancer and dementia. Aim for organic berries, as pesticides are hard to wash away due to their size. Note that blueberries are high in salicylate, another substance that can worsen some rosaceans flushing, for those sensitive to salicylates. If you flush from aspirin, you might also flush from high contents of salicylates in food.
6. Turmeric: This powerful Asian spice contains a natural anti-inflammatory compound, curcumin, which is often found in curry blends. It is said to have the same effect as over-the counter pain relievers (but without their side effects). Note that turmeric is a spice and while it helps some rosceans, it can worsen symptoms as well for some (for me it did when I tried it with bromelaine).
7. Ginger: Ginger contains a host of health benefits. Among them, it helps reduce inflammation and control blood sugar. Ginger tea is a great addition to any diet. Note that ginger is a spice and while it helps some rosceans, it can worsen symptoms as well for some. My traditional Chinese doctors warn against it, as it can heat the body up they say, for people with inflammatory skin diseases.
8. Garlic: Though a little more inconsistent (in terms of research), garlic can help reduce inflammation, regulate glucose and help your body fight infection. Note that garlic might help some rosceans, it can worsen symptoms for some. My traditional Chinese doctors warn against it, as it can heat the body up they say, for people with inflammatory skin diseases.
9. Green Tea: Like produce, this tea contains anti-inflammatory flavonoids that may even help reduce the risks of certain cancers. Note that some people react to the tannins and other chemicals in some types of green tea, and that a good alternative is to make tea from rosemary or thyme, both have anti inflammatory substances in them.
10. Sweet Potato: A great source of complex carbs, fiber, beta-carotene, manganese and vitamin B6 and C, these potatoes actually help heal inflammation in the body. Note, I love sweet potatoes! My rosacea handles them well, in moderation.
Top 10 inflammatory foods
 These
foods have been linked to obesity, increased risks of numerous diseases
and can elevate inflammation levels in the body and worsen auto-immune
diseases
These
foods have been linked to obesity, increased risks of numerous diseases
and can elevate inflammation levels in the body and worsen auto-immune
diseases1. Sugar: Sugar is everywhere. Try and limit processed foods, desserts and snacks with excess sugar. Opt for fruit instead.
2. Common Cooking Oils: Safflower, soy, sunflower, corn, and cottonseed. These oils promote inflammation and are made with cheaper ingredients.
3. Trans Fats: Trans fats increase bad cholesterol, promote inflammation, obesity and resistance to insulin. They are in fried foods, fast foods, commercially baked goods, such as peanut butter and items prepared with partially hydrogenated oil, margarine and vegetable oil.
4. Dairy: While kefir and some yogurts are acceptable, dairy is hard on the body. Milk is a common allergen that can trigger inflammation, stomach problems, skin rashes, hives and even breathing difficulties.
5. Feedlot-Raised Meat: Animals who are fed with grains like soy and corn contain higher inflammation levels. Some of these animals also gain excess fat and are injected with hormones and antibiotics. If possible, consider opting for organic, free-range meats who have been fed natural diets.
6. Red and Processed Meat: Red meat contains a molecule that humans don't naturally produce called Neu5GC. It is said to trigger an inflammatory response in the body. I eat red meat, but try to reduce red meat consumption to twice or three times a week perhaps.
7. Alcohol: Alcohol not only dilates the blood vessels, but regular consumption of alcohol also causes irritation and inflammation to numerous organs, which can also lead to cancer.
8. Refined Grains: "Refined" products have no fiber and have a high glycemic index. They spike the blood glucose level which can cause flushing. Consider trying to replace products like white rice, white flour, white bread, pasta, pastries with minimally processed grains.
9. Artificial Food Additives:
Aspartame and MSG are two common food additives that can trigger
inflammation responses.
10. Fill in the Blank: Sometimes, you may develop a reaction or even an allergy to a specific food. Coffee, certain vegetables, cheese... there might be a trigger you aren't even aware of. Or you are not actually allergic to the food, but intolerant to it (sensitivity that will cause you symptoms, but that won't show up in a standard blood test for allergies). Try and take a few foods out to see how you feel and slowly incorporate them back in to see if there might be a hidden culprit lurking in your diet.
Alcohol flushing
Alcohol is a concentrated source of calories and is metabolized very quickly. This causes the blood vessels to dilate, causing facial redness symptoms. The best way to avoid this type of flushing is by not drink any alcohol. Alcohol is a vasodilator. All alcohol is also fermented (thus higher in histamine), but because beer and wines (red wine being the worst) are not further distilled, they can cause the symptoms of allergy facial skin redness for many rosacea sufferers. Red wine also contains tannins and sulfites which can make you even more flushed and red than from the alcohol itself. Alcohol is also a diuretic which pushes water out of the body cells. In this state of dehydration, the body is also more prone to skin redness and flushing. Foreign beers imported into your country can also contain preservatives which can make for more redness. Domestic 'light beer' usually does not have as many carbohydrates and less alcohol content, making it the beer of choice for many. For many people it is also better to drink small amounts of gin, vodka, or whiskey diluted with water instead of sugary soft drinks, or mixes which also can stimulate the cardiovascular system. You should "chase" any alcoholic drink with water. Although these recommendations can help to minimize facial skin redness/flushing, the best advice if you find yourself constantly flushed after drinking an alcoholic beverage is to not drink any type of alcohol at all. In this Rosacea Forum post, patients rate their top alcohol triggers.
10. Fill in the Blank: Sometimes, you may develop a reaction or even an allergy to a specific food. Coffee, certain vegetables, cheese... there might be a trigger you aren't even aware of. Or you are not actually allergic to the food, but intolerant to it (sensitivity that will cause you symptoms, but that won't show up in a standard blood test for allergies). Try and take a few foods out to see how you feel and slowly incorporate them back in to see if there might be a hidden culprit lurking in your diet.
Alcohol flushing
Alcohol is a concentrated source of calories and is metabolized very quickly. This causes the blood vessels to dilate, causing facial redness symptoms. The best way to avoid this type of flushing is by not drink any alcohol. Alcohol is a vasodilator. All alcohol is also fermented (thus higher in histamine), but because beer and wines (red wine being the worst) are not further distilled, they can cause the symptoms of allergy facial skin redness for many rosacea sufferers. Red wine also contains tannins and sulfites which can make you even more flushed and red than from the alcohol itself. Alcohol is also a diuretic which pushes water out of the body cells. In this state of dehydration, the body is also more prone to skin redness and flushing. Foreign beers imported into your country can also contain preservatives which can make for more redness. Domestic 'light beer' usually does not have as many carbohydrates and less alcohol content, making it the beer of choice for many. For many people it is also better to drink small amounts of gin, vodka, or whiskey diluted with water instead of sugary soft drinks, or mixes which also can stimulate the cardiovascular system. You should "chase" any alcoholic drink with water. Although these recommendations can help to minimize facial skin redness/flushing, the best advice if you find yourself constantly flushed after drinking an alcoholic beverage is to not drink any type of alcohol at all. In this Rosacea Forum post, patients rate their top alcohol triggers.
This girl describes flushing from alcohol online
Many patients with rosacea have other symptoms that suggest the diagnosis of food allergies or sensitivities. A red nose, cheeks and red ears may act like warning lights that turn on when a food reaction starts. Other possible symptoms can be gastrointestinal disturbances, migraine headache, sinusitis and fatigue. Rosacea patients should ideally try to identify any food triggers they may have and avoid those foods or take an antihistamine before consuming it. Stimulants such as coffees, teas, soft drinks with caffeine and alcohol beverages can stimulate the system resulting in more facial redness or dilation. And if you find that your skin reacts badly to foods like tomatoes, citrus fruits, fermented foods, yogurt, old cheeses and chocolate for instance, it is possible that your skin reacts to foods high in histamine.
 Susybranch wrote on June 5th 2014 on The Rosacea Forum: "I had type 2 on my nose, and occasional papules with seb-derm. It could be tamed -- somewhat -- by Oracea and Metrogel, but these were a band-aid, and I was also having stomach issues and began to suspect food intolerance. As many on this board know, some of us who have Rosacea have found a connection to our digestive systems. In my case, I turned out to have so many mild -- but across the board-- food allergies, that the doctor diagnosed me with Leaky Gut syndrome. My immune system was reacting to
all these irritants by upsetting my stomach, and my skin. Rather than randomly cutting out food groups, my allergy test let me
know exactly what to avoid. (The doctor says that in a few weeks my
system should start to "re-set" and I will probably be able to eat most
of those foods again.) Between the new diet and the Prosacea, occasional Histame, along with some digestive enzymes and probiotics, I am almost entirely clear. I can even drink a little vodka -- not on my "verboten" list! I urge you all to get a full allergy workup, rather than shoot in the
dark about what foods to avoid. I spent a bit of money but saved myself
years of guessing."
Susybranch wrote on June 5th 2014 on The Rosacea Forum: "I had type 2 on my nose, and occasional papules with seb-derm. It could be tamed -- somewhat -- by Oracea and Metrogel, but these were a band-aid, and I was also having stomach issues and began to suspect food intolerance. As many on this board know, some of us who have Rosacea have found a connection to our digestive systems. In my case, I turned out to have so many mild -- but across the board-- food allergies, that the doctor diagnosed me with Leaky Gut syndrome. My immune system was reacting to
all these irritants by upsetting my stomach, and my skin. Rather than randomly cutting out food groups, my allergy test let me
know exactly what to avoid. (The doctor says that in a few weeks my
system should start to "re-set" and I will probably be able to eat most
of those foods again.) Between the new diet and the Prosacea, occasional Histame, along with some digestive enzymes and probiotics, I am almost entirely clear. I can even drink a little vodka -- not on my "verboten" list! I urge you all to get a full allergy workup, rather than shoot in the
dark about what foods to avoid. I spent a bit of money but saved myself
years of guessing."Pollen and contact allergy flushing
Spring in most countries is the time for pollen and mold spores with the result that it affects many rosacea sufferers. However, some areas have enough warmth and proper vegetation for pollen and mold spores year around. You may even see mold spores growing in your bathtub or shower. Other allergies can also stir up rosacea flushing, for instance dust mite allergy or cat dander allergy.
Gluten allergy
Acne rosacea has been brought in connection with gluten allergy, also called Celiac Disease, and with gluten intolerance. Celiac disease is an autoimmune disease. People respond badly here to a protein in certain grains, mostly wheat, barley and rye. The gluten itself is a protein made up of two protein parts, gliadin and glutenin. The gliadin part is responsible for the abnormal immune reaction that causes gluten sensitivity and celiac disease for some people. Between 0.5 and 1% of the world’s population suffers from gluten-sensitivity. Gluten sensitivity is not the same as a gluten allergy. The gluten proteins of corn and rice lack the gliadin part and do therefore not cause any sensitivity. The immune systems' overreaction to wheats' gluten causes celiac disease, in which the lining of the small intestine becomes chronically inflamed. Anecdotal evidence suggests that those following a gluten-free diet can sometimes reduce flare-ups of rosacea (source). Some rosacea patients who are diagnosed with gluten intolerance or celiac disease have noticed that the gluten-free diet clears up much of the redness apparent with rosacea. While there is not much medical evidence yet to link the two conditions, it is possible that there is a connection. It is possible that the inflammation of the intestines contributes to an overall stronger inflammatory response in the facial skin of rosacea patients. Symptoms of gluten sensitivity or celiac disease include chronic diarrhea, cramps, bloating, bowel disturbances, changes in stool, flatulence, weight loss, weakness, fatigue, joint pain, headaches, depression, abnormal menstrual cycles and malabsorption of essential nutrients, which could result in secondary symptoms such as psychological and neurological problems. The gluten sensitivity makes it difficult for the body to absorb vitamins, in particular vitamin D. Read more on wikipedia-gluten sensitivity or wikipedia coeliac disease.
This is an article about gluten sensitivity; it explains gluten intolerance and -allergy and the other grains that might cause problems for your system and why:
"(Quote) Two years ago, at the recommendation of a nutritionist, I stopped eating wheat and a few other grains. Within a matter of days the disabling headaches and fatigue that I had been suffering for months vanished. Initially my gastroenterologist interpreted this resolution of my symptoms as a sign that I perhaps suffered from celiac disease, a peculiar disorder in which the immune system attacks a bundle of proteins found in wheat, barley and rye that are collectively referred to as gluten. The misdirected assault ravages and inflames the small intestine, interfering with the absorption of vital nutrients and thereby causing bloating, diarrhea, headaches, tiredness and, in rare cases, death. Yet several tests for celiac disease had come back negative. Rather my doctors concluded that I had nonceliac “gluten sensitivity,” a relatively new diagnosis. The prevalence of gluten sensitivity is not yet clear, but some data suggest it may afflict as many as 6 percent of Americans, six times the number of people with celiac disease. (...) Lately, however, some researchers are wondering if they were too quick to pin all the blame for these problems on gluten. A handful of new studies suggest that in many cases gluten sensitivity might not be about gluten at all. Rather it may be a misnomer for a range of different illnesses triggered by distinct molecules in wheat and other grains.“You know the story of the blind man and the elephant? Well, that’s what gluten-sensitivity research is right now,” says Sheila Crowe, head of research at the gastroenterology division at the School of Medicine at the University of California, San Diego."
Lactose intolerance
Lactose intolerance, also called lactase deficiency and hypolactasia, is the inability to digest lactose, a sugar found in milk and to a lesser extent dairy products. People who are lactose intolerant have lower levels of lactase -an enzyme that is needed to break lactose down into glucose and galactose in the digestive system-, which may be genetic or environmentally induced. Lactose, a disaccharide molecule found in milk and dairy products, cannot be directly absorbed through the wall of the small intestine into the bloodstream so, in the absence of lactase, passes intact into the colon. Bacteria in the colon can metabolise lactose, and the resulting fermentation produces copious amounts of gas (a mixture of hydrogen, carbon dioxide and methane) that causes the various abdominal symptoms. The unabsorbed sugars and fermentation products also raise the osmotic pressure of the colon, causing an increased flow of water into the bowels (diarrhea). When people with this deficiency do consume enough amounts of lactose, this usually causes symptoms like abdominal bloating and cramps, flatulence, diarrhea, nausea, rumbling sounds coming from the stomach or vomiting. The severity of symptoms typically increases with the amount of lactose consumed; most lactose-intolerant people can tolerate a certain level of lactose in their diet without ill-effect. Some studies have produced evidence that milk consumption by lactose intolerant individuals may be a significant cause of inflammatory bowel disease. Wiki states that most mammals normally stop to produce lactase, and will naturally become lactose intolerant after weaning, but some human populations have developed lactase persistence, in which lactase production continues into adulthood. (Perhaps this is because humans began to drink milk as part of their normal diet at some point in time, and evolution then made us produce lactase for a longer period of time?). It is estimated that 75% of adults worldwide show some decrease in lactase activity during adulthood. The frequency of lactose intolerance ranges from 5% in Northern European countries (England, Scotland, Ireland, Scandinavia, and Iceland) to 71% in Italy (Sicily) to more than 90% in most African and Asian countries. This distribution is now thought to have been caused by recent natural selection favoring lactase-persistent individuals in cultures in which dairy products are available as a food source. Small intestine problems that can cause lactose intolerance include bacterial overgrowth, celiac disease and Crohn's disease.
Acne rosacea has been brought in connection with gluten allergy, also called Celiac Disease, and with gluten intolerance. Celiac disease is an autoimmune disease. People respond badly here to a protein in certain grains, mostly wheat, barley and rye. The gluten itself is a protein made up of two protein parts, gliadin and glutenin. The gliadin part is responsible for the abnormal immune reaction that causes gluten sensitivity and celiac disease for some people. Between 0.5 and 1% of the world’s population suffers from gluten-sensitivity. Gluten sensitivity is not the same as a gluten allergy. The gluten proteins of corn and rice lack the gliadin part and do therefore not cause any sensitivity. The immune systems' overreaction to wheats' gluten causes celiac disease, in which the lining of the small intestine becomes chronically inflamed. Anecdotal evidence suggests that those following a gluten-free diet can sometimes reduce flare-ups of rosacea (source). Some rosacea patients who are diagnosed with gluten intolerance or celiac disease have noticed that the gluten-free diet clears up much of the redness apparent with rosacea. While there is not much medical evidence yet to link the two conditions, it is possible that there is a connection. It is possible that the inflammation of the intestines contributes to an overall stronger inflammatory response in the facial skin of rosacea patients. Symptoms of gluten sensitivity or celiac disease include chronic diarrhea, cramps, bloating, bowel disturbances, changes in stool, flatulence, weight loss, weakness, fatigue, joint pain, headaches, depression, abnormal menstrual cycles and malabsorption of essential nutrients, which could result in secondary symptoms such as psychological and neurological problems. The gluten sensitivity makes it difficult for the body to absorb vitamins, in particular vitamin D. Read more on wikipedia-gluten sensitivity or wikipedia coeliac disease.
This is an article about gluten sensitivity; it explains gluten intolerance and -allergy and the other grains that might cause problems for your system and why:
"(Quote) Two years ago, at the recommendation of a nutritionist, I stopped eating wheat and a few other grains. Within a matter of days the disabling headaches and fatigue that I had been suffering for months vanished. Initially my gastroenterologist interpreted this resolution of my symptoms as a sign that I perhaps suffered from celiac disease, a peculiar disorder in which the immune system attacks a bundle of proteins found in wheat, barley and rye that are collectively referred to as gluten. The misdirected assault ravages and inflames the small intestine, interfering with the absorption of vital nutrients and thereby causing bloating, diarrhea, headaches, tiredness and, in rare cases, death. Yet several tests for celiac disease had come back negative. Rather my doctors concluded that I had nonceliac “gluten sensitivity,” a relatively new diagnosis. The prevalence of gluten sensitivity is not yet clear, but some data suggest it may afflict as many as 6 percent of Americans, six times the number of people with celiac disease. (...) Lately, however, some researchers are wondering if they were too quick to pin all the blame for these problems on gluten. A handful of new studies suggest that in many cases gluten sensitivity might not be about gluten at all. Rather it may be a misnomer for a range of different illnesses triggered by distinct molecules in wheat and other grains.“You know the story of the blind man and the elephant? Well, that’s what gluten-sensitivity research is right now,” says Sheila Crowe, head of research at the gastroenterology division at the School of Medicine at the University of California, San Diego."
Lactose intolerance
Lactose intolerance, also called lactase deficiency and hypolactasia, is the inability to digest lactose, a sugar found in milk and to a lesser extent dairy products. People who are lactose intolerant have lower levels of lactase -an enzyme that is needed to break lactose down into glucose and galactose in the digestive system-, which may be genetic or environmentally induced. Lactose, a disaccharide molecule found in milk and dairy products, cannot be directly absorbed through the wall of the small intestine into the bloodstream so, in the absence of lactase, passes intact into the colon. Bacteria in the colon can metabolise lactose, and the resulting fermentation produces copious amounts of gas (a mixture of hydrogen, carbon dioxide and methane) that causes the various abdominal symptoms. The unabsorbed sugars and fermentation products also raise the osmotic pressure of the colon, causing an increased flow of water into the bowels (diarrhea). When people with this deficiency do consume enough amounts of lactose, this usually causes symptoms like abdominal bloating and cramps, flatulence, diarrhea, nausea, rumbling sounds coming from the stomach or vomiting. The severity of symptoms typically increases with the amount of lactose consumed; most lactose-intolerant people can tolerate a certain level of lactose in their diet without ill-effect. Some studies have produced evidence that milk consumption by lactose intolerant individuals may be a significant cause of inflammatory bowel disease. Wiki states that most mammals normally stop to produce lactase, and will naturally become lactose intolerant after weaning, but some human populations have developed lactase persistence, in which lactase production continues into adulthood. (Perhaps this is because humans began to drink milk as part of their normal diet at some point in time, and evolution then made us produce lactase for a longer period of time?). It is estimated that 75% of adults worldwide show some decrease in lactase activity during adulthood. The frequency of lactose intolerance ranges from 5% in Northern European countries (England, Scotland, Ireland, Scandinavia, and Iceland) to 71% in Italy (Sicily) to more than 90% in most African and Asian countries. This distribution is now thought to have been caused by recent natural selection favoring lactase-persistent individuals in cultures in which dairy products are available as a food source. Small intestine problems that can cause lactose intolerance include bacterial overgrowth, celiac disease and Crohn's disease.
Testing for lactose intolerance
 Your
doctor may suspect lactose intolerance based on your symptoms and your
response to reducing the amount of dairy foods in your diet. Your doctor
can confirm the diagnosis by conducting one or more of the following
tests:
Your
doctor may suspect lactose intolerance based on your symptoms and your
response to reducing the amount of dairy foods in your diet. Your doctor
can confirm the diagnosis by conducting one or more of the following
tests:*Lactose tolerance test. The lactose tolerance test gauges your body's reaction to a liquid that contains high levels of lactose. Two hours after drinking the liquid, you'll undergo blood tests to measure the amount of glucose in your bloodstream. If your glucose level doesn't rise, it means your body isn't properly digesting and absorbing the lactose-filled drink.
*Hydrogen breath test. This test also requires you to drink a liquid that contains high levels of lactose. Then your doctor measures the amount of hydrogen in your breath at regular intervals. Normally, very little hydrogen is detectable. However, if your body doesn't digest the lactose, it will ferment in the colon, releasing hydrogen and other gases, which are absorbed by your intestines and eventually exhaled. Larger than normal amounts of exhaled hydrogen measured during a breath test indicate that you aren't fully digesting and absorbing lactose.
*Stool acidity test. For infants and children who can't undergo other tests, a stool acidity test may be used. The fermentation of undigested lactose creates lactic acid and other acids that can be detected in a stool sample (source).
 What foods to avoid when going lactose free?
What foods to avoid when going lactose free?Lactose is present in two large food categories—conventional dairy products, and as a food additive (casein, caseinate, whey), which may contain traces of lactose. If you want to avoid eating lactose, the prime product to avoid is milk. Lactose is a water-soluble substance. Most lactose is found in the water-based portions of dairy. Less lactose will be found in the fatty contents of dairy products like butter, as the butter-making process separates the majority of milk's water components from the fat components. Lactose will still be present in small quantities of the butter though, unless it is also fermented to produce cultured butter. But clarified butter contains very little lactose and is safe for most lactose-intolerant people. Dairy products that are "reduced-fat" or "fat-free" generally have slightly higher lactose content. People can be more tolerant of traditionally made yogurt than milk, because it contains lactase produced by the bacterial cultures used to make the yogurt. Frozen yogurt will contain similarly reduced lactose levels. With cheese, fermentation and higher fat content contribute to lesser amounts of lactose. Traditionally made Emmental or Cheddar might contain 10% of the lactose found in whole milk. In addition, the ageing methods of traditional cheeses (sometimes over two years) reduce their lactose content to practically nothing. Commercial cheeses, however, are often manufactured by processes that do not have the same lactose-reducing properties. You can read more on lactose intolerance on wikipedia.
 Here are some more post suggestions:
Here are some more post suggestions:Rosacea and Gluten
A rosacea blog about gluten
Does rosacea always get worse? Forum thread
Acne forum; is eliminating dairy the answer?
Acne help, rosacea and SIBO
Is gluten free helping? Rosacea forum
Gluten-wheat free diet, Rosacea Forum
Gluten intolerance, the culprit, Rosacea Forum
Does a low carb, no sugar or dairy help with skin burning and irritation?
Should I give up dairy?
Erythromelalgia (EM) is also a more rare cause of facial flushing
Erythromelalgia (EM) is a rare neurovascular disorder that typically affects the skin of the feet or hands, or both, and causes visible redness, intense heat and quite severe burning pain. It makes the blood vessels of the extremities (mostly hand and feet but also at times the face) episodically blocked, then become overly dilated and inflamed, causing throbbing heat, redness and burning pain. The pain is caused by the small fiber sensory nerves. The attacks are periodic and are commonly triggered by heat, pressure, mild activity, exertion, insomnia or stress. The term erythromelalgia describes the syndrome: erythros (redness), melos (extremity) and algia (pain). It can also affect the legs and arms or the face, nose and ears. Even in mild-to-moderate cases, normal functioning such as walking, standing, working, socializing, exercising, and sleeping may be impaired. Triggers for flare ups can be warm temperatures and even mild exercise. Cooling the hot body parts relieves the pain, as does elevating the affected areas. This is one of the hallmark characteristics of EM: cooling bringing relief. The cause of EM is unknown in the vast majority of cases. Only 5% of patients is said to have a genetically inherited cause. Peripheral neuropathies are often at the root of the problem and sometimes EM may be secondary to other disorders like the blood disease polycythemia. Recent research in the U.S. found the incidence of EM (the number of people a year diagnosed with EM) to be 1.3 per 100,000. The rate for women was higher – 2.0 per 100,000 per year – than men, which was just 0.6. The median age at diagnosis was 61 (source). For more information, also check out this blog post I made: "Do I have rosacea or erythromelalgia?"
Treatment
Like with rosacea, each case seems to react differently to treatment options. Traditional over-the-counter pain medications or stronger prescription drugs help some. NSAID's and blood vessel constricting medication might help. Anticonvulsant drugs like Neurontin and Lyrica help others. Certain antidepressants like Cymbalta and paroxetine might help. Combinations of drugs also have been reported effective. For instance, Lyrica and Cymbalta, at the lowest possible dosage, have been reported to be more effective than either drug by itself. It is recommended that people with EM find a doctor willing to help them pursue a trial-and-error course of treatment
EM or Raynaud's phenomenon?
Raynaud's syndrome also gives red and flushed extremities (hands and feet typically). It is characterized by excessively reduced blood flow in response to cold or emotional stress, causing discoloration of the fingers, toes, and occasionally other areas. They can also swell a bit and start to throb or itch even. It can cause the fingers and feet to become pale, white and cold (usually when you are exposed to cold temperatures and the blood flow doesn't read the hands and feet), or for them to become purple (when oxygen supply is depleted) or red and hot (when the blood supply is up to normal again). Raynaud's and EM can go together sometimes. EM seems to give much more pain than Raynaud's and the discolorations and blood vessel constriction of toes and hands from Raynaud's tend to last a lot longer at a time, compared to the short EM attacks. However, some EM patients report attacks lasting from one hour to a few weeks even. Both can be triggered by cold and heat but EM can flare without any obvious trigger at play. People with EM complaint about random attacks, very red and swollen extremities which can feel like skin burns, yet also itch at times (probably due to the skin swelling and the nerves getting stimulated or trapped I can imagine). It prevents some patients even from working and sleeping and one patient details how she sometimes has to try to sleep with her hands raised in the air, in search of some relief (source). Read more on Raynaud's here.
Tests that you can ask for are
An ANA test - please ask him to specify that it be done by IFA methodology.
An ENA panel (includes SCL-70, and anti-RNP)
Anticentromere B test
nailfold capillaroscopy (source).
EM lies within the field of 3 different medical specialisms, hematology, neurology and vascular diseases, which makes it even harder to treat, as very few specialist seems to master all of those 3 fields. You can read more on EM here. And here.
What does erythromelalgia (EM) look like?
 Erythromelalgia can look a lot like subtype 1 rosacea
Erythromelalgia can look a lot like subtype 1 rosaceaEspecially as in rare cases, erythromelalgia only manifests itself as redness and flushing and burning of the face (so not on the hands and feet as well). With erythromelalgia, flushing usually affects the hands and feet, but the face can also be involved. In this medical report, the case of a young woman in discussed, who was hospitalized with the exact same symptoms as I have (with as it stands for now the diagnosis rosacea): "Erythermalgia is a rare cutaneous disorder characterized by attacking of erythema (skin redness), pain and increased temperature, which primarily involves the extremities and may infrequently extend to the neck, face, ears and even the scrotum. We reported an 18-year-old woman who presented with 3 years history of sole involvement of attacking erythema, pain and warmth over her face and ears without any other associations. The frequency and severity of the flares progressed gradually during the course. Cutaneous examination revealed erythema, increased temperature and tenderness on the face and ears during the flare. The symptoms could be relieved rapidly by cooling. Dermatoscope showed that vessels inside the erythema were more dilated during the episode than after application of ice. The lesion is considered a rare variant of erythermalgia with sole involvement of face and ears. The symptoms had mild response to oral antihistamines, topical steroids and tacrolimus, but had excellent response to the combinative therapy of aspirin and paroxetine. A few kinds of cutaneous diseases present as attacking facial erythema associated with pain and increased temperature, which mainly include erythermalgia (EM) and red ear syndrome (RES). - Read the full report here.
Forum posts from rosacea patients about erythromelalgia (EM)
KRC wrote on May 4th 2014: "I am beginning to suspect that I might have something of this nature (EM)
as in addition to horrific facial burning I appear to also have burn
on my lower legs! The only confusing thing is I also get some of the
minor breakouts associated w. rosacea. I am under a little bit of
stress as life tends to do and am wondering if a plain old tranquilizer
might help me - So many avenues to pursue. I wish the medical community
were a little better educated to all of this. As it is with so many
symptoms I feel like they just think I am nuts. And any mention of
demodex makes them really squirm lol. It is classic as so many on the
board have elaborated."
Meg replied: "You are welcome. May I suggest you take a look the the EM site -www.erythromelalgia.org and if you want to discuss with others who have the same symptoms, join the following support group.
I think you will find that many people with EM have both rosacea and
Face EM, depending on the severity. If your legs are burning, along
with your face, you probably have EM. It is primary EM is there is no
other cause, but if you have something causing these symptoms, then it's
seen as secondary. For instance EM can be caused by peripheral
neuropathy, diabetes, lupus, etc,... EM is really a set of symptoms
which are essentially red, hot, burning skin that is often relieved with
cooling, etc... More details on the first site listed above. Also,
feel free to email me directly if I can be of further help."
GracieTiger wrote on December 19th 2008: "I need help understanding this - visit with derm was NOT GOOD. Hi all - I just visited a dermatologist for the first time since I started flushing. He is recognized as a "top doc" in this city and came recommended on the rosacea site. For those of you who don't remember me, I'd like to give a brief history of my symptoms. I lived in rural Africa for a year, and about two weeks after returning, I started having a lot of unusual symptoms. The first of which was facial flushing. I had no history of flushing/blushing at all, ever. It started suddenly, and at first, it was pretty transient. More like blushing. Then it progressed to the point that I felt like my face was red and hot all the time. That feeling eventually subsided a bit, however, when that winter began I realized that I had quite a problem on my hands. When my body was cold, then became warm, I would flush really really intensely for about eight to ten hours. The burning was near unbearable. Without a doubt, every single time that I felt cold, then took a hot shower or entered a hot room, I would have a major flush. It was pretty unbelievable to me that in just a couple months I went from never flushing to major major flushing. Along with the flushing I also had a lot of other problems. Heart arrhythmias, panic attacks (no history at all), breathing problems, vision issues, joint swelling, etc etc. Eventually I was diagnosed with having a type of autonomic nervous system dysfunction - POTS..Over the summer, the flushing wasn't nearly as bad. My skin got kind of red in the summer, but I wouldn't say I flushed. No burning. Now that it is cold again however, it is unbearable flushing. My body temp during a flush will go from like 96.5 pre-flush to 99 within ten minutes of flushing. I don't know if this is rosacea or not. But it doesn't really matter what it is. It is debilitating. I used to be a zookeeper and was working really really hard to be a wildlife veterinarian. That dream is shot out the door due to flushing. I can no longer work outside. I used to be an avid winter sportswoman, now I cannot do any outdoor activities. I used to love mountain camping, but now I can't do that, ever, because it gets too cold at night to camp and I flush when it warms up in the day. So, I finally went and saw a dermatologist. After educating myself about rosacea, flushing, blood vessel damage, etc I felt like I would be a good candidate for some laser treatment. My dermatologist completely write me off. He kept saying that it's clear I don't have rosacea because I have no inflammation and because I was not red at the time I saw him. He said it is clearly an autonomic nervous system dysfunction, and that he had no idea why I thought he could help me. He completely belittled me, repeatedly asking what I thought I would get out of him. When I tried to share my knowledge of blood vessel damage from prolonged flushing and the benefits of laser in curbing that damage, he told me I sound too educated to think he could do anything for me. Again, this is the top-rated dermatologist in my area. That is fine if he feels there is nothing that can be done for me. I was not expecting a miracle cure. But to repeatedly ask me why I came to see him, that was crossing the asshole line. I tried to explain how much I have lost in my life due to this flushing and he kept telling me that my other issues (heart problems, etc) are the ones I should be concerned about. Yes, I agree, and I do worry about those too, but the psychological impact that the flushing has had on my life is far greater than the other issues. What killed me the most was when my doctor said he would never want rosacea, so I should be glad I don't have it. Whatever the name of what I have is, flushing is flushing!!
 Plus, if he would never want rosacea, then how dare he question me as to why I am visiting him for assistance. Obviously the flushing is pretty darn damaging to me too. I don't know how much longer I can go on with this flushing with no treatment at all. None of my docs knew however if the flushing could be explained by the POTS or if it was rosacea. The propranolol helps a little, but not much. I can't even blow dry my hair and straighten it anymore. I look like a crazed mountain woman. Haha, not really, but I would love to be able to straighten my hair once in a while without knowing that I will be red and burning for ten hours. So I am really venting my frustrations, because I am really really frustrated right now, but also hoping you all can help me. Given that I flush, and have been intensely flushing for about two years for hours at a time, am I really not a candidate for laser? Even if I don't have rosacea? Let's say that the autonomic dysfunction is causing all my problems, can't flushing alone be reason for laser? Wouldn't blocking the newly formed or damaged blood vessels help stop the burning, at least? The derm also pointed out that flushing can become rosacea eventually. So don't I want to treat it early to prevent it from crossing that point? And how does he know it hasn't already? Just because I don't have bumps? I didn't think that was a criteria for rosacea. don't many of you just have flushing?And isn't it important to treat it early? Wouldn't I want to start now in order to prevent it from ever becoming rosacea? Soooo frustrated. My doc's solution: move to southern california, Hawaii or Florida. Great, huh? Oh sure, let me just pack up my bags now!!! Thanks for listening."
Plus, if he would never want rosacea, then how dare he question me as to why I am visiting him for assistance. Obviously the flushing is pretty darn damaging to me too. I don't know how much longer I can go on with this flushing with no treatment at all. None of my docs knew however if the flushing could be explained by the POTS or if it was rosacea. The propranolol helps a little, but not much. I can't even blow dry my hair and straighten it anymore. I look like a crazed mountain woman. Haha, not really, but I would love to be able to straighten my hair once in a while without knowing that I will be red and burning for ten hours. So I am really venting my frustrations, because I am really really frustrated right now, but also hoping you all can help me. Given that I flush, and have been intensely flushing for about two years for hours at a time, am I really not a candidate for laser? Even if I don't have rosacea? Let's say that the autonomic dysfunction is causing all my problems, can't flushing alone be reason for laser? Wouldn't blocking the newly formed or damaged blood vessels help stop the burning, at least? The derm also pointed out that flushing can become rosacea eventually. So don't I want to treat it early to prevent it from crossing that point? And how does he know it hasn't already? Just because I don't have bumps? I didn't think that was a criteria for rosacea. don't many of you just have flushing?And isn't it important to treat it early? Wouldn't I want to start now in order to prevent it from ever becoming rosacea? Soooo frustrated. My doc's solution: move to southern california, Hawaii or Florida. Great, huh? Oh sure, let me just pack up my bags now!!! Thanks for listening."
Meg replied: "Sounds a lot like you do in fact have an autonomic nervous system dysfunction. I have severe and painful flushing that was diagnosed at the Mayo Clinic as a form of autonomic dysfunction. It turns out that I also stopped sweating, which is another autonomic problem. You might consider seeing the autonomic neurologists at Mayo for an accurate diagnosis. Also, I find my flushing to be more like erythromelalgia, rather than rosacea, due to the burning pain. If you have red hot burning pain when you flush, look at http://www.erythromelalgia.org/ Hope this helps. Best regards, Meg"
And also: "Erythromelalgia (EM) definitely includes the face. If you look at the EM (TEA) website, you will see they even post photos of people who have EM on their faces. Having a face only case is rare. Most people seem to have the face involved in addition to hands and feet, but some cases also involve the face or even the torso. Any part can be affected. EM is noted or defined as red, hot burning skin that is relieved by cooling. Generally, it is a form of autonomic nervous system dysfunction. GracieTiger, my flushing/EM is face only. I have no symptoms on my hands, feet or other body parts. Just my face and ears. Hope this clears things up. Meg.
PS - I have cut and pasted the info below from the EM (TEA) website (note the inclusion of the face under the "Location" paragraph). Symptoms; if you have been diagnosed with EM, symptoms may include hands or feet that are very red to purple in color, are perhaps swollen, hot to the touch, and have burning pain. Location; for some, EM symptoms may appear in the face, ears, knees or other parts of the body. The intensity of the symptoms varies from person to person. Some notice a continual burning pain while others are troubled with "flare-ups" or episodes lasting from minutes to days in length. Triggers; warm temperatures seem to be the most frequent trigger for EM episodes. Flare-ups are provoked by heat and exercise, and symptoms are relieved by cooling and elevating the affected extremities. Some TEA members have found that foods, spices like MSG, beverages (particularly alcohol) and some drugs can make EM symptoms worse.
 Plus, if he would never want rosacea, then how dare he question me as to why I am visiting him for assistance. Obviously the flushing is pretty darn damaging to me too. I don't know how much longer I can go on with this flushing with no treatment at all. None of my docs knew however if the flushing could be explained by the POTS or if it was rosacea. The propranolol helps a little, but not much. I can't even blow dry my hair and straighten it anymore. I look like a crazed mountain woman. Haha, not really, but I would love to be able to straighten my hair once in a while without knowing that I will be red and burning for ten hours. So I am really venting my frustrations, because I am really really frustrated right now, but also hoping you all can help me. Given that I flush, and have been intensely flushing for about two years for hours at a time, am I really not a candidate for laser? Even if I don't have rosacea? Let's say that the autonomic dysfunction is causing all my problems, can't flushing alone be reason for laser? Wouldn't blocking the newly formed or damaged blood vessels help stop the burning, at least? The derm also pointed out that flushing can become rosacea eventually. So don't I want to treat it early to prevent it from crossing that point? And how does he know it hasn't already? Just because I don't have bumps? I didn't think that was a criteria for rosacea. don't many of you just have flushing?And isn't it important to treat it early? Wouldn't I want to start now in order to prevent it from ever becoming rosacea? Soooo frustrated. My doc's solution: move to southern california, Hawaii or Florida. Great, huh? Oh sure, let me just pack up my bags now!!! Thanks for listening."
Plus, if he would never want rosacea, then how dare he question me as to why I am visiting him for assistance. Obviously the flushing is pretty darn damaging to me too. I don't know how much longer I can go on with this flushing with no treatment at all. None of my docs knew however if the flushing could be explained by the POTS or if it was rosacea. The propranolol helps a little, but not much. I can't even blow dry my hair and straighten it anymore. I look like a crazed mountain woman. Haha, not really, but I would love to be able to straighten my hair once in a while without knowing that I will be red and burning for ten hours. So I am really venting my frustrations, because I am really really frustrated right now, but also hoping you all can help me. Given that I flush, and have been intensely flushing for about two years for hours at a time, am I really not a candidate for laser? Even if I don't have rosacea? Let's say that the autonomic dysfunction is causing all my problems, can't flushing alone be reason for laser? Wouldn't blocking the newly formed or damaged blood vessels help stop the burning, at least? The derm also pointed out that flushing can become rosacea eventually. So don't I want to treat it early to prevent it from crossing that point? And how does he know it hasn't already? Just because I don't have bumps? I didn't think that was a criteria for rosacea. don't many of you just have flushing?And isn't it important to treat it early? Wouldn't I want to start now in order to prevent it from ever becoming rosacea? Soooo frustrated. My doc's solution: move to southern california, Hawaii or Florida. Great, huh? Oh sure, let me just pack up my bags now!!! Thanks for listening."And also: "Erythromelalgia (EM) definitely includes the face. If you look at the EM (TEA) website, you will see they even post photos of people who have EM on their faces. Having a face only case is rare. Most people seem to have the face involved in addition to hands and feet, but some cases also involve the face or even the torso. Any part can be affected. EM is noted or defined as red, hot burning skin that is relieved by cooling. Generally, it is a form of autonomic nervous system dysfunction. GracieTiger, my flushing/EM is face only. I have no symptoms on my hands, feet or other body parts. Just my face and ears. Hope this clears things up. Meg.
PS - I have cut and pasted the info below from the EM (TEA) website (note the inclusion of the face under the "Location" paragraph). Symptoms; if you have been diagnosed with EM, symptoms may include hands or feet that are very red to purple in color, are perhaps swollen, hot to the touch, and have burning pain. Location; for some, EM symptoms may appear in the face, ears, knees or other parts of the body. The intensity of the symptoms varies from person to person. Some notice a continual burning pain while others are troubled with "flare-ups" or episodes lasting from minutes to days in length. Triggers; warm temperatures seem to be the most frequent trigger for EM episodes. Flare-ups are provoked by heat and exercise, and symptoms are relieved by cooling and elevating the affected extremities. Some TEA members have found that foods, spices like MSG, beverages (particularly alcohol) and some drugs can make EM symptoms worse.
Keratosis pilaris (KP, also follicular keratosis, lichen pilaris) is a common genetic follicular condition, that produces rough, slightly red bumps on the skin. It most often appears on the arms, but can also occur on the thighs, hands, and tops of legs, sides, buttocks, or on any body part except for the palms of the hands or the soles of the feet. Often the lesions will appear on the face, which may be mistaken for acne. Keratosis pilaris results in small bumps on the skin that feel like rough sandpaper. They are skin-colored bumps the size of a grain of sand, many of which are surrounded by a slight pink color. They are seldom sore or itchy. They occur when the human body produces excess keratin, a natural protein in the skin which is cream colored. It surrounds and entraps the hair follicles in the pore. This causes the formation of hard plugs. Doctors can often diagnose keratosis pilaris simply by examining the skin; tests are usually not needed. According to wiki, KP affects worldwide an estimated 40-50% of the adult population and approximately 50-80% of all adolescents. It is more common in women than in men, and is often present in otherwise healthy individuals. The skin condition is prevalent in persons of all races. No particular race is at higher risk for contracting keratosis pilaris. Although keratosis pilaris may manifest in persons of any age, it usually appears within the first decade of life and is more common in young children. In most cases, the condition gradually improves before age 30, however it can persist longer. There are several different types of keratosis pilaris, including keratosis pilaris rubra (red, inflamed bumps which can be on arms, head, legs), keratosis pilaris alba (rough, bumpy skin with no irritation), keratosis pilaris rubra faceii (reddish rash on the cheeks), and related disorders. Because of the resemblance with rosacea, I will focus on this last subtype.
Treatment
Wiki
states that keratosis pilaris is harmless and that medical treatment is
not necessary. Many patients do however look for treatment because of
the cosmetic appearance of KP. Topical creams and lotions are currently
the most commonly used treatment for keratosis pilaris, specifically
those consisting of moisturizing or keratolytic treatments, including:
urea, lactic acid, glycolic acid, salicylic acid, tretinoin, Vitamin D,
or topical retinoids. Steroid creams can
also be used to reduce redness. However, the effectiveness of these
treatments is limited and research to discover more effective treatments
is ongoing. Improvement of the skin often takes months and the bumps
are likely to return. Taking long hot baths followed by exfoliating the affected areas with a coarse washcloth or
stiff brush may help unplug pores and therefore can also be used as a
treatment method. Some cases of keratosis pilaris have been successfully
treated with laser therapy, which involves passing intense bursts of
light into targeted areas of the skin. Depending on the body's response
to the treatment, multiple sessions over the course of a few months may
be necessary. Note that most of these treatments can be detrimental to underlying rosacea, in case you suffer from both conditions. Steroid creams are not recommended when you have rosacea and long hot baths neither. Some of the suggested creams here can worsen rosacea as well.
This blogger with KP suggests for treatment: "For the majority of cases of Keratosis Pilaris, one can use moisturizers along with basic lubes that can be bought which are non-prescription such as Cetaphil and also Lubriderm and lactic acid lotions for instance AmLactin and Lac-Hydrin. Your affected area ought to be washed that has a mild moisturising soap or even facial bathe twice a day. By no means use unpleasant ingredients that can dry up your skin layer since this is only able to worsen the problem. Your skin specialist may also prescribe creams using alpha hydroxy acids, vitamin A lotions and immunomodulators. Even though not that effective in completely smoothing out Keratosis Pilaris, you can also use gentle exfoliant soaps and also facial scrubs to improve the disorder of the skin."
This blogger with KP suggests for treatment: "For the majority of cases of Keratosis Pilaris, one can use moisturizers along with basic lubes that can be bought which are non-prescription such as Cetaphil and also Lubriderm and lactic acid lotions for instance AmLactin and Lac-Hydrin. Your affected area ought to be washed that has a mild moisturising soap or even facial bathe twice a day. By no means use unpleasant ingredients that can dry up your skin layer since this is only able to worsen the problem. Your skin specialist may also prescribe creams using alpha hydroxy acids, vitamin A lotions and immunomodulators. Even though not that effective in completely smoothing out Keratosis Pilaris, you can also use gentle exfoliant soaps and also facial scrubs to improve the disorder of the skin."
KP or rosacea?
People with keratosis pilaris rubra faceii
can have very red faces. The excess Keratin that KP patients have, aggravates the blood vessels in the cheeks and causes them to be more
visible on the surface. People with fair skin are more likely to
suffer with this as it would be harder to see the blood vessels with
people with darker skin. It can be very difficult to distinguish these
red cheeks from rosacea. Especially when you read that KP is so common
and widespread. I can hardly believe to be honest that about 60 to 80%
of youth are afflicted with this condition, whereas just 40 per cent of grownups
manifest some degree of the condition (source).
Wiki estimates these percentage even higher as you could just read. I
doubt these massive numbers of people have the facial version keratosis pilaris rubra
faceii. The chicken skin texture on arms or legs may be the more widespread variant I suspect. So small red bumps on their arms and legs. But when the face is involved, this KPRF is a lot more rare than regular KP. On this forum a member writes: "As keratin disorders affecting the face are rarer than rosacea, it would be good to see a derm who is familiar with these to rule out KPRF or KPAF."
 Keratosis pilaris rubra faceii (KPRF) is often misdiagnosed as rosacea (source), since it primarily affects the face and makes the cheeks also red and ruddy looking. However, KP can be accompanied by itching in the affected area, whereas rosacea rarely itches, and often burns
instead. Also, KP not only gives a bright rosy color, but this color can
be very clearly marked from normal looking skin (and rosacea rarely has
such a clear cut division line). And KPRF can also look very smoothly red/rosy colored, whereas rosacea rarely is as evenly red or pink (but again, there are
exceptions for all this). KP can come with the typical KP bumps.
However, to make matters more difficult: KPRF doesn't even have to have
the chicken skin feel of normal KP. Also people who have Rubra Faceii
usually also have a small bit of Keratosis Pilaris on other body parts,
like the backs of their upper arms (however as 1/2 population has KP
this is probably not that great a test). Another difference is that rosacea usually can also affect your nose, the sides of your nose, your chi, your ears and/or your forehead (this can come gradually. I started of with
only redness in the cheek area but by now, 15 years later, my chin and
nose are also getting a lot more red). Rubra Faceii however just affects the cheeks,
the area just under the nose and just under the eyes. In addition, as
written before, rosacea usually is quite blotchy while Rubra Faceii gives a much more even red skin tone (source). People with KPRF do blush and flush easily, something they share with a lot of rosacea patients. Also KPRF does not affect the eyes, unlike rosacea (often causing ocular rosacea; dry, gritty, painful eyes). KPRF can also hit at a young age, whereas rosacea usually starts after age 18. Some derms still say rosacea only affects people in their 30's, but
this is most definitely incorrect. Mine started age 19 and I know a lot
of people from forums who had rosacea from their 20's, but I only heard
of people getting affected with it as early as puberty (seldomly) and
onwards. KP seems to start in kids already, and is common during puberty. Some other KPRF indications are a paler patch right in the middle of
the cheek redness area, or roughness or pitted areas (small depressions)
in the redness, around the hair follicles on the cheek. Both KP
and rosacea can run in families, so if any of your family members have
one or the other, this can be another indication of which of the two you
might have when you are dealing with these symptoms that can be both KP
or rosacea.
Keratosis pilaris rubra faceii (KPRF) is often misdiagnosed as rosacea (source), since it primarily affects the face and makes the cheeks also red and ruddy looking. However, KP can be accompanied by itching in the affected area, whereas rosacea rarely itches, and often burns
instead. Also, KP not only gives a bright rosy color, but this color can
be very clearly marked from normal looking skin (and rosacea rarely has
such a clear cut division line). And KPRF can also look very smoothly red/rosy colored, whereas rosacea rarely is as evenly red or pink (but again, there are
exceptions for all this). KP can come with the typical KP bumps.
However, to make matters more difficult: KPRF doesn't even have to have
the chicken skin feel of normal KP. Also people who have Rubra Faceii
usually also have a small bit of Keratosis Pilaris on other body parts,
like the backs of their upper arms (however as 1/2 population has KP
this is probably not that great a test). Another difference is that rosacea usually can also affect your nose, the sides of your nose, your chi, your ears and/or your forehead (this can come gradually. I started of with
only redness in the cheek area but by now, 15 years later, my chin and
nose are also getting a lot more red). Rubra Faceii however just affects the cheeks,
the area just under the nose and just under the eyes. In addition, as
written before, rosacea usually is quite blotchy while Rubra Faceii gives a much more even red skin tone (source). People with KPRF do blush and flush easily, something they share with a lot of rosacea patients. Also KPRF does not affect the eyes, unlike rosacea (often causing ocular rosacea; dry, gritty, painful eyes). KPRF can also hit at a young age, whereas rosacea usually starts after age 18. Some derms still say rosacea only affects people in their 30's, but
this is most definitely incorrect. Mine started age 19 and I know a lot
of people from forums who had rosacea from their 20's, but I only heard
of people getting affected with it as early as puberty (seldomly) and
onwards. KP seems to start in kids already, and is common during puberty. Some other KPRF indications are a paler patch right in the middle of
the cheek redness area, or roughness or pitted areas (small depressions)
in the redness, around the hair follicles on the cheek. Both KP
and rosacea can run in families, so if any of your family members have
one or the other, this can be another indication of which of the two you
might have when you are dealing with these symptoms that can be both KP
or rosacea.
 Keratosis pilaris rubra faceii (KPRF) is often misdiagnosed as rosacea (source), since it primarily affects the face and makes the cheeks also red and ruddy looking. However, KP can be accompanied by itching in the affected area, whereas rosacea rarely itches, and often burns
instead. Also, KP not only gives a bright rosy color, but this color can
be very clearly marked from normal looking skin (and rosacea rarely has
such a clear cut division line). And KPRF can also look very smoothly red/rosy colored, whereas rosacea rarely is as evenly red or pink (but again, there are
exceptions for all this). KP can come with the typical KP bumps.
However, to make matters more difficult: KPRF doesn't even have to have
the chicken skin feel of normal KP. Also people who have Rubra Faceii
usually also have a small bit of Keratosis Pilaris on other body parts,
like the backs of their upper arms (however as 1/2 population has KP
this is probably not that great a test). Another difference is that rosacea usually can also affect your nose, the sides of your nose, your chi, your ears and/or your forehead (this can come gradually. I started of with
only redness in the cheek area but by now, 15 years later, my chin and
nose are also getting a lot more red). Rubra Faceii however just affects the cheeks,
the area just under the nose and just under the eyes. In addition, as
written before, rosacea usually is quite blotchy while Rubra Faceii gives a much more even red skin tone (source). People with KPRF do blush and flush easily, something they share with a lot of rosacea patients. Also KPRF does not affect the eyes, unlike rosacea (often causing ocular rosacea; dry, gritty, painful eyes). KPRF can also hit at a young age, whereas rosacea usually starts after age 18. Some derms still say rosacea only affects people in their 30's, but
this is most definitely incorrect. Mine started age 19 and I know a lot
of people from forums who had rosacea from their 20's, but I only heard
of people getting affected with it as early as puberty (seldomly) and
onwards. KP seems to start in kids already, and is common during puberty. Some other KPRF indications are a paler patch right in the middle of
the cheek redness area, or roughness or pitted areas (small depressions)
in the redness, around the hair follicles on the cheek. Both KP
and rosacea can run in families, so if any of your family members have
one or the other, this can be another indication of which of the two you
might have when you are dealing with these symptoms that can be both KP
or rosacea.
Keratosis pilaris rubra faceii (KPRF) is often misdiagnosed as rosacea (source), since it primarily affects the face and makes the cheeks also red and ruddy looking. However, KP can be accompanied by itching in the affected area, whereas rosacea rarely itches, and often burns
instead. Also, KP not only gives a bright rosy color, but this color can
be very clearly marked from normal looking skin (and rosacea rarely has
such a clear cut division line). And KPRF can also look very smoothly red/rosy colored, whereas rosacea rarely is as evenly red or pink (but again, there are
exceptions for all this). KP can come with the typical KP bumps.
However, to make matters more difficult: KPRF doesn't even have to have
the chicken skin feel of normal KP. Also people who have Rubra Faceii
usually also have a small bit of Keratosis Pilaris on other body parts,
like the backs of their upper arms (however as 1/2 population has KP
this is probably not that great a test). Another difference is that rosacea usually can also affect your nose, the sides of your nose, your chi, your ears and/or your forehead (this can come gradually. I started of with
only redness in the cheek area but by now, 15 years later, my chin and
nose are also getting a lot more red). Rubra Faceii however just affects the cheeks,
the area just under the nose and just under the eyes. In addition, as
written before, rosacea usually is quite blotchy while Rubra Faceii gives a much more even red skin tone (source). People with KPRF do blush and flush easily, something they share with a lot of rosacea patients. Also KPRF does not affect the eyes, unlike rosacea (often causing ocular rosacea; dry, gritty, painful eyes). KPRF can also hit at a young age, whereas rosacea usually starts after age 18. Some derms still say rosacea only affects people in their 30's, but
this is most definitely incorrect. Mine started age 19 and I know a lot
of people from forums who had rosacea from their 20's, but I only heard
of people getting affected with it as early as puberty (seldomly) and
onwards. KP seems to start in kids already, and is common during puberty. Some other KPRF indications are a paler patch right in the middle of
the cheek redness area, or roughness or pitted areas (small depressions)
in the redness, around the hair follicles on the cheek. Both KP
and rosacea can run in families, so if any of your family members have
one or the other, this can be another indication of which of the two you
might have when you are dealing with these symptoms that can be both KP
or rosacea.What does KPRF look like?
Infection with Helicobacter pylori (H. pylori) is the cause of most stomach and duodenal ulcers. It is a bacterium (germ) that can infect the lining of the stomach and duodenum. It is a common infection, although it is getting less common as time goes by. More than a quarter of people in the UK for instance become infected with H. pylori at some stage in their life. Once you are infected, unless treated, the infection usually stays for the rest of your life. Commonly there are no problems when you are infected. Most people who are infected with H. pylori have no symptoms or problems caused by the infection. These people do not know that they are infected. A number of H. pylori bacteria may just live harmlessly in the lining of the stomach and duodenum. When it does cause symptoms, H. pylori also causes some cases of non-ulcer dyspepsia. You can read more about that here. Infection with H. pylori can be confirmed by a test done on a sample of faeces (stools), or in a breath test, or from a blood test, or from a biopsy sample taken during an endoscopy. A one-week course of two antibiotics plus an acid-suppressing medicine will usually clear the H. pylori infection. This should prevent the return of a duodenal or stomach ulcer that had been caused by this infection.
Reasons for testing on H. Pylori
If you have recurring dyspepsia (recurring indigestion symptoms). When you have a duodenal or stomach ulcer. When you have a first-degree relative (mother, father, brother, sister or child) who has been diagnosed with stomach cancer. When you are taking long-term anti-inflammatory medication such as ibuprofen, diclofenac, aspirin, etc. The combination of these medicines and H. pylori increases the risk of developing a stomach ulcer. When you have atrophic gastritis (inflammation of the stomach lining).
If you have recurring dyspepsia (recurring indigestion symptoms). When you have a duodenal or stomach ulcer. When you have a first-degree relative (mother, father, brother, sister or child) who has been diagnosed with stomach cancer. When you are taking long-term anti-inflammatory medication such as ibuprofen, diclofenac, aspirin, etc. The combination of these medicines and H. pylori increases the risk of developing a stomach ulcer. When you have atrophic gastritis (inflammation of the stomach lining).
Is there a relation between H. Pylori and rosacea?
In this Pubmed article
a group of rosacea patients was tested on H pylori presence in the
stomach and oral cavity, as well as a test group without rosacea/skin
conditions. Both had dyspeptic symptoms (some burning in the stomach
area I assume). A stunning 88% of the rosacea patients group had H. Pylori, compared to 65% in the control group. "A
noticeable number of rosacea patients showed chronic active gastritis
predominantly in antrum but also in the corpus while those with NUD
showed only mild gastritis confined to the antrum only." The
rosacea patients received antibiotic treatment (omeprazole (2 x 30 mg),
clarithromycin (2 x 500 mg) and metronidazole (2 x 500 mg), plus
gargling and application of metronidazole paste in the case of Hp oral
cavity infection. Afterwards, H. Pylori was eradicated from the stomach
in 97% and from the oral cavity in 73% of treated patients. Within 2-4 weeks, the symptoms of rosacea disappeared or decreased markedly in 51 subjects. The scientists concluded that rosacea is a disorder with various gastrointestinal symptoms closely related to gastritis. That eradication of H. Pylori leads to improvement of symptoms of rosacea and reduction in related gastrointestinal symptoms. And that if rosacea symptoms didn't clear after treatment, this could be because there was still H. Pylori bacteria lingering in the oral cavity. "Rosacea could be considered as one of the extragastric symptoms of Hp infection probably mediated by Hp-related cytotoxins and cytokines."
"There is often an association with hyperacidity/stomach ulcers and rosacea and this led to the theory that Helicobacter was a cause of rosacea - treatment of helicobacter is with combination antibiotics and this obviously settles inflammatory rosacea but not flushing and it recurs when the antibiotics are withdrawn. Possible the stress of the stomach problems is exacerbating the rosacea and absorption of the drugs could be a problem. Would suggest trying omeproazole - need at least 20mg/day and possibly twice daily to settle the stomach .You can buy omeprazole at the chemist but quite expensive. Also possibly antibiotics to eradicate the helicobacter."

Carcinoid syndrome describes the flushing that comes from having carcinoid tumors. A form of cancer. Symptoms are redness of the face, hot skin, a pellagra-like syndrome with purplish areas of spider like veins on the nose and upper lip, chronic diarrhea, a rapid heartbeat and difficulty breathing. The skin flushing from carcinoid syndrome is caused by secretion of mainly serotonin and kallikrein from within the tumor. It is not the serotonin that produces this blood vessel dilation (and therefore the flushing) -also called vasoactive substance-, but it is the secretion of kallikrein. Kallikrein is the enzyme that catalyzes the conversion of kininogen to lysyl-bradykinin. The latter is further converted to bradykinin, one of the most powerful vasodilators known. Carcinoid syndrome occurs in approximately 5% to 10% of carcinoid tumors. By the time the symptoms of carcinoid syndrome appear, the tumor has often already spread. This makes it important to diagnose the tumors and carcinoid syndrome as early as possible. When I went to my doctor to ask for treatment of my face flushing, she sent me to hospital first to undergo a large amount of tests, including testing for carcinoid tumors.
The most common symptoms of carcinoid syndrome
Diarrhea,
flushing of the skin of the face and chest, heart palpitations, stomach cramps,
shortness of breath, wheezing. Note that having a carcinoid tumor can
give a lot of different symptoms on top. Please read here for more info on that.
The
facial (and sometimes chest and neck) flushing of
carcinoid syndrome is usually a dry flushing, and not associated with
sweating like some other kinds of flushing. The flushing is often a symptom
that others first notice. Patients may not feel it themselves in the beginning.
These flushing symptoms may be worsened by stress, physical exertion, or by drinking
alcohol. Eating certain foods, such as aged cheese like cheddar or
stilton cheese, salted or pickled meats, or other foods that contain
tyramine may also trigger symptoms (source), (source). Basically just like with rosacea flushing.
The character of carcinoid syndrome flushing differs
The character of carcinoid syndrome flushing differs
depending on the location where the tumor started. Tumors of the foregut (stomach, lung, pancreas) are associated with a
bright red flush, with quite specifically showing small red area's
cluttering together, almost appearing like the different countries and
continents on a geographical map. These flushes continue for quite a
long time and are accompanied by wheezing, sweating and a sensation of skin burning. The flushing seen with foregut carcinoids is caused by the
release of
histamine. In ileal tumors, the flush is patchier and going towards purple in color, intermingled with
areas of paler skin, and this type of flushing episode does not last as long. Flushing seen with ileal carcinoids cannot be explained
solely by the production of serotonin. Foregut
carcinoids do not generally secrete serotonin but, instead its
precursor, 5-hydroxytryptamine. Screening should therefore seek this
product if the other metabolites are not elevated.
Other mediators that have been proposed include prostaglandins and tachykinins. Tachykinins are believed to be mediators of the flushing in
tumors of the midgut. They cause vasodilation and contraction of
various types of smooth muscle. These peptides include substance P,
substance K, and neuropeptide K. Both types of flushing can also cause swelling of the face, which may persist and lead to telangiectasia and even facial rosacea.
Table 1 Classification of Carcinoid Tumors According to Site of Primary Tumor
| Site | Biochemistry | Clinical Picture |
|---|---|---|
| Foregut bronchi, stomach, first part duodenum | 5-Hydroxytryptophan, adrenocorticotropin, growth hormone, gastrin, growth hormone releasing hormone | Protracted, purplish or violaceous flush, manifestation of other ectopic hormone secretion |
| Midgut second part of duodenum, jejunum, ileum, ascending colon | Serotonin, kinins, neuropeptides, prostaglandins | Pink-red flush |
Hindgut transverse, descending colon and rectum |
None | Only local symptoms |
The
most useful initial test is a urine test, which measures the 24 hour urine levels of 5-HIAA
(5-hydroxyindoleacetic acid), the end product of serotonin metabolism.
Patients with carcinoid syndrome usually excrete more than 25 mg of
5-HIAA per day. For diagnosing tumors and tumor metastasis, you have to
undergo a special scan, called a scintigraphy. Here doctors will inject you with a low radioactive substance and then make scans in the scintigraphy machine. Clinical diagnosis of carcinoid syndrome is not considered difficult in patients with flushing
episodes associated with systemic symptoms (e.g., diarrhea, wheezing,
weight loss) and hepatomegaly. It is more difficult in patients who have
occasional flushing and no associated symptoms. Sometimes doctors try to provoke a flush, when in doubt, by asking the patient to drink alcohol (4 mL of 45% ethanol) or through the infusion of 6 µg noradrenaline, an effect
that can be blocked by phentolamine (5-15 mg IV). Calcium gluconate, 10
to 15 mg/kg, administered IV over 4 hours, may also produce a flush mimicking
a spontaneous attack. Epinephrine (adrenaline) reverses flushing in patients with mastocytosis but provokes flushing in patients with the carcinoid syndrome. For more information, see this link.
Distinguishing rosacea from carcinoid syndrome
Both rosacea and carcinoid syndrome can cause facial flushing. Both types of flushing can appear very similar, affecting the same areas in the face and to make matters more complex, is that both types of flushing are triggered by similar factors: heat, stress, exercise and the same list of foods, including foods high in histamine like tomatoes, chocolate, cheese, as well as alcohol and spices. In this blog, a woman with carcinoid syndrome tells about her flushing.
Both rosacea and carcinoid syndrome can cause facial flushing. Both types of flushing can appear very similar, affecting the same areas in the face and to make matters more complex, is that both types of flushing are triggered by similar factors: heat, stress, exercise and the same list of foods, including foods high in histamine like tomatoes, chocolate, cheese, as well as alcohol and spices. In this blog, a woman with carcinoid syndrome tells about her flushing.
What does carcinoid syndrome flushing look like?
LesleyC wrote on May 18th 2012: "Yes, I was tested about a year back for carcinoid syndrome. This was done by performing a 24 hour urine sample, it was an easy test to perform. My internist requested for the test because at the time, I had other symptoms besides flushing, and he wanted to rule out carcinoid tumors and adrenal gland tumors (pheochromocytoma) as well."
Anathema wrote on April 22nd 2014: "Rosacea vs Carcinoid syndrome what is the difference? Basically my question is how is rosacea flush different from a carcinoid syndrome flush? Also should every flusher get tested for this disease? If anyone has done some research on this would be nice to hear. Thanks"
Anathema wrote on April 22nd 2014: "Rosacea vs Carcinoid syndrome what is the difference? Basically my question is how is rosacea flush different from a carcinoid syndrome flush? Also should every flusher get tested for this disease? If anyone has done some research on this would be nice to hear. Thanks"
Wicksyx replied on April 22nd 2014: "I was tested for the carcinoid syndrome with a 24hr urine test because of my flushing, the main symptom of the tumour (some carcinoid tumors
have no symptoms at all) is diarrhoea and abdominal pain which I also
was dealing with at that time. My dermatologist told me that if you
suffer from the tumour you can also develop Rosacea from flushing so
much and from the dilated blood vessels. Luckily my tests were all clear and I
didn't have it, but now I am still left curious about what causes my
flushing. [..] But yes every flusher should be tested for this disease, definitely."
Anathema replied: "Thanks for all the information Wicksy, I am going to get that test done right away, since I am have bunch of symptoms. And do you know if the carcinoid flush is different than a rosacea flush?"
Anathema replied: "Thanks for all the information Wicksy, I am going to get that test done right away, since I am have bunch of symptoms. And do you know if the carcinoid flush is different than a rosacea flush?"
Wicksyx replied: "There is no difference! I suffer from very severe burning pain and my derm said that there was no difference between Rosacea flush and carcinoid one because all the triggers are the same. I'm glad your going
for the test and hope you get good results!!"
Graemeb wrote on March 9th 2014: "Hi my name is Graeme. I have been suffering from facial flushing for around
7 months. The redness is across my nose, around my eyes, and on my
forehead. The redness is itchy and is usually worse after a shower. I
can't even wash my face with soap anymore through fear of burning.
Anyway I was tested for carcinoid syndrome which terrified me. Nothing
came up with that, so the drs believe I have rosacea. I have been putting
cream called metronidazole on my face which has helped a little. I have
now been given tetralysal (lymecycline) to take on a daily basis, which I have been
taking for a week. They don't seem to be helping."
J-MIll wrote on March 28th 2008: "I think when people first flare with Rosacea, they are stressed out. The
stress tends to cause all sorts of weird symptoms that the disease
process does not explain. Doctors start looking for zebras instead of
treating horses, to use medical lingo. When I first flared I was stressed and I developed brutal GI distress,
lost 25 pounds in 2 months, etc. They were checking for lupus,
carcinoid (btw it is not 100% fatal, I actually know someone who has
carcinoid and they live a very normal comfortable life but take beta
blockers, it is only 100% fatal if it moves to your liver, but seldom
happens), etc. When I managed to get my skin under some control and my stress levels
decreased, the GI distress went away and the weight came back on, all of
a sudden I just had Rosacea (w/Seb Derm just to be safe)."
Mistica wrote on January 19th 2012: "I have been tested several times for increased levels of serotonin and
catecholamines as part of the screening for carcinoid syndrome. This
syndrome occurs when certain tumours (normally in the gut) release
these hormones. They are vasodilative. I have always tested negative,
and really don't think I have any type of cancer."
 Polycythemia vera
Polycythemia vera
 Polycythemia vera
Polycythemia veraPolycythemia vera (PV) is a type of blood cancer in which the bone marrow makes too many red blood cells. It may also result in the overproduction of white blood cells and platelets. It is a slow-growing type of blood cancer. Polycythemia vera isn't common. It usually develops slowly, and you may have it for years without noticing signs or symptoms. Often, polycythemia vera is found during a blood test done for some other reason.Without treatment, polycythemia vera can be life-threatening. However, with proper medical care, many people experience few problems related to this disease. Over time, there's a risk of progressing to more-serious blood cancers, such as myelofibrosis or acute leukemia. PV is more common in the elderly and may be symptomatic or asymptomatic. Common signs and symptoms include itching (pruritus) especially after a warm bath or shower, and severe burning pain in the hands or feet that is usually accompanied by a reddish or bluish coloration of the skin. This stems from circulation problems in the small blood vessels, which can cause erythromelalgia and severe pains in hands, feet, toes or fingers. Symptoms may also include a flushed red face (facial plethora), high blood pressure (hypertension), and an enlargement of the spleen (splenomegaly). PV can also cause headaches, dizziness, vision problems, excessive sweating and shortness of breath. Patients with polycythemia vera are more likely to have arthritis. Treatment consists primarily of phlebotomy (source) and (source).
 Diagnosis
DiagnosisDoctors most frequently use blood tests to diagnose polycythemia vera. If you have polycythemia vera, blood tests may reveal: An increase in the number of red blood cells and, in some cases, an increase in platelets or white blood cells. Elevated hematocrit measurement, the percentage of red blood cells that make up total blood volume.Elevated levels of hemoglobin, the iron-rich protein in red blood cells that carries oxygen. Very low levels of erythropoietin, a hormone that stimulates bone marrow to produce new red blood cells. If your doctor suspects you have polycythemia vera, he or she may recommend a bone marrow aspiration or biopsy to collect a sample of your bone marrow. Read more here.
Treatment of PV
 The goal of treatment is to reduce the thickness of the blood and prevent bleeding and clotting. A method called phlebotomy is used to decrease blood thickness. One unit of blood (about 1 pint) is removed weekly until the hematocrit level is less than 45 (males) or 42 (females). Then therapy is continued as needed. Occasionally, chemotherapy (specifically hydroxyurea) may be given to reduce the number of red blood cells made by the bone marrow. Interferon may also be given to lower blood counts. A medicine called anagrelide may be given to lower platelet counts. Some patients are advised to take aspirin to reduce the risk of blood clots, though it increases the risk for stomach bleeding. Ultraviolet-B light therapy can reduce the severe itching some patients experience. Read more about treatments here. And also on this forum.
The goal of treatment is to reduce the thickness of the blood and prevent bleeding and clotting. A method called phlebotomy is used to decrease blood thickness. One unit of blood (about 1 pint) is removed weekly until the hematocrit level is less than 45 (males) or 42 (females). Then therapy is continued as needed. Occasionally, chemotherapy (specifically hydroxyurea) may be given to reduce the number of red blood cells made by the bone marrow. Interferon may also be given to lower blood counts. A medicine called anagrelide may be given to lower platelet counts. Some patients are advised to take aspirin to reduce the risk of blood clots, though it increases the risk for stomach bleeding. Ultraviolet-B light therapy can reduce the severe itching some patients experience. Read more about treatments here. And also on this forum.What does Polycythemia vera look like?
 Mixed connective tissue disease
Mixed connective tissue disease
Mixed connective tissue disease has signs and symptoms of a combination of disorders — primarily of lupus, scleroderma and polymyositis. For this reason, mixed connective tissue disease is sometimes referred to as an overlap disease. In mixed connective tissue disease, the symptoms of the separate diseases usually don't appear all at once. Instead, they tend to occur in sequence over a number of years, which can make diagnosis more complicated. Early signs and symptoms often involve the hands. Fingers may swell up like sausages, and the fingertips might turn white and become numb. In later stages, some organs — such as the lungs, heart and kidneys — may be affected. Mixed connective tissue disease occurs most commonly in young women. Treatment often includes drugs such as prednisone (source). The connective tissues are the structural portions of our body that essentially hold the cells of the body together. These tissues form a framework or matrix for the body. The connective tissues are composed of two major structural molecules, collagen and elastin. There are many different collagen proteins that vary in amount in each tissue of the body. Elastin is another protein that has the capability of stretching and returning to original length like a spring. Elastin is the major component of ligaments (tissues which attach bone to bone). Connective tissue diseases are disorders featuring abnormalities involving the collagen and elastin. Connective tissue diseases are often characterized by a variety of immune abnormalities that are common for each particular type of illness (source). Your doctor may suspect mixed connective tissue disease based on your signs and symptoms. A physical exam may reveal signs such as swollen hands and painful, swollen joints. A blood test can determine whether you have a certain antibody in your blood that indicates mixed connective tissue disease. Doctors will look for a positive, speckled anti-nuclear antibody and anti-U1-RNP antibody.
Symptoms
 Early indications of mixed connective tissue disease may include:
Early indications of mixed connective tissue disease may include:*A red face (similar to the lupus skin rash)
*General feeling of being unwell. This malaise may be accompanied by increased fatigue and a mild fever.
*Cold and numb fingers. One of the most common early indicators is known as Raynaud's phenomenon — in which your fingers feel cold and numb, often in response to cold or stress. Fingers may turn white and then purplish blue when the blood vessels constrict. After warming, the blood vessels relax, blood flow resumes and the fingers turn red. Toes also can be affected.
*Swollen fingers. Many people who have mixed connective tissue disease experience swelling in their hands and fingers, sometimes to the point where the fingers resemble sausages.
*Muscle and joint pain. Mixed connective tissue disease also can result in muscle aches and joint swelling and pain. In some cases, the joints may become deformed, similar to what is seen in rheumatoid arthritis.
*Other symptoms, such as Sjögren's syndrome, muscle inflammation, and sclerodactyly (thickening of the skin of the pads of the fingers).
 Causes
CausesDoctors don't know what causes mixed connective tissue disease. The disease is part of a larger group of diseases known as autoimmune disorders. When you have an autoimmune disorder, your immune system — responsible for fighting off disease — mistakes normal, healthy cells for intruders. In connective tissue diseases, your immune system mistakenly attacks the fibers that provide the framework and support for your body.
Flushing
I couldn't find much information about Mixed connective tissue disease and flushing, but what I could find seems to suggest that the flushing and red face issues that are reported for this disease, can stem from the flushing that lupus erythematosus can produce. I did find this information however on the skin symptoms of MCTD: The clinical spectrum seen in patients with lupus, dermatomyositis and scleroderma can range from skin-limited disorders to multi-systemic diseases. The skin can often be the presenting sign of illness.
What does Mixed connective tissue disease look like?
Thyroid problems
 The thyroid gland is located on the front part of the neck below the Adam's apple (or where men have the adam's apple located). The gland produces thyroid hormones, which regulate metabolic rate (how fast calories are consumed to produce energy). Thyroid hormones are important in regulating body energy, body temperature, the body's use of other hormones and vitamins, and the growth and maturation of body tissues. Diseases of the thyroid gland can result in either production of too much (overactive thyroid disease or hyperthyroidism), too little (underactive thyroid disease or hypothyroidism) thyroid hormone, thyroid nodules, and/or goiter. Hyperthyroidism is due to an overproduction of thyroid hormones. Hypothyroidism stems from an underproduction of thyroid hormones. Since your body's energy production requires certain amounts of thyroid hormones, a drop in hormone production leads to lower energy levels.Thyroid problems are much more common in women than in men.
The thyroid gland is located on the front part of the neck below the Adam's apple (or where men have the adam's apple located). The gland produces thyroid hormones, which regulate metabolic rate (how fast calories are consumed to produce energy). Thyroid hormones are important in regulating body energy, body temperature, the body's use of other hormones and vitamins, and the growth and maturation of body tissues. Diseases of the thyroid gland can result in either production of too much (overactive thyroid disease or hyperthyroidism), too little (underactive thyroid disease or hypothyroidism) thyroid hormone, thyroid nodules, and/or goiter. Hyperthyroidism is due to an overproduction of thyroid hormones. Hypothyroidism stems from an underproduction of thyroid hormones. Since your body's energy production requires certain amounts of thyroid hormones, a drop in hormone production leads to lower energy levels.Thyroid problems are much more common in women than in men. List of thyroid related diseases
Hypofunction - Hypothyroidism
Hashimoto's thyroiditis / thyroiditis
Ord's thyroiditis
Postoperative hypothyroidism
Postpartum thyroiditis
Silent thyroiditis
Acute thyroiditis
Iatrogenic hypothyroidism[clarification needed][citation needed]
Thyroid hormone resistance
Euthyroid sick syndrome
Hyperfunction - Hyperthyroidism
Thyroid storm
Graves' disease
Toxic thyroid nodule
Toxic nodular struma (Plummer's disease)
Hashitoxicosis
Nodular abnormalities - Goitre
Endemic goitre
Diffuse goitre
Multinodular goitre
Lingual thyroid
Thyroglossal duct cyst
 How thyroid diseases cause facial flushing
How thyroid diseases cause facial flushingBoth hyper- and hypothyroidism can cause facial (or body-)flushing, sweating and heat intolerance. Research shows that rates of hypothyroidism are higher in patients with rosacea compared with a control group. “In this study, the frequency of hypothyroidism was significantly increased in rosacea patients and no association between hyperthyroidism and rosacea was shown,” concluded the study authors. Hyperthyroidism can by itself also cause flushing and sweating. Redness or flushing of the face (and sometimes the palms) can occur when there's increased blood flow from hyperthyroidism, as well as hot flashes. Patients also complain sometimes about their thyroid medication making them flushed, for instance the drug synthroid/ Levoxyl (Levothyroxine) used to treat hypothyroidism, or carbimazole to treat hyperthyroidism. Flushing is also named by patients as a general symptom of an hypothyroidism attack (sources here and here for instance). 'Sub diseases' like Hashimoto's disease (directly linked to hypothyroidism) can also cause facial flushing, flushed cheeks and redness by itself. In this forum thread, patients write about their thyroid diseases and flushing problems.
 Forum posts from thyroid disease patients experiencing facial flushing
Forum posts from thyroid disease patients experiencing facial flushingJuliva wrote on March 30th 2010: "My face but mostly neck and chest were super flushed/red when I had gone hypo! Probably the first sign for me that I have NEVER experienced before. A friend of mine commented on how "Red" I was and one week later I found out my levels were off. It's been months and I'm still red but not as red as I was.. still working on levels. It was like a bad sunburn."
And she also wrote: "I flushed horribly with this last hypo episode I was in. Face/Neck/Chest. Never had that happen before in the ten years of thyroid disease but I know now it can happen. Looking back I'd say it was the first symptom I had that I was going hypo."
Brucergoldberg replied on March 30th 2010: "I got this too at first. It is called "flushing". It came and went when I started the levo. I also had what I thought was vertigo. My Doctor called them "menopausal hot flashes" because they are very similar. Keep in mind I'm a 42 male."
And he also wrote: "Face flushing definitely could be a sign of thyroid issues. I had the same thing.. Then the ear ringing started."
Bugaboo52 replied: "Is this a hypo symptom or just a side effect of finding the right level of medication? I have experienced the flushing for 4 years and was told it was rosacea, but I am not convinced that is what it is and neither is my dermatologist. I am trying thyroid medicine and I hope this is one symptom that will get better."
Juliva responded: "As for me, this is what I think caused my redness.. My joints/muscles/tendons ached because of the inflammation caused by going hypo. I believe the inflammation also effected my skin. My entire body was inflamed including my nerves. I'm sure the stress and pain weren't helping either. That's my personal take on it."
Jenna96 wrote on December 14th 2008: "I have hypothyroidism and rosacea. My doc started me on levoxyl about 3 years ago. Within about 2 months, I was diagnosed with Rosacea. I finally made the connection about 1 year ago that maybe it was the levoxyl making my face so red, so I stopped taking it. And sure enough my face stopped being so red. But, I really need the thyroid meds so my doc had me take synthroid, this made my face red again with little bumps this time. Just wondering if anyone has this problem and if you have found a solution. Maybe a thyroid treatment that does not cause a red face?"
 wxCathy2 wrote on July 6th 2005: "Hi All, The last month, I've been having an almost permanent red hot face - almost burning - and I'm HOT all the time and sweaty (with night sweats).... but my face feels like it's on fire (not like nerves burning/tingling - just hot). Is this a thyroid symptom? (Still have cold feet though). Thanks! Kathy (diagnosed with thyroid disease and multinodular goiter 1.5 years ago)"
wxCathy2 wrote on July 6th 2005: "Hi All, The last month, I've been having an almost permanent red hot face - almost burning - and I'm HOT all the time and sweaty (with night sweats).... but my face feels like it's on fire (not like nerves burning/tingling - just hot). Is this a thyroid symptom? (Still have cold feet though). Thanks! Kathy (diagnosed with thyroid disease and multinodular goiter 1.5 years ago)"THX 1138 replied: "I'm a guy and I've had the same problem for six years. I was also told that it was rosacea by a dermatologist who later changed it to Seborrheic dermatitis. The skin on my face is reddish in color and I flush after washing my face with water or taking a shower. I always feel tingling sensations on my face and scalp...occasionally burning sensations. I was diagnosed with hypothyroidism about 1.5 months ago and am on Synthroid. I'm currently trying to get on a t3 supplement because my symptoms have not lessened much. I'm hoping my flushing/red skin/burning/tingling face problem will go away once the thyroid is corrected." You can read more forum posts from thyroid patients discussing their flushing issues here.
 Here are some more post suggestions:
Here are some more post suggestions:Photosensitivity is an abnormally high sensitivity to sunlight. People who are photosensitive may develop a skin rash or severe burn even after limited exposure to the sun. Some chemicals contribute to sensitivity to the sun. These can cause two different types of photosensitive reactions: phototoxic and photoallergic. Phototoxic reactions are usually caused when a new chemical in the body interacts with ultraviolet rays from the sun. Medications are the most common cause of this type of reaction. Doxycycline and tetracycline antibiotics for example can cause this reaction. The result is a skin rash that looks like a severe sunburn. These usually develop within about 24 hours of exposure to the sun. Photoallergic reactions can also develop as a side effect of some types of medication. They can also develop because of chemicals found in products like beauty products and sunscreen. Photoallergic reactions to the sun tend to be delayed. It will usually take a few days for a rash to develop after sun exposure (source). The most common symptom is an exaggerated sunburn or a skin rash. The rash may or may not cause itching. In some cases, the sunburn can be so severe that blistering develops. Weeping of the skin and peeling can also occur in severe cases. The amount of sun exposure required for a reaction varies greatly. For some people, very little sun exposure can cause a rash or burn. Others may need prolonged exposure in order to have a reaction. Photo-sensitivity can also cause a worsening of rosacea. Most rosaceans find that sun exposure on their faces can worsen their symptoms. (Read more about this in this blog post, at date January 31st 2019, under peptide LL-37). However, for people with no rosacea, photosensitivity by itself can give them a face that looks like it has rosacea. Photosensitivity may produce a rash, which is known by the general term, photodermatosis. Patients may not associate their skin complaint with exposure to light. It is not always the bright summer sun which is responsible; some people also react to sunlight in winter, and very sensitive subjects may even be affected by fluorescent lamps indoors (source).
 Sometimes photo-sensitivity is caused by a pre-existing disease
Sometimes photo-sensitivity is caused by a pre-existing diseaseThese include conditions such as:
*Lupus erythematosus (especially subacute and systemic forms)
*Dermatomyositis
*Darier's disease
*Rosacea
*Pemphigus
*Atopic dermatitis
*Psoriasis
You can read more detailed information here and here.
What does photosensitivity look like?
Harlequin Ichthyosis Syndrome
Harlequin syndrome is a condition characterized by asymmetric sweating and flushing on the upper thoracic region of the chest, the neck, and the face. Harlequin syndrome happens on only one side of the face. Harlequin syndrome is clearly different from rosacea as normally it makes only half of the face flush and sweat, which is usually not the case with rosacea. In the affected half, the face does not sweat or flush even with simulation. The arms and trunk can also be affected. In contrast to the patient's beliefs, the affected side is not the one that flushes and sweats, but the pale and anhidrotic side. This condition is induced by heat, exercise and emotional factors. It is caused by sustaining an injury to the sympathetic nervous system and it is a rare disease, affecting fewer than 200,000 people in the United States for instance. It can also affect the eyes. You can read more on Harlequin syndrome here and here.What does Harlequin syndrome look like?
Harlequin patient explains symptoms
Auriculotemporal Nerve Syndrome (Frey’s Syndrome)
Frey's Syndrome is a syndrome that includes sweating while eating (gustatory sweating) and facial flushing. The sweating associated with Frey's syndrome can happen from eating any type of food (even ice cream) or from just thinking about food. Patients find it usually extremely embarrassing and uncomfortable. It is caused by injury to a nerve, called the auriculotemporal nerve. Many cases of gustatory sweating show up after surgery or trauma to a parotid gland. Most people have a pair of parotid glands, one located on each side of the face, below and in front of the external ear. The parotid glands are the body's largest salivary glands. Saliva is secreted by salivary glands to aid chewing, swallowing, and digestion of food. If a parotid gland is damaged or if surgery to a parotid is required (damage can occur due to inflammation, infection, and mumps, and tumors can require surgery), then the related nerves may become damaged or may regenerate from such damage in a way that causes them to become "mixed up" and/or "intertwined". This nerve, when it heals, then reattaches to sweat glands instead of the original salivary gland (which had been removed during surgery). The result is that when a person is supposed to salivate, he or she may also sweat and experience facial flushing. This combination of sweating and flushing related to parotid trauma is called Frey's syndrome. Usually Frey's syndrome affects just one side of the face. Gustatory sweating can also occur for no known reason (idiopathic) or related to another medical condition ("secondary hyperhidrosis" due to conditions such as diabetes, cluster headaches, Parkinson's, and facial herpes zoster or shingles). In these cases, the sweating is often experienced on both sides of the face and particularly on the temples, forehead, cheeks, neck, and/or chest, as well as around the lips. Redness and sweating may appear when an affected person eats, sees, thinks about, or talks about foods.
Treatments include:
-Topical anticholinergic ointments (scopolamine, glycopyrrolate)
-Topical antiperspirants (deodorant)
-Topical α agonist (clonidine)
-Botulinum toxin (botox) injections
Botulinum toxin appears to be the easiest and safest method. It provides the longest period of symptom relief with the lowest complications. However, none of these treatments allow a definitive cure; relief is only temporary. For permanent treatment, reconstructive surgery is the only option. You can read more on Frey's syndrome here and here. And check my own blog post about botox injections for rosacea here.
Pictures of Frey's syndrome
Male hypogonadism is a condition in which the body doesn't produce enough testosterone — the hormone that plays a key role in masculine growth and development during puberty — or has an impaired ability to produce sperm or both. Someone may be born with male hypogonadism, or it can develop later in life from injury or infection. The effects and treatment options depend on the cause and at what point in life male hypogonadism occurs. Some types of male hypogonadism can be treated with testosterone replacement therapy.
Hypogonadism, or low testosterone levels, by itself can cause males to flush. This article states: "It is likely that the patient’s flushing was caused by his low testosterone to estrogen ratio, a symptom commonly seen in men undergoing androgen deprivation therapy for prostate cancer."
On top, such males might need to be checked for underlying carcinoid tumors. This article states: "A series of three male patients with secondary hypogonadism has been described, in whom flushing was associated with elevated 24-hour urine 5-HIAA levels. Flushing disappeared, and 5-HIAA levels normalized after starting testosterone enanthate treatment. Male patients with flushing and increased urinary 5-HIAA levels should undergo assessment for hypogonadism after screening for carcinoid tumor."
Those mentioned urinary 5-HIAA levels and hypogonadism was also at play here: Tested were three male patients who had flushing, secondary hypogonadism, and increased urinary 5-HIAA levels, but normal blood serotonin levels. Their clinical and laboratory features were described before and after treatment with testosterone. In addition, six male patients with hypogonadism (three with primary and three with secondary hypogonadism) without flushing were assessed. "Urinary 5-HIAA levels became normal after treatment with testosterone. When testosterone therapy was discontinued in two patients, flushing and increased urinary 5-HIAA levels recurred. Furthermore, flushing and the elevated urinary 5-HIAA values resolved when testosterone treatment was reinitiated. The six patients with hypogonadism without flushing had normal urinary 5-HIAA levels. CONCLUSION: Male patients with flushing and increased urinary 5-HIAA levels should undergo assessment for hypogonadism after screening for carcinoid tumor. If hypogonadism is diagnosed, resolution of flushing and normalization of 5-HIAA may be achieved with testosterone treatment."
Treatments that lower the serum testosterone level, such as orchiectomy or luteinizing hormone-releasing hormone analogues, cause hot flushes in more than 50% of men. Lack of regulatory feedback in the hypothalamus from circulating serum testosterone is the presumed mechanism.
 Erysipelas
ErysipelasErysipelas (which can be translated as red skin, "holy fire", and "St. Anthony's fire") is an acute infection of the upper dermis and superficial lymphatics, usually caused by streptococcus bacteria. Erysipelas is more superficial than cellulitis, and is typically more raised and demarcated. Patients typically develop symptoms including high fever, shaking, chills, fatigue, headaches, vomiting and general illness within 48 hours of the initial infection. The erythematous skin lesion quickly grows bigger and has a sharply raised edge between the red skin and the normal looking skin. It appears as a red, swollen, warm, hardened and painful rash, similar in consistency to an orange peel. Lymph nodes may be swollen and skin swelling may occur. Occasionally, a red streak extending to the lymph node can be seen. The infection may occur on any part of the skin including the face, arms, fingers, legs and toes, but it tends to favor the extremities (arm, leg, face). Fat tissue is most susceptible to infection, and facial areas typically around the eyes, ears, and cheeks. Repeated infection of the extremities can lead to chronic swelling. This disease is most common among the elderly, infants, and children. People with immune deficiency, diabetes, alcoholism, skin ulceration, fungal infections and impaired lymphatic drainage (e.g., after mastectomy, pelvic surgery, bypass grafting) are also at increased risk. This disease is diagnosed mainly by the appearance of well-demarcated rash and inflammation. Depending on the severity, treatment involves either oral or intravenous antibiotics, using penicillins, clindamycin or erythromycin. While illness symptoms resolve in a day or two, the skin may take weeks to return to normal.
Other Diseases Causing Episodic Flushing
can cause episodes of flushing affecting the face and chest when triggered by emotion or certain foods. It is also called Brunner syndrome, and is caused by a monoamine oxidase A (MAOA) deficiency, which leads to an excess of monoamines in the brain, such as serotonin, dopamine, and norepinephrine (noradrenaline). Blood serotonin can become raised and the activity of monoamine oxidase is decreased. See for more information this link.
Pheochromocytoma
Pheochromocytoma is a type of neuroendocrine tumor that grows from cells called chromaffin cells. Flushing is rare in patients with pheochromocytoma, a rare, usually non cancerous (benign) tumor that develops in cells in the center of an adrenal gland (link). If flushing occurs at all, it is seen after an episode of hypertension, tachycardia, palpitations, chest pain, severe throbbing headaches, and excessive perspiration. Paleness is typically seen during the attack, and mild flushing may occur after the attack as a rebound vasodilation of the facial.
Asthma flushing
During an asthma attack the breathing pathways constrict, making it difficult
to exhale carbon dioxide. When you can't exhale an adequate amount of
carbon dioxide, you can't inhale oxygen. The lack of oxygen causes the
face to turn red. This is not a true rosacea flush, but it's not uncommon
for rosacea suffers to also have asthma. Asthma flushing/redness can also result from a food allergy, airborne pollutants or toxins. Aside from using regular medication to control asthma, using an
allergen air filter and changing it every one to two weeks can help
reduce indoor pollens, toxins, fungi, and/or molds in the home. Air
purifiers can also be helpful. Controlling your environment as much as
possible can help to relieve some of the symptoms of asthma.
POTS; postural orthostatic tachycardia syndrome
I stumbled upon this blog, where a girl blogs about her dealing with the disease POTS. Postural orthostatic tachycardia syndrome (POTS) is defined as an abnormal increase in heart rate when sitting or standing upright. There are many causes. Although blood pressure does not necessarily fall, symptoms are similar to low blood pressure and can consist of dizziness, fainting, headache, sweating, shakiness, nausea, poor concentration and memory, discoloured hands and feet, a sense of anxiety, chest pains and many others. These symptoms get worse when the patient is standing. Treatment can consist of high fluid intake, care with posture, careful fitness training and, in some patients, high salt intake and medication (source). The blogger mentioned also describes being flushed in the face at times and shared a picture. She writes: "My flushing and hives have died down significantly since I got off the beta blocker (I also took myself off of all 3 antihistamines). I still get the episodes but not as bad and it’s been something I could ignore because they haven’t been nearly as bad. But today, after eating the same macaroni and cheese that I have eaten recently with no symptoms, my face flushed and I got the standard inflammation and itchiness in my eyes, lips and nose. My whole being is fatigued and I just to put my head down and close my eyes. I feel lethargic and worn down. Brain fog has definitely arrived. My face isn’t nearly as red as it can get and I don’t have the hives down my neck, chest and arms, though I have that feeling like it’s slightly there (and I am definitely itchy). I am not sure what my blood pressure is but I know my heart rate is up and it’s pounding too. As you can see from my other post today, I am having a pretty symptomatic day and I know I probably need to lay down – though I can’t because I am at work. I am just confused. I know I am in a downswing in regards to how I have been feeling physically, but what in the world is triggering the flushing episode to return in a huge way? I have been considering looking into antihistamines again now that I am off the beta blocker (since I believe that was the culprit in making my flushing episodes significantly worse!). The only thing is that I want to know what’s triggering these episodes first, before I go back on anything to treat them. [..] I guess I will have to start using my blood pressure/heart rate monitor again and start keeping notes on everything for awhile. But to be perfectly honest, I feel ridiculous pulling out that monitor while I am out and about and especially at work. It’s not quiet and yes, I will admit that I am afraid that people will think I am just looking for attention… and that’s why I haven’t been doing it. Yeah, I know." - In this research, POTS is linked to facial flushing and mast cell issues:
 |
| Link to image Source |
I stumbled upon this blog, where a girl blogs about her dealing with the disease POTS. Postural orthostatic tachycardia syndrome (POTS) is defined as an abnormal increase in heart rate when sitting or standing upright. There are many causes. Although blood pressure does not necessarily fall, symptoms are similar to low blood pressure and can consist of dizziness, fainting, headache, sweating, shakiness, nausea, poor concentration and memory, discoloured hands and feet, a sense of anxiety, chest pains and many others. These symptoms get worse when the patient is standing. Treatment can consist of high fluid intake, care with posture, careful fitness training and, in some patients, high salt intake and medication (source). The blogger mentioned also describes being flushed in the face at times and shared a picture. She writes: "My flushing and hives have died down significantly since I got off the beta blocker (I also took myself off of all 3 antihistamines). I still get the episodes but not as bad and it’s been something I could ignore because they haven’t been nearly as bad. But today, after eating the same macaroni and cheese that I have eaten recently with no symptoms, my face flushed and I got the standard inflammation and itchiness in my eyes, lips and nose. My whole being is fatigued and I just to put my head down and close my eyes. I feel lethargic and worn down. Brain fog has definitely arrived. My face isn’t nearly as red as it can get and I don’t have the hives down my neck, chest and arms, though I have that feeling like it’s slightly there (and I am definitely itchy). I am not sure what my blood pressure is but I know my heart rate is up and it’s pounding too. As you can see from my other post today, I am having a pretty symptomatic day and I know I probably need to lay down – though I can’t because I am at work. I am just confused. I know I am in a downswing in regards to how I have been feeling physically, but what in the world is triggering the flushing episode to return in a huge way? I have been considering looking into antihistamines again now that I am off the beta blocker (since I believe that was the culprit in making my flushing episodes significantly worse!). The only thing is that I want to know what’s triggering these episodes first, before I go back on anything to treat them. [..] I guess I will have to start using my blood pressure/heart rate monitor again and start keeping notes on everything for awhile. But to be perfectly honest, I feel ridiculous pulling out that monitor while I am out and about and especially at work. It’s not quiet and yes, I will admit that I am afraid that people will think I am just looking for attention… and that’s why I haven’t been doing it. Yeah, I know." - In this research, POTS is linked to facial flushing and mast cell issues:
can als provoke facial flushing. (Link)
Lyme disease
can also provoke facial flushing. Read more on Lyme disease here and here. Please also watch this very insightful and important video on Lyme disease. Lyme disease can affect the central nervous system and cause skin burning and redness. Lyme disease can also make your body temperature fluctuate, and cause night sweats and flushing of the face and head. This documentary below is fantastic in terms of thoroughness and how interesting it is. If youtube takes it off for some reason, you can also watch it here and here.
 Kittydoc wrote on August 15th, 2017: "Neurogenic rosacea turned out to be Lyme disease. - Hi all, I posted for the first time a few months back about my neurogenic rosacea and wanted to come back with an update. A brief history - I developed extreme facial burning and redness over the course of one day out of what seemed to be nowhere. Thus began my nightmare. Although the redness has almost completely resolved (other than a faint blush over the bridge of my nose and my upper cheeks) the burning has continued. As I reported previously, to the casual observer I probably appear normal. The burning was constant at first, but now has become more random. It flares for a few days and then calms down, only to flare a week later (or less). Sunlight and computer screens are my two big triggers. If I'm not in a large hat and wearing 50 spf or more when I leave the house my skin reminds my of my error later on in the day. I was instantly diagnosed with Rosacea, and later diagnosed with neurogenic Rosacea. I tried several treatments from 2 different derms (metrogel, solantra, etc) but they didn't help at all. One derm recommended I try an SSRI or an anti-seizure med since this form of the disease is sometimes responsive to those. Tried one dose of Lexapro and ended up having a massive panic attack. I haven't been the same since that panic attack. For whatever reason this episode led to a generalized anxiety disorder. I was put on xanax and told I should try another SSRI (ummm, no way). I next started experiencing horrible insomnia and getting weird muscle twitches and spasms. All in all, I ended up seeing 2 GP's, 2 derms, 2 naturopaths, a chiropractor, and an acupuncturist before getting to the root problem.
Kittydoc wrote on August 15th, 2017: "Neurogenic rosacea turned out to be Lyme disease. - Hi all, I posted for the first time a few months back about my neurogenic rosacea and wanted to come back with an update. A brief history - I developed extreme facial burning and redness over the course of one day out of what seemed to be nowhere. Thus began my nightmare. Although the redness has almost completely resolved (other than a faint blush over the bridge of my nose and my upper cheeks) the burning has continued. As I reported previously, to the casual observer I probably appear normal. The burning was constant at first, but now has become more random. It flares for a few days and then calms down, only to flare a week later (or less). Sunlight and computer screens are my two big triggers. If I'm not in a large hat and wearing 50 spf or more when I leave the house my skin reminds my of my error later on in the day. I was instantly diagnosed with Rosacea, and later diagnosed with neurogenic Rosacea. I tried several treatments from 2 different derms (metrogel, solantra, etc) but they didn't help at all. One derm recommended I try an SSRI or an anti-seizure med since this form of the disease is sometimes responsive to those. Tried one dose of Lexapro and ended up having a massive panic attack. I haven't been the same since that panic attack. For whatever reason this episode led to a generalized anxiety disorder. I was put on xanax and told I should try another SSRI (ummm, no way). I next started experiencing horrible insomnia and getting weird muscle twitches and spasms. All in all, I ended up seeing 2 GP's, 2 derms, 2 naturopaths, a chiropractor, and an acupuncturist before getting to the root problem. After doing my own research I came up with Lyme. I asked one of the naturopaths to test me and I came up positive. I started treatment today. I'm coming back to this board because I'm hoping to reach anyone out there that has the neurogenic form of the disease, especially people that have just started having similar symptoms, or for those that experience any symptoms beyond the skin in association with their Rosacea. I spent the better part of year thinking I had Rosacea when I didn't. My treatment for Lyme has been delayed since everyone kept chalking it up to stress and Rosacea. I know that it's definitely more of an out there diagnosis for Rosaceans, but I wanted to put it out there in case my story helps anyone. [..] I had the Igenex IGg/IGm and and IFA performed. They don't look directly for spirochetes, but tend to use antibody/PCR/IFA. Lyme disease, especially when it's been longer than the acute phase of 6-8 weeks can sometimes be a bit difficult to diagnose - so much so that some doctors feel comfortable diagnosing Lyme disease based entirely on clinical signs. Most doctors (unless they are what the lyme community calls lyme literate doctors) won't treat you without a positive blood test. Fortunately - or unfortunately depending upon how you look at it - my IGg and IFA was positive. My doctor is convinced the phantom burning in my face, along with the sensitivity I've experienced is due to a neuropathy caused by Lyme attacking my nervous system. My symptoms seem to be neural and digestive so far - although the digestive is likely due to inappropriate neural stimulation too. My treatment consists of two antibiotics, doxycycline and Augmentin. I am also on a variety of supplements to to support my gut health, detox from the lyme die off, and prevent yeast overload from the chronic antibiotics. This will go on for months at a minimum. If I don't respond well to the orals he mentioned placing a port for IV antibiotics. There are also more unconventional treatments out there such as Vit C IV infusions and UV treatment. I'm just starting to get myself educated about this disease, so I don't know all the ins and outs yet. I've just joined a support forum like this one for Lyme. It's a real drag going from one chronic crappy disease which is poorly understood to another chronic crappy disease which is poorly understood, but at least I have an accurate diagnosis now. I remember being bitten by a tick, I didn't think it was a deer tick at the time. I also didn't get a classic rash or feel sick after the bite. I now know that 50% of people don't remember getting bit when they come up lyme positive. Now that I know better I wish I would have checked it out. Live and learn I guess. Kittydoc"
Perioral dermatitis
 The lesions of rosacea that initially show up in the central areas of the face. They can be papules and pustules against a background of skin redness, telangiectasia (visible blood vessels), flushing and eventually in some cases thickening of the affected skin. People can either develop rosacea out of the blue, over time (for instance due to genetics or as a result of steroid cream use) or as a result of flushing from other conditions. Because persistent flushing from any cause may eventually lead to rosacea. Patients with severe flushing caused by mastocytosis can for instance develop rosacea in less than 1 year after the onset of flushing episodes. This is a blog by a doctor who works for the German army and here he writes about a patient of his with rosacea and face swelling, and how he treated her. I have already written a lot about rosacea on this blog and I will just give some common symptoms and characteristics of rosacea here, together with pictures of rosacea skin. It might serve to see differences with the other medical conditions mentioned in this post.
The lesions of rosacea that initially show up in the central areas of the face. They can be papules and pustules against a background of skin redness, telangiectasia (visible blood vessels), flushing and eventually in some cases thickening of the affected skin. People can either develop rosacea out of the blue, over time (for instance due to genetics or as a result of steroid cream use) or as a result of flushing from other conditions. Because persistent flushing from any cause may eventually lead to rosacea. Patients with severe flushing caused by mastocytosis can for instance develop rosacea in less than 1 year after the onset of flushing episodes. This is a blog by a doctor who works for the German army and here he writes about a patient of his with rosacea and face swelling, and how he treated her. I have already written a lot about rosacea on this blog and I will just give some common symptoms and characteristics of rosacea here, together with pictures of rosacea skin. It might serve to see differences with the other medical conditions mentioned in this post. Rosacea consist of redness of the facial skin. It is considered a difficult to treat dermatological condition, which is often chronic in nature. Rosacea usually causes persistent redness in the central portion of your face, including the cheeks, chin, nose and even ears and forehead. Some people find that the redness can even spread to the neck and chest, but this is more rare. Apart from facial redness, small blood vessels might also become visible over time on your skin. Many people who have rosacea also develop bumps on their face that resemble acne, the so called p&p's (papules and pustules). These bumps sometimes contain pus. Sometimes patients get all of those symptoms combined. More often they suffer from one or the other 'subtype'. Subtype 1 patients are dealing more with general redness, skin burning and facial flushing. The skin may feel hot and tender. This subtype is also called Erythematotelangiectatic rosacea. Those suffering from subtype 2 are dealing more with the p&p's and skin inflammation, and not so much with flushing. About half of the people who have rosacea also experience eye dryness, with irritated and swollen, reddened eyelids. This is called ocular rosacea. Rarely, rosacea can thicken the skin on the nose, causing the nose to appear bulbous (rhinophyma). This occurs more often in men than in women. Rosacea is often characterized by flare-ups and remissions, especially in the early stages. Initially the redness on the cheeks, nose, chin or forehead may come and go. Over time, the redness tends to become ruddier and more persistent, and visible blood vessels may appear. Left untreated, bumps and pimples can develop or the flushing and burning issues can become more persistent. Although rosacea can affect all segments of the population, individuals with fair skin who tend to blush more easily are believed to be at greatest risk. The disease is more frequently diagnosed in women, but more severe symptoms tend to be seen in men -- perhaps because they often delay seeking medical help until the disorder reaches advanced stages (source and source).
 Erythematotelangiectatic rosacea
Erythematotelangiectatic rosaceaWhile considered by many to represent a separate entity, erythematotelangiectatic rosacea may in fact be difficult to distinguish from normal facial flushing and sun-damaged skin. Doctors often looks at the extent of baseline facial telangiectasia, hypopigmentation and hyperpigmentation. However, since these 3 conditions are all common, they may coexist in many patients.
 *Rosacea usually develops in your 20's or 30's, or even during menopause for women (but it can also affect younger people! Mine developed at age 19 and I know several other young patients).
*Rosacea usually develops in your 20's or 30's, or even during menopause for women (but it can also affect younger people! Mine developed at age 19 and I know several other young patients).*The rosacea redness usually worsens over time (if left untreated).
*The redness can be seen on the cheeks but also the chin and nose (and even forehead and ears for some)
*People with rosacea often have a pale complexion and a tendency to blush (but it can also affect those with olive skin tone and even darker skin tone; but statistically predominantly people with fair skin).
*In the earlier stages the skin can become red, yet it also can look pale again once a flare is over. Flushing flares can last short or longer. Only with time the redness usually can become more permanent.
*Generally occurrence of worsening of symptoms after sun exposure, drinking alcohol or eating certain foods.
*Skin becomes often dry and flaky
*Rosacea flushing isn't accompanied by sweating
*Papulas/spots may appear on the face
*The face can become a bit swollen from the redness, called oedema.
* In a very recent survey conducted by the NRS, nearly 93 percent of 1,709 rosacea patients said they had experienced physical discomfort as a result of the disorder, with burning and stinging the most commonly cited pain sensations. Among the other physical discomforts experienced by the survey participants were tightness, cited by 45 percent; swelling, named by 44 percent; tenderness, mentioned by 41 percent; tingling, 32 percent; prickling, 25 percent; and headache, 19 percent.
Pictures of rosacea
Benign causes of flushing
Emotions
Temperature
Food or beverage
Rosacea
Emotions
Temperature
Food or beverage
Rosacea
Climacteric flushing
Fever
Alcohol
Uncommon, serious causes
Carcinoid
Pheochromocytoma
Mastocytosis
Anaphylaxis
Other causes
Medullary thyroid carcinoma
Pancreatic cell tumor (VIP tumor)
Renal cell carcinoma
Fish ingestion
Histamine
Ciguatera
Psychiatric or anxiety disorders
Idiopathic flushing
Fever
Alcohol
Uncommon, serious causes
Carcinoid
Pheochromocytoma
Mastocytosis
Anaphylaxis
Other causes
Medullary thyroid carcinoma
Pancreatic cell tumor (VIP tumor)
Renal cell carcinoma
Fish ingestion
Histamine
Ciguatera
Psychiatric or anxiety disorders
Idiopathic flushing
Neurologic
Parkinson’s
Migraine
Multiple sclerosis
Trigeminal nerve damage
Horner syndrome
Frey syndrome
Autonomic epilepsy
Autonomic hyperreflexia
Orthostatic hypotension
Streeten syndrome
Medications
Very rare causes
Sarcoid, mitral stenosis, dumping syndrome, male androgen deficiency, arsenic intoxication, POEMS syndrome, basophilic granulocytic leukemia, bronchogenic carcinoma, malignant histiocytoma, malignant neuroblastoma, malignant, ganglioneuroma, peri-aortic surgery, Leigh syndrome, Rovsing syndrome.
Parkinson’s
Migraine
Multiple sclerosis
Trigeminal nerve damage
Horner syndrome
Frey syndrome
Autonomic epilepsy
Autonomic hyperreflexia
Orthostatic hypotension
Streeten syndrome
Medications
Very rare causes
Sarcoid, mitral stenosis, dumping syndrome, male androgen deficiency, arsenic intoxication, POEMS syndrome, basophilic granulocytic leukemia, bronchogenic carcinoma, malignant histiocytoma, malignant neuroblastoma, malignant, ganglioneuroma, peri-aortic surgery, Leigh syndrome, Rovsing syndrome.
Steps to take for evaluation of a patient with a Flushing Disorder
 These are some tips for doctors about diagnosing patients with flushing symptoms. He or she needs to first look at clinical characteristics. Are there certain things that
trigger the flushing? This could suggest an underlying systemic disease as the cause
for the flushing, such as mastocytosis and carcinoid syndrome.
These are some tips for doctors about diagnosing patients with flushing symptoms. He or she needs to first look at clinical characteristics. Are there certain things that
trigger the flushing? This could suggest an underlying systemic disease as the cause
for the flushing, such as mastocytosis and carcinoid syndrome.
Morphology
- Is there a basic feature that comes and goes?
- Is the redness patchy or even?
- What is the color of the flush?
- Is there a bluish-purple hue to the skin?
- Is the flushing preceded or followed by paleness?
The morphology of the flushing may suggest not only the cause of the flushing, but also - in the case of carcinoids - the anatomic origin of the disorder. Associated Features. These may include respiratory symptoms, gastrointestinal symptoms, headache, urticaria, facial edema, hypertension, hypotension, palpitations, or sweating. Temporal Characteristics. Temporal characteristics are the frequency of the flushing and the timing of the specific features during each flushing reaction. Important information can be obtained from a 2-week diary in which the patient records how long and how severe the flushing events were, and lists exposure to all outside agents. When the diagnosis remains obscure after evaluation of the 2-week diary, the patient can be given an exclusion diet, listing foods high in histamine, foods and drugs that affect urinary 5-HIAA tests, and foods and beverages that cause flushing. If the flushing reactions completely disappear, the doctor can start to reintroduce the excluded items individually, one by one, to identify the food item that causes the flushing. If the flushing reactions continue unchanged, then further metabolic workup may be undertaken. Always make sure when you have rosacea that you maintain a gentle skin care regimen. Try to identify your triggers and avoid them. Look together with your dermatologist for treatment options. For instance medication, natural anti inflammatory treatment options, diet or laser/IPL. Treating your rosacea successfully will help you achieve and hopefully maintain remission.
So, in summary
Rosacea is said to typically start in people's late twenties, thirties, forties or even onwards. Some doctors insist they don't see it in teenagers or youngsters, but the forums are proof that this is not correct. I developed rosacea virtually out of the blue at age 19. Other patients had a long standing tendency to blush or get red as a youngster and found that this developed into rosacea over time. A good portion of rosacea patients also seem able to trace rosacea back in their family history, and know parents or grand parents who had rosacea symptoms. However, this definitely isn't the case for everyone. The use of Accutane/Roaccutane or (Hydro)cortisone cream can also have been the trigger for rosacea to erupt. When people develop red, burning and flushed skin or bad skin rashes after use of any of these creams, then steroid induced rosacea should be the first suspect. Rosacea tends to wax and wane and can flare badly, only to calm down again some time later. Flushing also tends to be temporary initially. Some people with rosacea have a lot of baseline redness, but those mainly affected by the flushing can have relatively pale and normal looking skin when not flushed. This is another characteristic of rosacea.
The redness of rosacea is usually not sharply marked from unaffected skin. So the redness usually blends in somewhat, and the flushing can affect only part of the cheeks, usually the inner cheeks closest to the nose. Redness and flushing tend to to start on the cheeks for many, although especially males also find their nose and ears affected quickly. The chin can also get red with time, and even the forehead. This is another characteristic of rosacea, although not an entirely exclusive one. Rosacea tends to cause both facial flushing and redness, or/and small red paps and pimple like eruptions. Some people mainly deal with either the one or the other subtype (subtypes 1 and 2), but most people with rosacea experience both symptoms at some point, more or less severe. For instance, I have subtype 1, with erythema, burning, redness and flushing and very little outbreaks, but when I flush badly or eat certain foods I also get red dots that look like little red pimples without a real white head (but often with some fluid or very fluid thin puss inside).
With rosacea, most flushing reactions result from benign causes. However, since flushing may be the presenting sign or symptom of several life-threatening conditions, it it important to discuss your symptoms with your doctor. If needed, he or she will do more tests to rule out some other diseases. For instance systemic mastocytosis, carcinoid syndrome and other tumors. Read also this link from the Rosacea Org.
A little peek into the experiences of rosacea patients with diagnosing
their rosacea and at times their underlying coexisting health problems
Froggirl wrote on May 23th 2014: "It seems to be pretty well accepted in the medical literature that a
diagnosis of rosacea can only be made once a multitude of other
conditions are first ruled out. My doctor did but i wondering if
everyone's doctor or derm are ruling these things out to? Especially for
people for who redness and flushing are the key symptoms (rather than
P&P). I remember back when i first started getting flushing that the only
thing that came up on the internet for flushing was rosacea, but have
since found out there are many many things which can look like rosacea,
so thought i'd put it out there. When evaluating patients with rosacea, it is important to exclude
the diagnoses of polycythemia vera, photosensitive eruption, lupus
erythematosus, mixed connective tissue disease, carcinoid syndrome,
systemic mastocytosis, or side effects from long-term facial application
of topical steroids. Since rosacea is typically limited to the face,
extra facial erythema is generally an exclusionary sign. Rosacea
flushing is associated with burning or stinging but not sweating,
lightheadedness, or palpitations. http://rosacea.ii.net/news/2006/08/r...t-rosacea.html Most
of these are unlikely or rare but there are also some pretty common
conditons that can cause flushing or make it worse, such as allergies,
food intolerances, thyroid issues, oestrogen imbalance (for women),
lactose intolerance, fructose intolerance and coeliac disease. Of course
all of the above generally cause other symptoms aside from
flushing or redness, most commonly GI issues, but some of these can be
symptom less, like Coeliac disease, which is why only about 1 in 1000
people are diagnosised with it despite approx 1 in 100 having it. And
the fact that lot's of rosacea say they improve when cutting out wheat
or dairy products makes me wonder if some of us also have other things
going on, aside from rosacea. Anyway most of these are simple blood
tests, so is everyone getting checked out for these things?"
 Melissa W. replied: "Hi Kate, My derm diagnosed rosacea without any workup to rule out other diseases.
It wasn't until I got chilblains that the drs ordered the whole series
of connective tissue blood tests to R/O all the other stuff. And that
was months after I was formally diagnosed with rosacea. Best wishes, Melissa"
Melissa W. replied: "Hi Kate, My derm diagnosed rosacea without any workup to rule out other diseases.
It wasn't until I got chilblains that the drs ordered the whole series
of connective tissue blood tests to R/O all the other stuff. And that
was months after I was formally diagnosed with rosacea. Best wishes, Melissa" Patty replied: "I was diagnosed with rosacea by my primary dr. who sent me for more blood tests to test for lupus, and other auto-immune type diseases. I have had more done with my derm, and also a more complete workup done by a rheumatologist. My ANA was on the high side of normal, which is why all the blood work. I've been told I have a mild case of Raynaud's, very common in rosaceans from what I see."
Froggirl wrote:
"Oh and i forgot erythromelalgia as a very rare cause of facial flushing.
So i guess it's not so common to get tested straight away, maybe my
doctor did because my facial flushing came so suddenly and rapidly got
worse and worse? And then i developed flushing in other areas, like my
knees, hands, feet and chest which is when he started testing me for the
rarer and more obscure things. So many tests and still no answers for
me which means there is at least one other thing missing form this list,
so if anyone knows what it is that would be great! ;) " [..] "Unfortunately having triggers doesn't automatically mean rosacea. Carcinoid (sic) and mastocytosis both get triggered by many of the same things as rosacea, ie stress, heat, cheese, alcohol to name a few, with the result being flushing, wheezing, and GI issues. Most of the rosacea food triggers are on the list because they are high in serotonin, histamine or msg, so if you have food intolerance's to these chemicals than eating them can cause flushing (and other things like headaches) even without rosacea. Plus any conditions that involve inflammation in the skin, like seb derm (or most other things on Brady Barrows list), will get redder with anything that increases blood flow in the skin, so with heat, alcohol, or even with the same foods to avoid for rosacea. And then this inflammation can trigger flushing. It all gets so complicated but i guess this range of things is why it's
not always so straight forward to get a diagnosis of rosacea, or
anything else on this list!"
Grace replied: "Froggirl, Thank you for your post, for I have been frustrated by this also. GP and
derms have taken one look at me, no more than a foot away, and have
diagnosed me with rosacea and quickly l walked out the door. Yet I have
questioned this, it may very well be, yet I do believe there are other
things going on, for like you, I started flushing very suddenly and very
badly and the progression has been a bit severe I now get very bad
swelling in my nose, feet and hands, and my nose is constantly running -
symptoms I have never had before. Sometimes I wake up in the middle of
the night and it hurts to make a fist, due to the swelling in my
fingers. I had to adamantly request blood tests to screen out lupus and
autoimmune conditions. I know for me hormones are part of it. For
about 9 months ago my menstruation stopped, suddenly, even though i'm
only 42. And I think since people react so differently to so many things, we all
have different things going on in our bodies that is causing these
similar symptoms clumped as "rosacea". Grace"
Bluesky replied: "Hi, I found this to be very interesting, so thanks for bringing this topic up again Melissa... I'm going to the university derm center but my insurance will not cover it, so I would like to go to my regular doctor and get some testing done as opposed to at the derm. What kind of testing is suggested?? I would like to rule out any of these diseases or anything else that might be causing this awful flushing and redness, so can someone please provide a list of what should be tested for, deficiencies etc.and also diseases?? Thank you!! Something I notice also, I flush in my feet. What is that?? Lol! :( Really though, when I'm outside in the sun or the heat, or even if no heat and I'm walking or doing some kind of vigorous exercise, my feet will turn really red and flush, at first I thought, oh no it's sunburn, but my feet have never burned at all like that, and afterwards they always go back to white again. Is that a normal rosacea sign? Any thoughts? Thanks! Bluesky"
Melissa W. replied: "Flushing hands and feet could be related to Raynaud's as well I believe."
Meg replied on February 15th 2011: "Originally Posted by Mogge: i have the same, but not just my feet. My face,
back of the hands and top of my chest also gets really red. At first i
thought of Lupus but since I'm a caucasian man in my 20's its highly
unlikely. Does yours feel like "pulsating" or "throbbing" when they get
really red? feels like some sort of swelling
That may be Erythromelalgia. It's usually hands and feet, but faces can be involved too. Meg."
Mogge replied back: "EM is rare though (about 1 in 100.000) which makes even Lupus Erythematosus more likely. My hands and feet tend to "flare" when im
drinking alcohol,shower in warm water or even by wearing a long-sleeved
sweater indoors so it kind of fits with EM but it seems unlikely to have
such a rare disease."
Meg wrote back: "EM is not as rare as once thought, although it is considered a rare
disease according to NORD. With that said, I have never heard of hands
or feet involvement when it comes to Lupus, although I may be wrong. It
you have flushed extremities that turn red and burn, then it qualifies
as EM. You can have varying underlying causes and it's still considered
EM if you have these combined symptoms. Meg"
Mogge replied: "The most common rash in lupus is the butterfly on the face. Rash on the
back of the hands and on the V-neck area are sometimes presented as
well. But that is usually after being exposed to UV-light. It could be
EM but even if its more common than 1 in 100.000 the chance is still
pretty slim. Something like Histaminosis (histamine intolerance) would
be more likely. Anyway i think im going to get a new appointment with my
dermatologist and show her all the rashes and not just the one on my
face"
Shantelle replied to this thread: "Hi all In regards to the above posts...Yes, Lupus is not as common in males as it is in females (Ratio Females 9:1 Males). Lupus can present itself in may different forms, and symptoms (all inflammatory) often masquerade as other diseases or health issues. The butterfly rash is not seen in every Lupus patient, but if it does appear it can certainly masquerade itself as Rosacea (Type 1). Inflammatory hand and and feet symptoms are common symptoms of lupus, particular if the person has systemic lupus, or Raynaud's (Raynaud's is often seen in patients with autoimmune disease) or chronic cutaneous lupus affecting the hands or feet (lupus chilblains/ lupus pernio). If anyone thinks that they might have lupus they should see their GP for a referral to a Rheumatologist (multiple inflammatory symptoms) or Dermatologist (symptoms all skin related). Lupus symptoms information:
http://www.dermnet.org.nz/immune/cutaneous-lupus.html
http://www.lupus.org/webmodules/weba...268&zoneid=526
http://www.hopkinslupus.org/lupus-info/"
Mogge replied: "Lupus is a possibility, but my symptoms are usually induced by stress, heat, alcohol, caffeine and eating which indicates Systemic Mastocytosis. My symptoms are: swelling of the hands,feet and face, chronic diarrhea,stomach pain,blodshot eyes,weightloss,joint pain, myalgia, malar rash+rash on chest,hands and feet,vertigo,vomiting,blurry vision and fatigue. Those are very common in Lupus but mine are triggered by the environment which is why I think it's Mastocytosis. Both are uncommon diseases, Lupus is pretty rare in caucasian males and Systemic Mastocytosis affects about 1 in 1.000.000 people."
GiGi replied: "I have never had any specific blood tests nor other check ups done, though I have some other symptoms. (Fatigue, foggy brain and digestive issues.) I am wondering, who do you ask to run those tests? My NHS GP didn't show any interest/knowledge, and the private dermatologist I consulted seems to be not aware of any tests neither... If someone who lives in the UK is reading this thread, I would greatly appreciate recommendations for a good private GP/specialist doctor who does run these kind of tests and is willing to investigate possible underlying illnesses. Many thanks."
Brady Barrows replied: "Two recommendations:
*Professor Tony Chu, FRCP
West London Dermatology Centre
227-229 Chiswick High Road, Chiswick, W4 2DW
*Frank Powell, M.D.
Consultant Dermatologist
Regional Centre of Dermatology
Mater Misericordiae Hospital
Dublin, Ireland
Leading European authority on rosacea
Also these posts:
What to ask my physician?
What should I know about diagnosing rosacea?"
John111 wrote on November 27th 2011: "Hi I'm 25 years old and have a condition which came on around adolescence. I have constant red cheeks that cover the whole area of cheeks and have a red nose. This redness started out as light pink and has now become permanent and the color is now dark red. I am very sensitive to hot/cold and my face can burn with me having a malar complexion. I also get red rashes on upper body, arms and around knees. My skin can also become red when exposed to heat and alcohol makes the flushing and redness a lot worse. I also have constant redness in side of eyes and redness can become worse while looking at a screen for too long or rubbing them as sometimes I feel like there is sand in my eyes. My vision has also become blurred. I also suffer from excessive sweating and sweat during light exertion, walking. I also experience sharp sudden pains in my chest when I breath in deeply and I have to change my body position and take small breathes and they pass. I can also get pains in my lungs and these can also be sharp too. Occasionally I get sharp paralyzing pains in rectum and these can be quite intense and pass after a few seconds. My theory is that call these symptoms relate to an autoimmune disease. I have been to a endocrinologist and he tested me for carcinoid cancer and pheos which are adrealan tumours. He tested my urine with 24hr tests and my thyroids and both came back fine. Last week I also went to get tested for diabetes and the nurse said that the blood tests, test for thyroids and covered everything. - My question is would lupus show up on a standard blood test for diabetes or on a thyroid test or is there any specific test for lupus. Also can anyone help me with my condition and does anyone know if my symptoms are like lupus or an autoimmune disease? I don't have any pustules, raised skin or red spots on face, my skin is smooth but red and can become inflamed on exposure to hot and my complexion can become much redder on exposure to cold. I also have a shy personality and can flush easily. The only time my cheeks turns pale is when I feel sick or when I've taken stimulants like speed and mdma. Does anyone know why this is? Is this a hormonal problem or does anyone know a supplement that will help with the redness. I just have red cheeks with a red nose, redness on neck and upper body with no bumps or roughness. Any help would be welcome as I don't know why I turn pale. Any replies would be welcome. Thanks, John"
 Emlarkin replied: "I'm 16 and I've had this problem develop from about 8 years old. My mum
keeps saying she doesn't think it is rosacea but it's getting worse.
What do you think? I am so sick of looking orange when I cover it up
with makeup. [...] The worst is in the evening, usually it gets really hot and red almost like
it's burning. When it's not so red there are white splotches in between
but if it's flushing then it completely covers my cheeks and sometimes
under my chin. My face doesn't sweat really. I would say it is
rosacea, as looking at some of the seborrhoeic dermatitis information, it
is not affected by diet. Whereas I get worse when eating hot food like
curries or too many fatty foods. My skin is generally best first thing in the morning, but as soon as I get too
hot I will flush for hours after. So embarrassing and no one
understands that I'm NOT blushing! It's good to know other people
understand here."
Emlarkin replied: "I'm 16 and I've had this problem develop from about 8 years old. My mum
keeps saying she doesn't think it is rosacea but it's getting worse.
What do you think? I am so sick of looking orange when I cover it up
with makeup. [...] The worst is in the evening, usually it gets really hot and red almost like
it's burning. When it's not so red there are white splotches in between
but if it's flushing then it completely covers my cheeks and sometimes
under my chin. My face doesn't sweat really. I would say it is
rosacea, as looking at some of the seborrhoeic dermatitis information, it
is not affected by diet. Whereas I get worse when eating hot food like
curries or too many fatty foods. My skin is generally best first thing in the morning, but as soon as I get too
hot I will flush for hours after. So embarrassing and no one
understands that I'm NOT blushing! It's good to know other people
understand here."J1992 replied: "Emlarkin, your skin is red in exactly the same areas as mine. I'm 19 years old, male but my skin is a complete red mass whereas yours seems to have small white areas around your redness. I'm in two minds as to whether I have Rosacea or Seborrheic dermatitis. My face is cold from 2am to 6am, feels normal no tingling, or heat, cold & normal. I believe that's due to the body temperature decreasing naturally at that time. Worst is 6pm to 11pm. Do you feel the same? I also don't sweat on my face anymore :? Joe."
 Scully55 had skin sensitivity for shampoo after all: "Hi, I was diagnosed with Rosacea many years ago and lived with it for a
long time believing my doctor even though he did nothing other than ask
me a few questions and peek at my skin from 4 feet away. No blood tests,
nothing like that. I was in and out of his office in less then three
minutes. It took him longer to write up the prescriptions than it did to
discuss the symptoms with me. I had previously been diagnosed with
having a rash from shaving but when a years worth of treatment for that
failed I consulted another doctor as I was a little suspicious of his
diagnosis since I had the rash all over my forehead as well as large
areas of my cheeks. After a years worth of expensive treatments for
rosacea I learned from a coworker that some soaps and shampoos can cause
long term rashes. After learning this, I went home and read all the
labels on my soap packaging and on my shampoo bottle. It turns out that I
was using a medicated dandruff shampoo that was not intended for daily
use. I was using it every day and sometimes twice a day. It was only
supposed to be used two or three times a week when dandruff was visible
and only monthly if no dandruff was visible as a preventative
measure.and the disclaimer on the label specifically warned of the
possibility of a rash occuring and expressed the need to stop using the
product immediately if a rash did appear and to consult a doctor if the
rash persisted. I should have consulted that label before I consulted
two or three dermatologist as well as my general practitioner. The rash
went away 100% within two weeks and never came back or at least has not
reappeared for 15 years. I lived with it for at least three or four
years. I highly recommend that all of you who have been diagnosed with
Rosacea but have not been tested for it check your hair care and skin
care products as well as consult a good doctor. [...] I had very similar rashes that I lived with for many years that were so
severe I stopped going out with friends on the weekends and avoided
social contact with anyone but my closest friends because I was tired of
the "What's wrong with your face?" comments and having people say
EEEEEEIIIIIIIIIWWWWW. After years of misdiagnosis from two or three
"specialists" I finally did what a coworker suggested. I read all the
labels on my bath soap packaging and on my hair care products. It turns
out I was using a heavily medicated dandruff shampoo loaded with "tar"
that was only supposed to be used a few times a week when dandruff
appeared and once or twice a month when dandruff was not visible, as a
preventative measure. I was using it daily and sometimes twice a day for
years. When I stopped using the shampoo, my face cleared up 100% within
a few weeks and never came back."
Scully55 had skin sensitivity for shampoo after all: "Hi, I was diagnosed with Rosacea many years ago and lived with it for a
long time believing my doctor even though he did nothing other than ask
me a few questions and peek at my skin from 4 feet away. No blood tests,
nothing like that. I was in and out of his office in less then three
minutes. It took him longer to write up the prescriptions than it did to
discuss the symptoms with me. I had previously been diagnosed with
having a rash from shaving but when a years worth of treatment for that
failed I consulted another doctor as I was a little suspicious of his
diagnosis since I had the rash all over my forehead as well as large
areas of my cheeks. After a years worth of expensive treatments for
rosacea I learned from a coworker that some soaps and shampoos can cause
long term rashes. After learning this, I went home and read all the
labels on my soap packaging and on my shampoo bottle. It turns out that I
was using a medicated dandruff shampoo that was not intended for daily
use. I was using it every day and sometimes twice a day. It was only
supposed to be used two or three times a week when dandruff was visible
and only monthly if no dandruff was visible as a preventative
measure.and the disclaimer on the label specifically warned of the
possibility of a rash occuring and expressed the need to stop using the
product immediately if a rash did appear and to consult a doctor if the
rash persisted. I should have consulted that label before I consulted
two or three dermatologist as well as my general practitioner. The rash
went away 100% within two weeks and never came back or at least has not
reappeared for 15 years. I lived with it for at least three or four
years. I highly recommend that all of you who have been diagnosed with
Rosacea but have not been tested for it check your hair care and skin
care products as well as consult a good doctor. [...] I had very similar rashes that I lived with for many years that were so
severe I stopped going out with friends on the weekends and avoided
social contact with anyone but my closest friends because I was tired of
the "What's wrong with your face?" comments and having people say
EEEEEEIIIIIIIIIWWWWW. After years of misdiagnosis from two or three
"specialists" I finally did what a coworker suggested. I read all the
labels on my bath soap packaging and on my hair care products. It turns
out I was using a heavily medicated dandruff shampoo loaded with "tar"
that was only supposed to be used a few times a week when dandruff
appeared and once or twice a month when dandruff was not visible, as a
preventative measure. I was using it daily and sometimes twice a day for
years. When I stopped using the shampoo, my face cleared up 100% within
a few weeks and never came back." Some people seem to think that we are all made up in a different way and what works for one may not work for another. I don't agree with this. I think that what works for one but doesn't work for another means that these two individuals have two different conditions. But having all of us bundled here together, is that a help or a hindrance? This would be just a guess, but I believe that this site is full of people with facial tinea infections, dermatitis herpeticum, perioral bacterial infections, perioral fungal infections, candida induced facial dermatitis and rosaceiform and many other conditions of which the morphology has changed from use of steroids or topical immunomodulators. Every now and then there is a rave over something and we all jump on the bandwagon, hoping that this will cure us. But so many here don't know what they got, or have been misdiagnosed or self diagnosed or they put up pictures and we try to guess what they have. If this is the only way that it can work, then I think that a lot of people will suffer for a long time here. Well I can argue with that. I think that the first thing that people
should learn when coming here is to educate themselves on the tests that
they should carry out if conventional methods of treatment are not
working. They should insist on a skin biopsy and scrape test and be tested
for food intolerances and food allergies and whatever else. Every derm
has access to a microbiologist, but it's up to us to make sure that they
test us properly and insist on it. It's almost impossible for a mechanic
to know what's wrong with my car by looking under the bonnet(hood) and I
think the same applies to dermatology. There is too much guessing. Look
for instance at seb derm. This, like rosacea, is chronic but it's
irrefutable that this condition can be controlled by certain topical
antifungals. By eliminating the malassezia you will see a marked
improvement in this condition and this is a fact for all of us that
suffer this. If you don't then you don't have seb derm. But I would bet that
there are people here who are taking antibiotics and using topical
metronidazole to treat this fungal infection. And similar tinea
infections. All they are doing is adding to their woes and the
confusion. Now I know that these tests can be costly, but so can visiting
10 different derms and getting different diagnoses along the way. Some
people can feel quite inhibited when visiting a derm, especially when
you're young and inhibited. So I think a list of derms that carry out these
tests on request and without dispute should be compiled. Every
country, every state and every province. People should know exactly where
to go in every corner of the rosacea world. They should know exactly what
tests need to be carried out to find the rosacea mimics. In my opinion, rosacea is one of a handful of conditions that is caused by over
sensitive skin. It can be congenital or self induced. Diet can help to
reduce inflammation and symptoms, but is not a cure. For those who have
been totally cured by diet, I will say it again. You don't and never
did have rosacea. Of course this is just my opinion. I respect your
opinions Bumpy (but now clear) face and I admire you for staying on here
and helping others that have your condition, even though you have cured
yours. But it would be a whole lot easier if you had the proper name for
this. In my humble opinion I would guess at a form of dermatitis
herpeticum. But let's do away with the guesswork."
Some people seem to think that we are all made up in a different way and what works for one may not work for another. I don't agree with this. I think that what works for one but doesn't work for another means that these two individuals have two different conditions. But having all of us bundled here together, is that a help or a hindrance? This would be just a guess, but I believe that this site is full of people with facial tinea infections, dermatitis herpeticum, perioral bacterial infections, perioral fungal infections, candida induced facial dermatitis and rosaceiform and many other conditions of which the morphology has changed from use of steroids or topical immunomodulators. Every now and then there is a rave over something and we all jump on the bandwagon, hoping that this will cure us. But so many here don't know what they got, or have been misdiagnosed or self diagnosed or they put up pictures and we try to guess what they have. If this is the only way that it can work, then I think that a lot of people will suffer for a long time here. Well I can argue with that. I think that the first thing that people
should learn when coming here is to educate themselves on the tests that
they should carry out if conventional methods of treatment are not
working. They should insist on a skin biopsy and scrape test and be tested
for food intolerances and food allergies and whatever else. Every derm
has access to a microbiologist, but it's up to us to make sure that they
test us properly and insist on it. It's almost impossible for a mechanic
to know what's wrong with my car by looking under the bonnet(hood) and I
think the same applies to dermatology. There is too much guessing. Look
for instance at seb derm. This, like rosacea, is chronic but it's
irrefutable that this condition can be controlled by certain topical
antifungals. By eliminating the malassezia you will see a marked
improvement in this condition and this is a fact for all of us that
suffer this. If you don't then you don't have seb derm. But I would bet that
there are people here who are taking antibiotics and using topical
metronidazole to treat this fungal infection. And similar tinea
infections. All they are doing is adding to their woes and the
confusion. Now I know that these tests can be costly, but so can visiting
10 different derms and getting different diagnoses along the way. Some
people can feel quite inhibited when visiting a derm, especially when
you're young and inhibited. So I think a list of derms that carry out these
tests on request and without dispute should be compiled. Every
country, every state and every province. People should know exactly where
to go in every corner of the rosacea world. They should know exactly what
tests need to be carried out to find the rosacea mimics. In my opinion, rosacea is one of a handful of conditions that is caused by over
sensitive skin. It can be congenital or self induced. Diet can help to
reduce inflammation and symptoms, but is not a cure. For those who have
been totally cured by diet, I will say it again. You don't and never
did have rosacea. Of course this is just my opinion. I respect your
opinions Bumpy (but now clear) face and I admire you for staying on here
and helping others that have your condition, even though you have cured
yours. But it would be a whole lot easier if you had the proper name for
this. In my humble opinion I would guess at a form of dermatitis
herpeticum. But let's do away with the guesswork." Redfacegirl wrote: "I hate that doctors really don't understand rosacea. I have seen two
derms and both of them told me food does not matter and kept giving me
different creams that never worked. Food does matter for me so much, and I
wish I knew that months ago. I'm 15 and they look at me like I'm crazy
but I know so much more than they do about rosacea and I have only had
rosacea and seb derm for about a year. And for most of that time, nobody
even believed there was anything wrong with me. Also, many doctors I've
been to are so rude to me, unless you have this then you can not
understand. If I met someone with rosacea or any skin disorder before
this happened, I would NEVER understand or pretend that I know more then
the person who has it does. Haha sorry needed to vent."
Redfacegirl wrote: "I hate that doctors really don't understand rosacea. I have seen two
derms and both of them told me food does not matter and kept giving me
different creams that never worked. Food does matter for me so much, and I
wish I knew that months ago. I'm 15 and they look at me like I'm crazy
but I know so much more than they do about rosacea and I have only had
rosacea and seb derm for about a year. And for most of that time, nobody
even believed there was anything wrong with me. Also, many doctors I've
been to are so rude to me, unless you have this then you can not
understand. If I met someone with rosacea or any skin disorder before
this happened, I would NEVER understand or pretend that I know more then
the person who has it does. Haha sorry needed to vent."
Tom Busby replied: "Sorry to hear about your difficulties. I think that derms have too
little education or training about immune responses to anything,
including food, so their only reaction is to look at the patient like he
or she is crazy. Along the same line of thinking, I asked a friend of
mine with a Masters in Nursing degree why dermatologists seemed so
incompetent. She said that derms usually appeared to be the dumbest
doctors and immunologists always appeared to be the smartest. A
wisecrack, but apropos. I don't have rosacea but I'm certainly sympathetic to your condition,
and I so often see similar posts about rosacea and food triggers, I'm
curious if anyone with rosacea has ever had a chance to see an
immunologist instead of a dermatologist. I've never seen a post
stating, "My immunologist says.."
Mistica replied: "I have heard the same thing many times. A professor mentor of mine who
spent years teaching medical students, thinks of many derms as amateur
doctors. Sounds insulting, but well, it would appear that many here have
various stories to tell which support that observation. Alas. In addition, my old derm who I had in teenage years has kept in touch
with me even though I am now in a different country. He is a dear, kind
man and I respect him even though he can not help me. He has said that
derms don't have a very good understanding of internal medicine, which
is quite an admission! I have been seen by immunologists. I have some abnormalities. I lack CD8
positive lymphocytes. It is a minor deficiency. There are a few other
minor things. I also have intermittent low white counts. Usually lymphocytes and neutrophils. The
CD 8 play a role in resolving inflammation. Many of these are made
in the gut, so there is another clue highlighting the gut connection. In
my case, I have also had elevated levels of ACE. I'd be very
interested to hear who else has had that particular test? It is not one
that is commonly performed, and while indicative of inflammation, it is
usually linked to more sinister diseases. My ACE levels dropped within
range after a couple of months on the GAPS diet. Nat (she has posted about her immune assay, so I am not breaking a
confidence), has also had full immune assays, and some of her results
are the opposite to mine. Yet, we are both severe flushers and have
similar physical issues."
Sources:
http://rosacea-support.org/red-face-when-flushing-isnt-rosacea.html
http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/endocrinology/flushing/
http://site2012.sbd-sp.org.br/public/img/destaques/destaque06.pdf
http://en.diagnosispro.com/differential_diagnosis-for/facial-malar-flush-rash/33343-154.html
http://www.rosaceagroup.org/The_Rosacea_Forum/showthread.php?11993-When-a-red-face-isn-t-rosacea-is-everyones-doctor-checking
http://www.rosaceagroup.org/The_Rosacea_Forum/showthread.php?18568-Its-2009-stop-calling-facial-flushing-and-burning-rosacea!/page3
http://www.rosacea.org/weblog/lupus-or-rosacea-test-may-mislead
http://www.lupus.org/answers/entry/lupus-tests
http://www.internationalrosaceafoundation.org/symptoms.php
http://www.stopthethyroidmadness.com/celiac/
http://www.reverta.com/blog/rosacea/rosacea-and-gluten/
http://www.erythromelalgia.org/WhatisEM.aspx
http://users.telenet.be/zeldzame.ziekten/Getuig/Get.Erythromelalgia.htm
http://www.webmd.com/cancer/features/what-is-carcinoid-syndrome
http://www.patient.co.uk/doctor/carcinoid-tumours
http://www.livingwitherythromelalgia.org/photo/182?context=latest
https://www.mdguidelines.com/polycythemia-vera
http://www.healthboards.com/boards/rosacea/707625-some-questions-polythemia-vera-sp-3.html
http://www.medicinenet.com/mixed_connective_tissue_disease/article.htm
http://www.the-dermatologist.com/article/3004
http://www.medhelp.org/posts/Thyroid-Disorders/shoulder-pain-and-flushing-sensation-with-hypothyroid/show/1142746
http://www.healthboards.com/boards/thyroid-disorders/292367-red-flushed-hot-face-thyroid.html
http://www.thyroid.org.au/Information/disorders.html
http://www.nlm.nih.gov/medlineplus/ency/article/000356.htm
http://www.healthline.com/health/photosensitivity#Types
http://dermnetnz.org/reactions/photosensitivity.html
http://en.wikipedia.org/wiki/Photosensitivity
http://en.wikipedia.org/wiki/Postural_orthostatic_tachycardia_syndrome
http://photographingpots.wordpress.com/tag/autonomic-dysfunction/
http://www.patient.co.uk/health/postural-orthostatic-tachycardia-syndrome
http://hyper.ahajournals.org/content/45/3/385.full
http://www.wisegeek.com/what-is-harlequin-syndrome.htm
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3699916/
http://www.parotid.net/freys-syndrome-treatment-surgery.php
http://www.sweathelp.org/en/where-do-you-sweat/other-sweating/gustatory-sweating.html
http://www.healio.com/endocrinology/news/print/endocrine-today/%7B6c614ea4-a89d-40d6-899c-852a148b3fde%7D/mamas-boy-has-hypogonadism
http://www.expertconsultbook.com/expertconsult/op/book.do?method=display&type=bookPage&decorator=none&eid=4-u1.0-B978-1-4160-4096-5..50054-X--cesec25&isbn=978-1-4160-4096-5
http://www.ncbi.nlm.nih.gov/pubmed/8945484
http://www.mayoclinic.org/diseases-conditions/pheochromocytoma/basics/definition/con-20030435
www.medlink.com/medlinkcontent.asp
http://en.wikipedia.org/wiki/Brunner_syndrome
http://www.raynauds.org/support/forums/forum/messageview.cfm?catid=10&threadid=3327
https://www.rosacea.org/rr/1996/summer/article_1.php
http://rosacea-support.org/red-face-when-flushing-isnt-rosacea.html
http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/endocrinology/flushing/
http://site2012.sbd-sp.org.br/public/img/destaques/destaque06.pdf
http://en.diagnosispro.com/differential_diagnosis-for/facial-malar-flush-rash/33343-154.html
http://www.rosaceagroup.org/The_Rosacea_Forum/showthread.php?11993-When-a-red-face-isn-t-rosacea-is-everyones-doctor-checking
http://www.rosaceagroup.org/The_Rosacea_Forum/showthread.php?18568-Its-2009-stop-calling-facial-flushing-and-burning-rosacea!/page3
http://www.rosacea.org/weblog/lupus-or-rosacea-test-may-mislead
http://www.lupus.org/answers/entry/lupus-tests
http://www.internationalrosaceafoundation.org/symptoms.php
http://www.stopthethyroidmadness.com/celiac/
http://www.reverta.com/blog/rosacea/rosacea-and-gluten/
http://www.erythromelalgia.org/WhatisEM.aspx
http://users.telenet.be/zeldzame.ziekten/Getuig/Get.Erythromelalgia.htm
http://www.webmd.com/cancer/features/what-is-carcinoid-syndrome
http://www.patient.co.uk/doctor/carcinoid-tumours
http://www.livingwitherythromelalgia.org/photo/182?context=latest
https://www.mdguidelines.com/polycythemia-vera
http://www.healthboards.com/boards/rosacea/707625-some-questions-polythemia-vera-sp-3.html
http://www.medicinenet.com/mixed_connective_tissue_disease/article.htm
http://www.the-dermatologist.com/article/3004
http://www.medhelp.org/posts/Thyroid-Disorders/shoulder-pain-and-flushing-sensation-with-hypothyroid/show/1142746
http://www.healthboards.com/boards/thyroid-disorders/292367-red-flushed-hot-face-thyroid.html
http://www.thyroid.org.au/Information/disorders.html
http://www.nlm.nih.gov/medlineplus/ency/article/000356.htm
http://www.healthline.com/health/photosensitivity#Types
http://dermnetnz.org/reactions/photosensitivity.html
http://en.wikipedia.org/wiki/Photosensitivity
http://en.wikipedia.org/wiki/Postural_orthostatic_tachycardia_syndrome
http://photographingpots.wordpress.com/tag/autonomic-dysfunction/
http://www.patient.co.uk/health/postural-orthostatic-tachycardia-syndrome
http://hyper.ahajournals.org/content/45/3/385.full
http://www.wisegeek.com/what-is-harlequin-syndrome.htm
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3699916/
http://www.parotid.net/freys-syndrome-treatment-surgery.php
http://www.sweathelp.org/en/where-do-you-sweat/other-sweating/gustatory-sweating.html
http://www.healio.com/endocrinology/news/print/endocrine-today/%7B6c614ea4-a89d-40d6-899c-852a148b3fde%7D/mamas-boy-has-hypogonadism
http://www.expertconsultbook.com/expertconsult/op/book.do?method=display&type=bookPage&decorator=none&eid=4-u1.0-B978-1-4160-4096-5..50054-X--cesec25&isbn=978-1-4160-4096-5
http://www.ncbi.nlm.nih.gov/pubmed/8945484
http://www.mayoclinic.org/diseases-conditions/pheochromocytoma/basics/definition/con-20030435
www.medlink.com/medlinkcontent.asp
http://en.wikipedia.org/wiki/Brunner_syndrome
http://www.raynauds.org/support/forums/forum/messageview.cfm?catid=10&threadid=3327
https://www.rosacea.org/rr/1996/summer/article_1.php




































































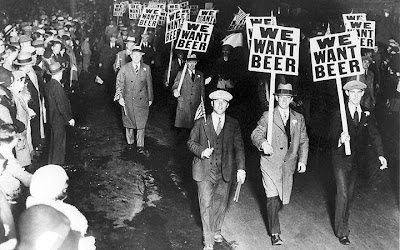


































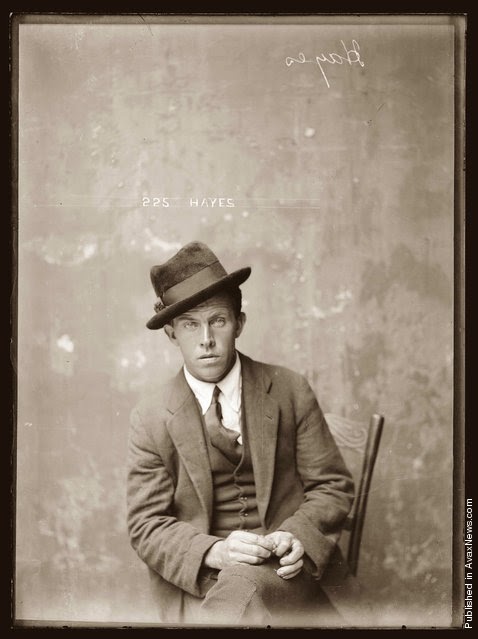













































































Thank you for taking the time to work all this out. it seems like a big job. I feel it is so helpful, as you combine this scientific approach with personal first hand experience and offer rosacea sufferers practical information and tips to work with. Very thorough work and its good reading something that surpasses the usual blog information How someone was miraculously cured with X/Y/Z. hope this helps people determine where their flushing might come from. Thank you!
ReplyDelete